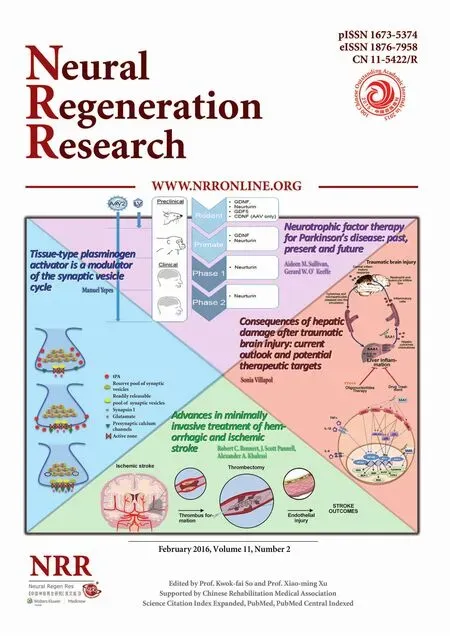
Advances in minimally invasive treatment of hemorrhagic and ischemic stroke
PERSPECTIVE
Advances in minimally invasive treatment of hemorrhagic and ischemic stroke
Cerebrovascular diseases, including ischemic and hemorrhagic strokes, affect more than 6 million US adults annually. Strokes cause high rates of morbidity and mortality due to the central nervous system’s sensitivity to disruptions in blood flow, and are refractory to traditional surgical interventions. A variety of minimally invasive surgical and endovascular approaches have recently been developed to improve patient outcomes following stroke.
Hemorrhagic strokes, also referred to as intracranial hemorrhages (ICH), have clinical outcomes largely dependent on hemorrhage location, size, and secondary peri-hematomal edema (Rennert et al., 2015). In theory, clot evacuation addresses local mass effect and enhances survival of edematous penumbral tissue (Rennert et al., 2015), however, multiple clinical trials have failed to show a definitive benefit for surgical hematoma evacuation following ICH (Rennert et al., 2015). The largest of these is the 2005 International Surgical Trial in Intracerebral Haemorrhage (STICH) trial (Mendelow et al., 2005), wherein 1,033 patients with spontaneous lobar and/or basal ganglia ICH were randomly selected for surgical evacuation within 24 hours of presentation, or initial conservative treatment. In this study there was no significant difference in favorable outcomes across groups (26% vs. 24%, P = 0.4), yet subgroup analysis revealed that patients with superficial hematomas (≤ 1 cm from the cortical surface) may benefit from surgery, supporting the hypothesis that decreasing secondary neurologic injury from manipulation of injured penumbral tissue during clot removal critically affects outcomes. Current guidelines thus recommend consideration of open surgical evacuation only in specific clinical scenarios, such as lobar clots >30 mL and within 1 cm of the cortical surface. In this setting, there has been a recent push to develop minimally invasive approaches for ICH removal.
One such minimally invasive approach is stereotactic surgery (i.e., using an imaging based three dimensional roadmap for surgical localization) combined with intra-clot injection of thrombolytic agents, such as tissue plasminogen activator (tPA). The Minimally Invasive (Stereotactic) Surgery plus rTPA for ICH Evaluation (MISTIE) randomized clinical trials have demonstrated the safety and effectiveness of this approach for reducing clot and perihematomal edema (Rennert et al., 2015), with a larger phase III clinical efficacy trial currently ongoing. Stereotactic endoscopic evacuation of intraventricular hemorrhages (IVH) in ICH is also being explored, as is targeted infusion of intraventricular thrombolytics based on pre-clinical and clinical safety data (Gaberel et al., 2014; Rennert et al., 2015).
Endoscopic techniques (i.e., burr hole craniotomy with direct hematoma visualization/removal through a sheath) are similarly appealing due to minimization of secondary neurologic injury from surgical manipulation. Direct hematoma visualization with this approach also allows for identification and real-time treatment of the original bleeding source, and is associated with improved evacuation rates compared to stereotactic aspiration (Cho et al., 2006). Moreover, this technique may be particularly well suited for deeper hemorrhages, with preliminary data showing improved clot evacuation rates and post-operative neurologic status compared to open surgery in patients with hemorrhage in deeper brain structures such as the putamen and thalamus (Nagasaka et al., 2011).
New technology combining real-time neuronavigation with neuroendoscopy has also been developed and trialed for ICH evacuation (Rennert et al., 2015). The initial multi-center clinical experience with one such system was recently reported, with twenty-nine patients with lobar, basal ganglia, and brainstem hemorrhages (including six with the poor prognostic finding of intraventricular extension) treated with a nearly 92% technical success rate and low morbidity and mortality (Spiotta et al., 2015). While general clinical guidelines for endoscopic ICH evacuation are currently supratentorial hemorrhages ≥ 30 mL, with a goal of <15 mL post-operative residual, combined neuronavigation/neuroendoscopy has already been integrated into the senior author’s clinical practice (Figure 1), and has the potential to expand these indications and gain widespread adaptation for the treatment of ICH as additional clinical data is obtained.
Minimally invasive surgical techniques are also being increasingly utilized in ischemic strokes, where the rapid restoration of normal blood flow via thrombolytics or mechanical thrombectomy is critical. In fact, for large vessel occlusive strokes, multiple large, randomized trials were recently stopped for dramatic outcome improvement with thrombectomy for acute large vessel stroke (Berkhemer et al., 2015; Campbell et al., 2015; Goyal et al., 2015), making this intervention the new standard of care (Powers et al., 2015).
The initial data with mechanical thrombectomy nonetheless demonstrated a decoupling of clinical outcomes with the technical success of angiographic reperfusion (Teng et al., 2015). These findings, combined with the known detrimental effects of disruptions in physiologic blood flow on endothelial cell maintenance, remodeling, and cytokine signaling, support the hypothesis that vascular endothelial cell damage resulting from altered flow dynamics, reperfusion injury, and/or iatrogenic trauma may potentiate secondary neuronal injury in post-thrombectomy stroke patients (Figure 2) (Teng et al., 2015).
To better assess the effect of thrombectomy devices on the endothelium, we recently developed a novel in vitro live cell platform capable of characterizing endothelial injury patterns and mechanisms across thrombectomy devices (Figure 3) (Teng et al., 2015). This technology allowed for the tubular growth of endothelial cells under peristaltic flow, with post-thrombectomy injuries easily visualized and quantified with a novel rotational-scanning image system and three-dimensional reconstruction. Specifically, six thrombectomy devices were tested across three vessel diameters in vitro: (1) 5MAX ACE (Penumbra, Inc., Alameda, CA) with A Direct Aspiration first Pass Technique (ADAPT), (2) MERCI (3.0 firm) (Concentric Medical Inc/Stryker Corp., Kalamazoo, MI), (3) 5MAX with Separator (Penumbra, Inc.), (4) 5MAX with Separator 3D (Penumbra, Inc.), (5) Solitaire FR (4 × 20 mm) (Covidien, Ltd, Mansfield, OH) and (6) TREVO (Stryker Corp.). Characteristic injuries were seen across devices, ranging from a nearly complete degloving injury with the Merci retriever, to a focused circumferential or linear denudation with the 5MAX ACE with the ADAPT technique and the Separator 3D. These findings were surprising by ours (Teng et al., 2015) and others (Gory et al., 2013) data from in vivo experiments, and validate the in vitro live cell model as an important tool for thrombectomy device assessment and future design evaluations.
As research in other surgical fields has demonstrated multiple advantages of minimally invasive techniques, including avoidance of large incisions requiring less sedation, less trauma to the patient, and potentially lower treatment costs resulting from shorter hospital courses and a reduced need for post-operative intensive medical care, it is not surprising that minimally invasive surgical approaches to stroke have recently gained traction. As highlighted herein, the successful development and integration of such technology requires a strong pre-clinical foundation and well designed clinical trials. The promising results in the aforementioned and ongoing clinical trials suggest the future utilization of minimally invasive techniques for the treatment of hemorrhagic and ischemic stroke will continue to increase.
RCR, JSP and AAK contributed to idea generation, paper preparation, and revisions. The authors are grateful to Victor W. Wong for his original figure artwork. AAK has previously received competitive grants from Covidien Ltd. and Penumbra Inc, and holds consulting arrangements for physician training with Stryker Neurovascular, Covidien Ltd., and Penumbra Inc. AAK has no direct financial interests related to this work. RCR and JSP have no disclosures concerning the materials or methods used in this study or the findings specified in this paper.
Robert C. Rennert, J. Scott Pannell, Alexander A. Khalessi*
Department of Neurosurgery, University of California - San Diego, La Jolla, CA, USA
*Correspondence to: Alexander A. Khalessi, MD, MS, FAANS, FAHA, akhalessi@ucsd.edu.
Accepted: 2015-11-19
How to cite this article: Rennert RC, Pannell JS, Khalessi AA (2016) Advances in minimally invasive treatment of hemorrhagic and ischemic stroke. Neural Regen Res 11(2):228-229.

Figure 1 Endoscopic hematoma evacuation.

Figure 2 Schematic illustration of the hypothesis that thrombectomyassociated iatrogenic endothelial cell injury can influence strokeoutcomes.

Figure 3 In vitro live cell model demonstrating the heterogeneous effects of thrombectomy devices on the endothelium.
Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, Schonewille WJ, Vos JA, Nederkoorn PJ, Wermer MJ, van Walderveen MA, Staals J, Hofmeijer J, van Oostayen JA, Lycklama à Nijeholt GJ, Boiten J, Brouwer PA, Emmer BJ, de Bruijn SF, van Dijk LC, et al. (2015) A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 372:11-20.
Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, Yan B, Dowling RJ, Parsons MW, Oxley TJ, Wu TY, Brooks M, Simpson MA, Miteff F, Levi CR, Krause M, Harrington TJ, Faulder KC, Steinfort BS, Priglinger M, et al. (2015) Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 372:1009-1018.
Cho DY, Chen CC, Chang CS, Lee WY, Tso M (2006) Endoscopic surgery for spontaneous basal ganglia hemorrhage: comparing endoscopic surgery, stereotactic aspiration, and craniotomy in noncomatose patients. Surg Neurol 65:547-555.
Gaberel T, Montagne A, Lesept F, Gauberti M, Lemarchand E, Orset C, Goulay R, Bertrand T, Emery E, Vivien D (2014) Urokinase versus Alteplase for intraventricular hemorrhage fibrinolysis. Neuropharmacology 85:158-165.
Gory B, Bresson D, Kessler I, Perrin ML, Guillaudeau A, Durand K, Ponsonnard S, Couquet C, Yardin C, Mounayer C (2013) Histopathologic evaluation of arterial wall response to 5 neurovascular mechanical thrombectomy devices in a swine model. AJNR Am J Neuroradiol 34:2192-2198.
Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, Roy D, Jovin TG, Willinsky RA, Sapkota BL, Dowlatshahi D, Frei DF, Kamal NR, Montanera WJ, Poppe AY, Ryckborst KJ, Silver FL, Shuaib A, Tampieri D, Williams D, et al. (2015) Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 372:1019-1030.
Mendelow AD, Gregson BA, Fernandes HM, Murray GD, Teasdale GM, Hope DT, Karimi A, Shaw MD, Barer DH (2005) Early surgery versus initial conservative treatment in patients with spontaneous supratentorial intracerebral haematomas in the International Surgical Trial in Intracerebral Haemorrhage (STICH): a randomised trial. Lancet 365:387-397.
Nagasaka T, Tsugeno M, Ikeda H, Okamoto T, Inao S, Wakabayashi T (2011) Early recovery and better evacuation rate in neuroendoscopic surgery for spontaneous intracerebral hemorrhage using a multifunctional cannula: preliminary study in comparison with craniotomy. J Stroke Cerebrovasc Dis 20:208-213.
Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC, Johnston KC, Johnston SC, Khalessi AA, Kidwell CS, Meschia JF, Ovbiagele B, Yavagal DR (2015) 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 46:3020-3035.
Rennert RC, Signorelli JW, Abraham P, Pannell JS, Khalessi AA (2015) Minimally invasive treatment of intracerebral hemorrhage. Exp Rev Neurother 15:919-933.
Spiotta AM, Fiorella D, Vargas J, Khalessi A, Hoit D, Arthur A, Lena J, Turk AS, Chaudry MI, Gutman F, Davis R, Chesler DA, Turner RD (2015) Initial multicenter technical experience with the Apollo device for minimally invasive intracerebral hematoma evacuation. Neurosurgery 11 Suppl 2:243-2511.
Teng D, Pannell JS, Rennert RC, Li J, Li YS, Wong VW, Chien S, Khalessi AA (2015) Endothelial trauma from mechanical thrombectomy in acute stroke: in vitro livecell platform with animal validation. Stroke 46:1099-1106.
10.4103/1673-5374.177747 http://www.nrronline.org/
- 中国神经再生研究(英文版)的其它文章
- Tissue-type plasminogen activator is a modulator of the synaptic vesicle cycle
- Impaired consciousness caused by injury of the lower ascending reticular activating system: evaluation by diffusion tensor tractography
- Considering calcium-binding proteins in invertebrates: multi-functional proteins that shape neuronal growth
- Cardiovascular dysfunction following spinal cord injury
- Practical application of the neuroregenerative properties of ketamine: real world treatment experience
- Exergames: neuroplastic hypothesis about cognitive improvement and biological effects on physical function of institutionalized older persons