Hepatocarcinoma with metastasis to the anterior mediastinum
Rogério Camargo Pinheiro Alves, Lorena Sagrilo Auer, Lisa Rodrigues da Cunha Saud, Raquel Coris Arrelaro, Aline Carboni Casado, Bruno Gustavo Ferreira, Denis Szjenfeld, Paula Bechara Poletti
1Department of Hepatology, Instituto de Assistência Médica ao Servidor Público Estadual, 04028-000 São Paulo, Brazil
2Department of Gastroenterology, Instituto de Assistência Médica ao Servidor Público Estadual, 04028-000 São Paulo, Brazil
3Department of Radiology, Instituto de Assistência Médica ao Servidor Público Estadual, 04028-000 São Paulo, Brazil
Hepatocarcinoma with metastasis to the anterior mediastinum
Rogério Camargo Pinheiro Alves1, Lorena Sagrilo Auer2, Lisa Rodrigues da Cunha Saud2, Raquel Coris Arrelaro2, Aline Carboni Casado2, Bruno Gustavo Ferreira2, Denis Szjenfeld3, Paula Bechara Poletti2
1Department of Hepatology, Instituto de Assistência Médica ao Servidor Público Estadual, 04028-000 São Paulo, Brazil
2Department of Gastroenterology, Instituto de Assistência Médica ao Servidor Público Estadual, 04028-000 São Paulo, Brazil
3Department of Radiology, Instituto de Assistência Médica ao Servidor Público Estadual, 04028-000 São Paulo, Brazil
Alves et al. Hepatoma Res 2016;2:293-6
Article history:
Received: 22-01-2016
Accepted: 13-10-2016
Published: 21-10-2016
Hepatocellular carcinoma, mediastinal metastasis, sorafenib, computed tomography
Liver malignancies are the sixth leading cause of cancer worldwide, whereas hepatocellular carcinoma (HCC) is the most frequent histological type of liver cancer. Extrahepatic metastasis, which rarely involves the mediastinum, is associated with poor prognosis. An 80-year-old male presenting with mild diffuse abdominal pain for 4 months, associated with hyporexia, increased abdominal volume, dry cough, and loss of 4 kg in 1 month, sought medical assistance due to hemoptysis and chest pain. Tomographic study revealed HCC with mediastinal metastasis, after which sorafenib therapy was started. Disease progressed to death 4 months after the start of the treatment.
INTRODUCTION
Hepatocellular carcinoma (HCC) has high incidence and mortality rates, being the most common primary liver cancer[1]and the third leading cause of cancer mortality. It usually starts with a solitary encapsulated lesion that often shows slow growth and is asymptomatic for a long time.[2]HCC is usually associated with liver cirrhosis, which may impair treatment tolerability and thus increase the risk of complications in cases of advanced cirrhosis. Although there are great differences in the global incidence and frequency of coexisting HCC and cirrhosis that vary according to ethnicity, the coexistence of these two conditions has the same basic clinical characteristics and leads to poor prognosis, regardless of race and location.[2]
Liver cirrhosis of any etiology and chronic infection by hepatitis B are the main risk factors for the development of HCC. All patients with these two conditions benefit from biannual screening for HCC with abdominal ultrasound and measurement of alphafetoprotein (AFP) levels, although the latter has been shown to have questionable efficacy in population surveillance.[3,4]
Non-invasive diagnosis is made by imaging techniques, such as computed tomography and/ or magnetic resonance imaging,[4]based on the vascular findings for these tumors, which exhibit a hypervascular pattern during the arterial phase and a washout pattern during the portal venous or delayed phase. Such radiological characteristic occurs in a small number of 1-2 cm tumors. In these cases, biopsy and tissue biomarkers, such as AFP, are used to confirm the diagnosis. Disease staging should be established at this point, in order to plan treatment and assess prognosis.[3,4]
The most frequent location of metastatic HCC is the lungs, due to possible hematogenous dissemination through their capillary network, followed by bones and abdominal lymph nodes. Conversely, mediastinal metastasis is an uncommon manifestation of HCC and shows poor prognosis.[5,6]We present a case of an elderly patient admitted to our institution after being diagnosed with HCC and mediastinal metastasis.
CASE REPORT
This is the case report of an 80-year-old retired widower coming from São Paulo, southeastern Brazil. His past medical history included high blood pressure, dyslipidemia, diabetes mellitus, benign prostatic hypertrophy, and osteopenia. He was a former smoker of 90 packs a year and denied alcohol abuse. Four months before admission, the patient started to present with mild diffuse abdominal pain, hyporexia, increased abdominal volume, dry cough, anterior chest pain, and loss of 4 kg in the last mouth. He sought medical assistance after two episodes of hemoptysis.
A tomographic study revealed a contrast-enhanced expansive heterogeneous mass measuring 9.7 cm × 5.1 cm × 5.6 cm at this largest diameter and located on the left midline of the anterior mediastinum, with no clear interface between mediastinum and pericardium. No mediastinal lymphadenomegaly was detected. There were hepatic lesions showing a washout pattern in segments V, VI, VII, VIII and IV and protruding toward the hepatic hilum. Evidence of splenic vein thrombus was found [Figure 1].
Laboratory findings were as follows: hemoglobin = 10.5 g/dL; hematocrit = 34%; leukocytes = 7,500.000/mm3(segmented: 64%, band cells: 0%, lymphocytes: 28%, eosinophils: 5%, monocytes: 3%, basophils: 1%); total bilirubin = 0.7 mg/dL; alanine aminotransferase = 48 U/L; aspartate aminotransferase = 40 U/L; AFP = 14,000 ng/mL; gamma-glutamyl transferase = 350 U/L; alkaline phosphatase = 148 U/L; international normalized ratio = 1.75; creatinine = 0.77 mg/dL.

Figure 1:Axial contrast-enhanced computed tomography slices at arterial (A) and portal (B) phases. Note tumor infiltration (arrow) extending from part of the right hepatic lobe to the hilar region and tumor infiltration of the portal vein (arrow head)

Figure 2:Axial contrast-enhanced computed tomography (CT) slice (A) and coronal reconstruction of CT scan (B). Note large heterogeneous hypervascular anterior mediastinal mass (arrow) posteriorly compressing the right atrium and pulmonary artery
The patient and his family decided to start sorafenib therapy, and he did not want to undergo invasive procedures, such as chemoembolization, for the treatment of mediastinal metastasis. Drug therapy was maintained for 3 months, when the patient was readmitted due to clinical worsening, with the development of jaundice and severe ascites. Patient staging was reassessed, showing evidence of growth of the mediastinal mass, which measured 11.0 cm × 6.3 cm × 7.7 cm at that time and was compressing the right atrium and the pulmonary artery [Figure 2]. There was also an increase in the size of hepatic solid lesions and in the extension of thrombosis. AFP levels reached 45,000 ng/mL. It was decided to discontinue chemotherapy with sorafenib, and the patient died 1 month after readmission.
DISCUSSION
HCC is one of the most common primary tumors worldwide, and its prognosis has improved over the past few decades with the assessment of tumor vascular pattern by imaging methods and the emergence of therapeutic procedures. A considerable amount of literature has been published on the different presentations of HCC and on extrahepatic metastases, which occur in 30-50% of HCC cases. The most common metastatic sites are lungs, bones,and loco-regional lymph nodes, presenting commonly with dyspnea and bone pain.[7]A study in autopsy files showed that unusual extrahepatic metastatic sites include diaphragm, pancreas, gall bladder, stomach, colon, adrenal gland, pleura, peritoneum, cervical lymph nodes, brain, skin, and oral cavity.[8]
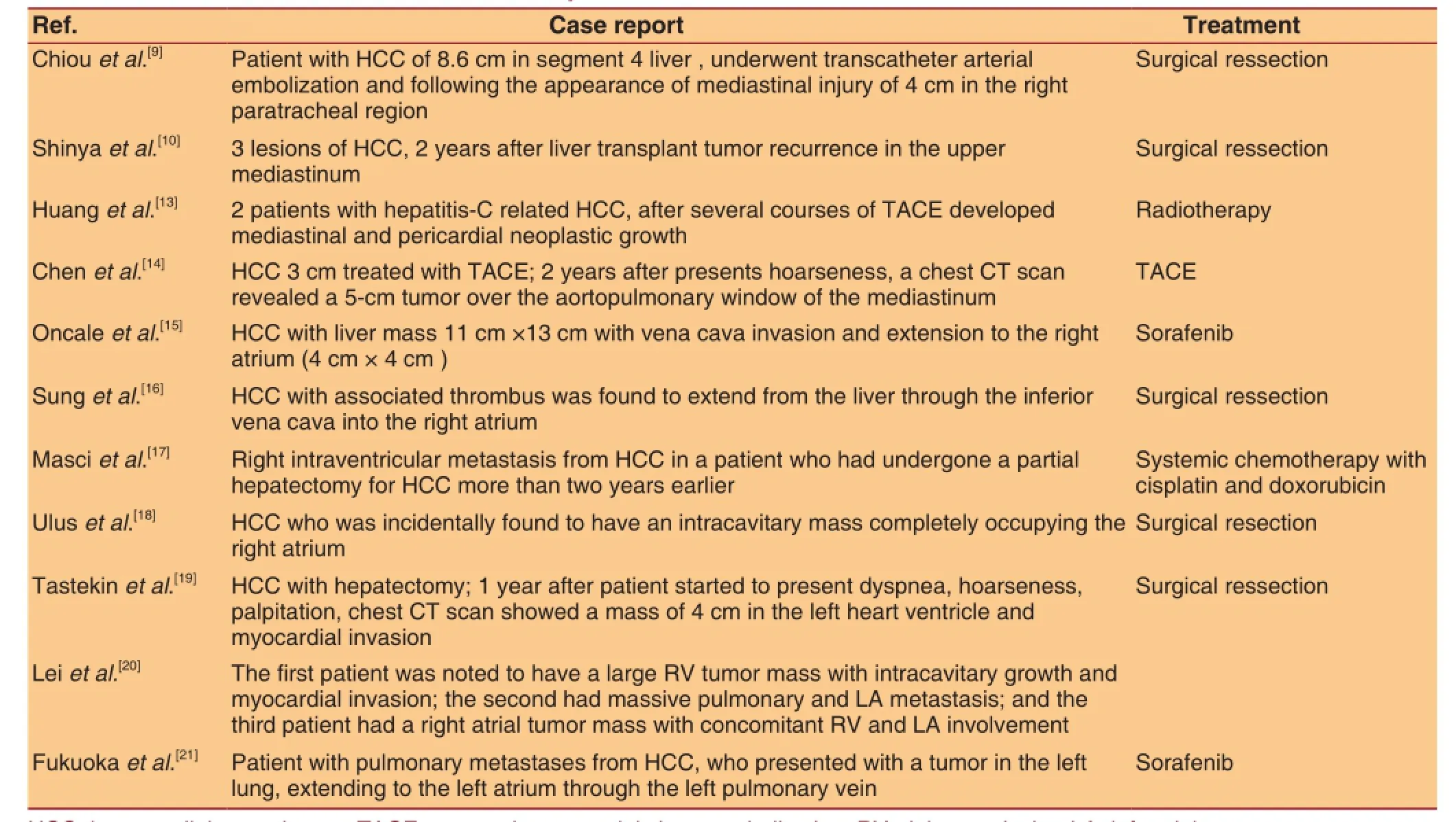
Table 1: Cases of mediastinal metastases reported in the literature
It is important to emphasize that the diagnosis of our patient was based on the presence of mediastinal mass and hepatic lesions. We decided not to perform liver biopsy because an imaging study revealed that the tumor had a washout vascular pattern and the patient showed AFP levels of 14,000 ng/mL.
The involvement of mediastinal lymph nodes occurs in 4% to 5% of the cases of HCC. In patients with mediastinal metastasis, lesions were mostly diagnosed simultaneously with the viable intrahepatic tumor.[9]Mediastinal metastases are unusual, and mediastinal involvement usually leads to dissemination to lymph nodes, which occurs by three routes of hepatic lymphatic drainage. The first route is from the left hepatic lobe via anterior phrenic lymph nodes to the parasternal or subcarinal lymph nodes; the second, from the liver through the hepatic falciform ligament to the parasternal or paratracheal lymph nodes; and the third, from the right hepatic lobe through the right triangular ligament to the paratracheal lymph nodes.[9,10]
The predictors of the presence of extrahepatic metastases are: size and number of HCC nodules, presence of tumor vascular invasion or tumor biomarkers.[2]
Patients with initial HCC, i.e. with no distant metastases, may undergo partial liver resection, which is potentially curative, as well as liver transplantation or percutaneous ablation. More advanced cases, such as the one presented in this study, are eligible to palliative treatment with sorafenib.[4]However, research has shown that treatment of intrahepatic lesions should not be contraindicated in the presence of extrahepatic metastasis. Moreover, radical treatments for extrahepatic metastases should be considered when hepatic lesions are under reasonable control or if metastasis is accompanied by severe symptoms.[11,12]In the case of mediastinal metastasis, transarterial chemoembolization has shown good response and adequate symptom control, in addition to increasing survival.[13,14]In Table 1, we detail HCC cases of mediastinal metastases reported in the literature.
The present study showed that, despite therapeutic advances and the use of target therapy, survival is very limited when tumor is advanced, diagnosis is made at a later stage, and there are distant metastases.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
Patient consent
Consent form was obtained from the patient family.
Ethics approval
The study was approved by the Institutional Review Board of IAMSPE.
1. Vilana R, Forner A, Garcia A, Ayuso C, Bru C. Hepatocellular carcinoma: diagnosis, staging, and treatment strategy.Radiologia2010;52:385-98. (in Spanish)
2. Okuda K, Ohtsuki T, Obata H, Tomimatsu M, Okazaki N, Hasegawa H, Nakajima Y, Ohnishi K. Natural history of hepatocellular carcinoma and prognosis in relation to treatment. Study of 850 patients.Cancer1985;56:918-28.
3. Achkar JP, Araya V, Baron RL, Marsh JW, Dvorchik I, Rakela J. Undetected hepatocellular carcinoma: clinical features and outcome after liver transplantation.Liver Transpl Surg1998;4:477-82.
4. European Association for the Study of the Liver; European Organization for Research and Treatment of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma.J Hepatol2012;56:908-43.
5. Kanda M, Tateishi R, Yoshida H, Sato T, Masuzaki R, Ohki T, Imamura J, Goto T, Yoshida H, Hamamura K, Obi S, Kanai F, Shiina S, Omata M. Extrahepatic metastasis of hepatocellular carcinoma: incidence and risk factors.Liver Int2008;28:1256-63.
6. Katyal S, Oliver JH 3rd, Peterson MS, Ferris JV, Carr BS, Baron RL. Extrahepatic metastases of hepatocellular carcinoma.Radiology2000;216:698-703.
7. Uka K, Aikata H, Takaki S, Shirakawa H, Jeong SC, Yamashina K, Hiramatsu A, Kodama H, Takahashi S, Chayama K. Clinical features and prognosis of patients with extrahepatic metastases from hepatocellular carcinoma.World J Gastroenterol2007;13:414-20.
8. Terada T, Maruo H. Unusual extrahepatic metastatic sites from hepatocellular carcinoma.Int J Clin Exp Pathol2013;6:816-20.
9. Chiou SR, Lin TL, Bora D, Lu HI, Chen CL, Wang SH, Lin CC, Liu YW, Yong CC, Li WF, Liu CY, Wang CC. Metastatic hepatocellular carcinoma mimicking a solitary mediastinal tumor.J Cancer Res Pract2010;26:257-62.
10. Shinya S, Noritomi T, Yamauchi Y, Sasaki T, Hamada Y, Yamashita Y. Two rare metachronous metastases of hepatocellular carcinoma after liver transplantation.Int Surg2013;98:432-6.
11. Uchino K, Tateishi R, Shiina S, Kanda M, Masuzaki R, Kondo Y, Goto T, Omata M, Yoshida H, Koike K. Hepatocellular carcinoma with extrahepatic metastasis: clinical features and prognostic factors.Cancer2011;117:4475-83.
12. Shimada M, Takenaka K, Gion T, Fujiwara Y, Kajiyama K, Maeda T, Shirabe K, Nishizaki T, Yanaga K, Sugimachi K. Prognosis of recurrent hepatocellular carcinoma: a 10-year surgical experience in Japan.Gastroenterology1996;111:720-6.
13. Huang CC, Ng WW, Chiang JH, Chen FH, Huang CH, Wang YJ, Chang FY, Lee SD. Hepatocellular carcinoma with mediastinal and pericardial invasion: report of two cases.Zhonghua Yi Xue Za Zhi (Taipei)1999;62:891-5.
14. Chen CC, Yeh HZ, Chang CS, Ko CW, Lien HC, Wu CY, Hung SW. Transarterial embolization of metastatic mediastinal hepatocellular carcinoma.World J Gastroenterol2013;19:3512-6.
15. Oncale M, Lewis B. Hepatocellular carcinoma with extension to the heart via the inferior vena cava.Proc (Bayl Univ Med Cent)2015;28:229-30.
16. Sung AD, Cheng S, Moslehi J, Scully EP, Prior JM, Loscalzo J. Hepatocellular carcinoma with intracavitary cardiac involvement: a case report and review of the literature.Am J Cardiol2008;102:643-5.
17. Masci G, Magagnoli M, Grimaldi A, Covini G, Carnaghi C, Rimassa L, Santoro A. Metastasis of hepatocellular carcinoma to the heart: a case report and review of the literature.Tumori2004;90:345-7.
18. Ulus T, Birdane A, Dündar E, Tünerir B. Asymptomatic course of a metastatic mass completely filling the right atrium in a patient with hepatocellular carcinoma.Turk Kardiyol Dern Ars2012;40:52-4.
19. Tastekin E, Usta U, Ege T, Kazindir G, Kutlu AK. Cardiac metastasis of hepatocellular carcinoma in a young non-cirrhotic patient, to the left ventricle.Ann Hepatol2012;11:392-4.
20. Lei MH, Ko YL, Kuan P, Lien WP, Chen DS. Metastasis of hepatocellular carcinoma to the heart: unusual patterns in three cases with antemortem diagnosis.J Formos Med Assoc1992;91:457-61.
21. Fukuoka K, Masachika E, Honda M, Tsukamoto Y, Nakano T. Isolated metastases of hepatocellular carcinoma in the left atrium, unresponsive to treatment with sorafenib.Mol Clin Oncol2015;3:397-9.
10.20517/2394-5079.2016.01
Dr. Rogério Camargo Pinheiro Alves, Department of Hepatology, Instituto de Assistência Médica ao Servidor Público
Estadual, Av. Ibirapuera, 981, Indianópolis, 04028-000 São Paulo, Brazil. E-mail: rcpalves@uol.com.br
How to cite this article:Alves RCP, Auer LS, da Cunha Saud LR, Arrelaro RC, Casado AC, Ferreira BG, Szjenfeld D, Poletti PB. Hepatocarcinoma with metastasis to the anterior mediastinum. Hepatoma Res 2016;2:293-6.
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
For reprints contact:service@oaepublish.com
- Hepatoma Research的其它文章
- Prof. Shu-Kui Qin, M.D.& Ph.D., Joins HR as Honorary Editor-in-Chief
- Epstein-Barr virus associated secondary hemophagocytic lymphohistiocytosis with an unusual presentation of abdominalcompartment syndrome
- ONGOING SPECIAL ISSUES
- Is transarterial embolization a valuable treatment option for spontaneous rupture of hepatocellular carcinoma: experience from a tertiary care hospital of South-Asia
- GENERAL INFORMATION
- EDITORIAL BOARD