Neurotrophic factor therapy for Parkinson’s disease: past, present and future
HIGHLIGHTS
Neurotrophic factor therapy for Parkinson’s disease: past, present and future
One of the greatest unmet needs in the treatment of Parkinson’s disease (PD) is a disease-modifying therapy, which can halt the ongoing degeneration of dopaminergic neurons that is characteristic of this disorder. Current therapies focus on managing symptoms, rather than on addressing their cause. Promising candidates for disease-modifying therapies are the dopaminergic neurotrophic factors (NTFs). NTFs are secreted proteins which play critical roles in the developing nervous system, directing and supporting the specification, maturation and survival of specific neuronal populations. Several dopaminergic NTFs have shown great potential in animal models of PD, conferring protective and regenerative effects on the nigrostriatal dopaminergic neurons which undergo progressive degeneration in this disease (for reviews see Sullivan and Toulouse, 2011; Hegarty et al., 2014a).
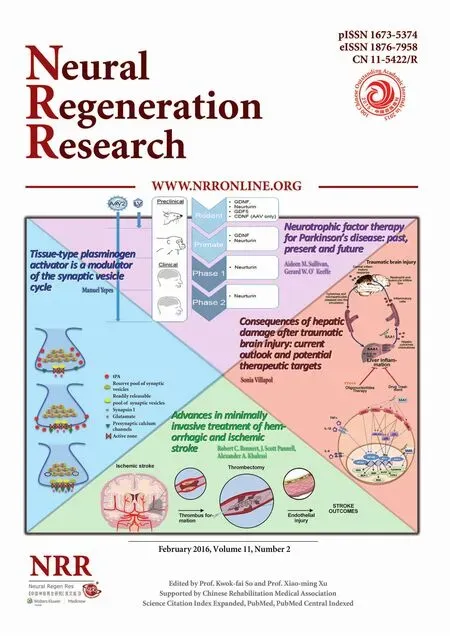
The significant promise of preclinical studies led to clinical trials involving two of these dopaminergic NTFs, glial cell line-derived neurotrophic factor (GDNF) and neurturin (NRTN) (Figure 1). In the initial clinical trials of GDNF, the recombinant protein was injected or infused into the brain. However, this type of delivery is associated with several practical problems, not least of which is the rapid biometabolism of NTF proteins by endogenous enzymes in vivo. Gene therapy can circumvent this issue by incorporating the gene for the therapeutic protein into brain cells, achieving longterm and targeted delivery. This approach has enormous potential for the delivery of NTFs to the degenerating nigrostriatal pathway and its use has led to considerable advancements in the ongoing development of neuroprotective therapies for PD. Recent studies have used recombinant adeno-associated viral (AAV) or lentiviral (LV) vectors to induce over-expression of NTFs in animal models of PD (for recent review see Kelly et al., 2015). This led to clinical testing of viral vector-mediated delivery of NTFs in PD patients, with AAV2 vectors deemed the most safe and appropriate for human use.
GDNF: Although promising results emerged from two open-label trials, which used direct infusion of recombinant human GDNF to the putamen in PD patients (Gill et al., 2003; Slevin et al., 2005), a subsequent placebo-controlled trial showed no significant motor improvements (Lang et al., 2006). Furthermore, safety issues were raised, as some patients developed antibodies towards the exogenous GDNF protein. The discrepancies between the open-label and placebo-controlled trials may have been due to variations in patient selection, as well as to a placebo effect. Another factor may have been poor diffusion of GDNF throughout the caudate-putamen from its infusion site. Delivery of GDNF to the brain using viral vectors may overcome this latter issue. Pre-clinical studies on AAV-mediated delivery of GDNF, and its optimisation via the use of convection-enhanced delivery (CED) (Richardson et al., 2011), led to the development of a protocol which is currently being implemented in an ongoing phase 1 clinical trial for advanced PD (NIH trial No. NCT01621581). A second ongoing clinical trial is one conducted by the Bristol group. In early 2015, they completed patient enrolment for a phase II trial in 42 patients, using a new infusion protocol for GDNF protein delivery, involving CED (UK CRN 12085).
Neurturin (NRTN): Based on promising results from animal studies using AAV2-mediated NRTN gene transfer, Ceregene initiated an open-label clinical trial using this vector in PD patients (Marks et al., 2008). Although this initial trial showed promising symptomatic improvements, a subsequent double-blind phase II trial reported only modest benefits in NRTN-treated patients at the 12-month end-point (Marks et al., 2010). However, some patients displayed significant improvements in some UPDRS subscores after 18 months, implying that there may have been a delayed neurotrophic effect (Marks et al., 2010). Studies on post mortem tissue from participants in that trial showed very limited transport of NRTN from its intraputamenal infusion site to the midbrain, despite strong NRTN expression in the putamen for at least four years. The lack of retrograde transport of NRTN from the intraputamenal injection site to the dopaminergic cell bodies in the SN may have been due to its poor solubility and diffusion properties. These findings of limited transport as well as of a potential delayed neurotrophic effect led Ceregene to investigate new methodologies for optimising AAV2-NRTN delivery.

Figure 1 Summary of the stages of development of each neurotrophic factor in development for Parkinson’s disease therapy.
After extensive preclinical testing, Ceregene initiated clinical trials in which AAV2-NRTN was injected to both striatum and SN, in order to maximise NRTN delivery throughout the degenerating nigrostriatal system. An initial phase I trial in six patients demonstrated the safety of delivering AAV-NRTN bilaterally to both putamen and nigra (Bartus et al., 2013). How-ever, the subsequent double-blind trial conducted in 52 patients did not meet the predetermined end-points in efficacy; there was no significant difference between the UPDRS scores of the NRTN-treated and sham surgery groups (Olanow et al., 2015). Nevertheless, the surgical procedure was well-tolerated, with no significant adverse effects, lending further support to the safety of gene therapy to the brain and furthermore to the targeting of the midbrain in stereotactic delivery of therapeutics.
Downregulation of Ret by alpha-synuclein: In recent years, preclinical studies on a new animal model of PD have yielded some clues regarding the disappointing failures of GDNF and NRTN in clinical trials. In contrast to the successful studies which used GDNF in the 6-OHDA lesion rat models, GDNF delivery by either AAV or LV vectors was not effective in preventing neurodegeneration in the AAV-α-synuclein model (Decressac et al., 2011). In this model, AAV-mediated overexpression of α-synuclein in the adult rat brain induces protracted and progressive degeneration of the nigrostriatal pathway which closely mimics the human disease. Further investigation demonstrated that α-synuclein overexpression downregulates the expression of Nurr1 and its downstream target, the GDNF receptor Ret, in DA neurons of the SN (Decressac et al., 2012). That study also showed that Ret expression was reduced in nigral DA neurons in PD patients (Decressac et al., 2012). Both GDNF and NTRN signal through multicomponent receptors consisting of Ret receptor tyrosine kinase and either of two glycosyl-phosphatidylinositol (GPI)-linked ligand-binding subunits - GFRα1 for GDNF and GFRα2 for NRTN. Thus, downregulation of Ret by α-synuclein may explain the failure of these two NTFs to exert neuroprotective effects in the α-synuclein rat model, and further, could potentially expound their failure in clinical trials.
Conclusions and future perspectives: The use of NTFs has the advantage over existing therapies for PD, since these factors may protect the remaining nigrostriatal dopaminergic neurons from delayed or further damage, rather than only treating the disease symptoms. This is crucial, since by the time that most patients present clinically, approximately 50% of these neurons have degenerated, corresponding to a loss of striatal input of about 80%. Despite extremely promising reports in preclinical models of PD, the clinical application of NTFs has unfortunately not been successful. The recent failure of AAV-NRTN in a phase II trial (Olanow et al., 2015), following disappointing results from similar trials using GDNF, is a large blow to this research field. There is a critical need to decipher the reasons for the failures of GDNF and NRTN in placebo-controlled trials and to develop a focused research strategy, if this therapeutic area is to advance.
One issue arising from the GDNF clinical trials was the detection of neutralising antibodies in some of the participants. It is possible that this antibody production could have been stimulated by the presence of small amounts of bacterial endotoxins in the recombinant protein preparation. The potential adverse and efficacy-limiting consequences of patients developing antibodies to exogenous GDNF protein should be counteracted by the use of gene therapy. A gene therapy approach would not result in GDNF protein entering the peripheral circulation, which must have occurred in the prior clinical trials. Another way around this issue is demonstrated in a recent study which developed an engineered variant of GDNF with lower immunogenicity and improved biodistribution properties (Smith et al., 2015). Both gene therapy and this bioengineering approach could also circumvent the issue of poor stability of recombinant GDNF.
An important point to note from the most recent NRTN clinical trial was that post hoc analysis found that patients who had been diagnosed within 5 years of receiving AAV-NRTN treatment showed significantly greater improvements in UPDRS scores than those who were diagnosed more than ten years before the trial (Olanow et al., 2015). This pattern of greater improvements in patients who are at earlier disease stages has been reported in several previous trials of neuroprotective therapies. Careful consideration of inclusion criteria for future trials is thus warranted. The development of biomarkers for PD is a critically important research area, which will enable identification of patients at early disease stages, who are likely to gain optimal benefit from NTF therapies.
The important finding that alpha-synuclein down-regulates the expression of Ret in dopaminergic neurons shows that the development of dopaminergic NTFs that are Ret-independent is critical. If Ret expression is significantly affected by the pathology of PD, then the use of GDNF and NRTN may never reach the potential which was shown in the early preclinical studies. These early studies employed biochemical models of PD such as 6-OHDA and MPTP, which do not produce alpha-synuclein aggregation as is seen in the human disease. If the machinery needed for GDNF and NRTN to produce their protective effects on dopaminergic neurons is lacking in the PD brain, then these factors may never achieve clinical success, even with optimal delivery methods. Gene delivery of Ret in combination with that of GDNF or NRTN is one approach that may be taken, but the use of other NTFs that are not dependent on Ret must also be explored.
GDNF and NRTN are not the only NTFs which have been investigated in preclinical studies for their potential use in PD. Others which show comparable effects to these include growth/ differentiaion factor 5 (GDF5) and cerebral dopamine neurotrophic factor (CDNF) and its paralogue, mesencephalic astrocyte-derived neurotrophic factor (MANF).
CDNF and MANF both confer neurotrophic and restorative actions on the nigrostriatal pathway. Viral vector-delivered CDNF has been tested successfully in rodents (Back et al., 2013) and combined overexpression of CDNF and MANF in the adult rat SN has recently been reported to have enhanced efficacy (Cordero-Llana et al., 2015). Delivery of MANF to the porcine putamen and striatum using CED showed significant potential for translation of this factor to human studies (Barua et al., 2015). The receptors for CDNF and MANF are still uncharacterised, and little is known about the mechanism of their neurotrophic actions. Further studies on these promising factors are warranted to ascertain their potential in therapeutic applications.
GDF5 is a member of the TGFβ superfamily, but is part of the bone morphogenetic protein (BMP) subfamily, a distinct group from the GDNF subfamily. It has neurotrophic and protective actions on nigrostriatal dopaminergic neurons in vitro and in vivo that are comparable to those of GDNF (for reviews see Hegarty et al., 2014a; Kelly et al, 2015), rendering it a good can-didate for neurotrophic therapy for PD. GDF5 signals through a complex of the type Ib (BMPRIb) and type II (BMPRII) BMP receptors, activating the canonical Smad 1/5/8 signalling pathway (Hegarty et al., 2014b). Since GDF5 does not require Ret for its neurotrophic actions, it may have more efficacy in the PD brain, than GDNF or NRTN, both of which rely on the Ret receptor, which is now known to be down-regulated by alpha-synuclein. We are currently investigating the expression of the BMP receptors in the AAV-alpha-synuclein rat model, as well as testing the efficacy of LV- and AAV-delivered GDF5 in this model (Sullivan et al., in preparation). Another important strategy for the future clinical application of NTF therapy is the development of small molecule activators of their downstream effectors. The use of such NTF-mimicking drugs would circumvent many of the technical issues involved in the application of recombinant proteins or viral vectors.
In summary, studies to assess the clinical potential of Ret-independent NTFs and of small molecules which mimic their actions, to optimise current delivery methods for NTFs, and to enable selection of patients at earlier disease stages will be critical if the promise of NTF therapy for PD is to be fulfilled.
AMS wrote the paper; AMS and GWO’K edited the paper; GWO’K prepared the figure.
Aideen M. Sullivan*, Gerard W. O’Keeffe Department of Anatomy and Neuroscience, University College Cork, Cork, Ireland
*Correspondence to: Aideen M. Sullivan, Ph.D., a.sullivan@ucc.ie.
Accepted: 2015-12-22
orcid: 0000-0001-9692-6438 (Aideen M. Sullivan)
Back S, Peranen J, Galli E, Pulkkila P, Lonka-Nevalaita L, Tamminen T, Voutilainen MH, Raasmaja A, Saarma M, Mannisto PT, Tuominen RK (2013) Gene therapy with AAV2-CDNF provides functional benefits in a rat model of Parkinson’s disease. Brain Behav 3:75-88.
Bartus RT, Baumann TL, Siffert J, Herzog CD, Alterman R, Boulis N, Turner DA, Stacy M, Lang AE, Lozano AM, Olanow CW (2013) Safety/feasibility of targeting the substantia nigra with AAV2-neurturin in Parkinson patients. Neurology 80:1698-1701.
Barua NU, Bienemann AS, Woolley M, Wyatt MJ, Johnson D, Lewis O, Irving C, Pritchard G, Gill S (2015) Convection-enhanced delivery of MANF -Volume of distribution analysis in porcine putamen and substantia nigra. J Neurol Sci 357:264-269.
Cordero-Llana O, Houghton BC, Rinaldi F, Taylor H, Yanez-Munoz RJ, Uney JB, Wong LF, Caldwell MA (2015) Enhanced efficacy of the CDNF/MANF family by combined intranigral overexpression in the 6-OHDA rat model of Parkinson’s disease. Mol Ther 23:244-254.
Decressac M, Kadkhodaei B, Mattsson B, Laguna A, Perlmann T, Bjorklund A (2012) alpha-Synuclein-induced down-regulation of Nurr1 disrupts GDNF signaling in nigral dopamine neurons. Sci Transl Med 4:163ra156.
Decressac M, Ulusoy A, Mattsson B, Georgievska B, Romero-Ramos M, Kirik D, Bjorklund A (2011) GDNF fails to exert neuroprotection in a rat alpha-synuclein model of Parkinson’s disease. Brain 134:2302-2311.
Gill SS, Patel NK, Hotton GR, O’Sullivan K, McCarter R, Bunnage M, Brooks DJ, Svendsen CN, Heywood P (2003) Direct brain infusion of glial cell line-derived neurotrophic factor in Parkinson disease. Nat Med 9:589-595.
Hegarty SV, O’Keeffe GW, Sullivan AM (2014a) Neurotrophic factors: from neurodevelopmental regulators to novel therapies for Parkinson’s disease. Neural Regen Res 9:1708-1711.
Hegarty SV, Collins LM, Gavin AM, Roche SL, Wyatt SL, Sullivan AM, O’Keeffe GW (2014b) Canonical BMP-Smad signalling promotes neurite growth in rat midbrain dopaminergic neurons. Neuromolecular Med 16:473-489.
Kelly MJ, O’Keeffe GW, Sullivan AM (2015) Viral vector delivery of neurotrophic factors for Parkinson’s disease therapy. Exp Rev Mol Med 17: e8,1-14.
Lang AE, Gill S, Patel NK, Lozano A, Nutt JG, Penn R, Brooks DJ, Hotton G, Moro E, Heywood P, Brodsky MA, Burchiel K, Kelly P, Dalvi A, Scott B, Stacy M, Turner D, Wooten VG, Elias WJ, Laws ER, et al. (2006) Randomized controlled trial of intraputamenal glial cell line-derived neurotrophic factor infusion in Parkinson disease. Ann Neurol 59:459-466.
Marks WJ, Jr., Ostrem JL, Verhagen L, Starr PA, Larson PS, Bakay RA, Taylor R, Cahn-Weiner DA, Stoessl AJ, Olanow CW, Bartus RT (2008) Safety and tolerability of intraputaminal delivery of CERE-120 (adeno-associated virus serotype 2-neurturin) to patients with idiopathic Parkinson’s disease: an open-label, phase I trial. Lancet Neurol 7:400-408.
Marks WJ Jr, Bartus RT, Siffert J, Davis CS, Lozano A, Boulis N, Vitek J, Stacy M, Turner D, Verhagen L, Bakay R, Watts R, Guthrie B, Jankovic J, Simpson R, Tagliati M, Alterman R, Stern M, Baltuch G, Starr PA, et al. (2010) Gene delivery of AAV2-neurturin for Parkinson’s disease: a double-blind, randomised, controlled trial. Lancet Neurol 9:1164-1172.
Olanow WC, Bartus RT, Baumann TL, Factor S, Boulis N, Stacy M, Turner DA, Marks W, Larson P, Starr PA, Jankovic J, Simpson R, Watts R, Guthrie B, Poston K, Henderson JM, Stern M, Baltuch G, Goetz CG, Herzog C, et al. (2015) Gene delivery of neurturin to putamen and substantia nigra in Parkinson disease: A double-blind, randomized, controlled trial. Ann Neurol 78:248-257.
Richardson RM, Kells AP,Rosenbluth KH, Salegio, EA, Fiandaca, MS, Larson PS, Starr PA, Martin AJ, Lonser, RR, Federoff, HJ, Forsayeth, JR, Bankiewicz KS (2011) Interventional MRI-guided putaminal delivery of AAV2-GDNF for a planned clinical trial in Parkinson’s disease. Mol Ther19:1048-1057.
Slevin JT, Gerhardt GA, Smith CD, Gash DM, Kryscio R, Young B (2005) Improvement of bilateral motor functions in patients with Parkinson disease through the unilateral intraputaminal infusion of glial cell line-derived neurotrophic factor. J Neurosurg 102:216-222.
Smith RC, O’Bryan LM, Mitchell PJ, Leung D, Ghanem M, Wilson JM, Hanson JC, Sossick S, Cooper J, Huang L, Merchant KM, Lu J, O’Neill MJ (2015) Increased brain bio-distribution and chemical stability and decreased immunogenicity of an engineered variant of GDNF. Exp Neurol 267:165-176.
Sullivan AM, Toulouse A (2011) Neurotrophic factors for the treatment of Parkinson’s disease. Cytokine Growth Factor Rev 22:157-165.
10.4103/1673-5374.177710 http://www.nrronline.org/
How to cite this article: Sullivan AM, O’Keeffe GW (2016) Neurotrophic factor therapy for Parkinson’s disease: past, present and future. Neural Regen Res 11(2):205-207.
- 中国神经再生研究(英文版)的其它文章
- Gas6-Tyro3 signaling is required for Schwann cell myelination and possible remyelination
- Impaired consciousness caused by injury of the lower ascending reticular activating system: evaluation by diffusion tensor tractography
- Tissue-type plasminogen activator is a modulator of the synaptic vesicle cycle
- Cardiovascular dysfunction following spinal cord injury
- Practical application of the neuroregenerative properties of ketamine: real world treatment experience
- Exergames: neuroplastic hypothesis about cognitive improvement and biological effects on physical function of institutionalized older persons