Impairment of the nerve growth factor pathway driving amyloid accumulation in cholinergic neurons: the incipit of the Alzheimer's disease story?
Viviana Triaca, Pietro CalissanoEuropean Brain Research Institute (EBRI)/R.L. Montalcini Foundation, and Institute of Cell Biology and Neuroscience, National Research Council (IBCN-CNR), Rome, Italy
Impairment of the nerve growth factor pathway driving amyloid accumulation in cholinergic neurons: the incipit of the Alzheimer's disease story?
Viviana Triaca*, Pietro Calissano
European Brain Research Institute (EBRI)/R.L. Montalcini Foundation, and Institute of Cell Biology and Neuroscience, National Research Council (IBCN-CNR), Rome, Italy
How to cite this article: Triaca V, Calissano P (2016) Impairment of the nerve growth factor pathway driving amyloid accumulation in cholinergic neurons∶ the incipit of the Alzheimer's disease story? Neural Regen Res 11(10)∶1553-1556.
Open access statement: This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Funding: This study was supported by Ministry of Education, Universities and Research (MIUR/FIRB) funding to PC.
Data communicated as poster presentation to the following meetings:
1. “Molecular Mechanisms in Neuroscience”, Rome, Accademia dei Lincei, SINS, 3-5/10/2013, Angelicum Congress Center, Rome.
2. “Alzheimer's Association International Conference”, 12-17/07/2014, Copenhagen, Denmark.
3. “Mechanisms of Neurodegeneration”, 14 -17 June 2015, EMBL Heidelberg, Germany.
Viviana Triaca, Ph.D.,
viviana.triaca@ibcn.cnr.it.
Accepted: 2016-09-28
The current idea behind brain pathology is that disease is initiated by mild disturbances of common physiological processes. Overtime, the disruption of the neuronal homeostasis will determine irreversible degeneration and neuronal apoptosis. This could be also true in the case of nerve growth factor (NGF) alterations in sporadic Alzheimer’s disease (AD), an age-related pathology characterized by cholinergic loss, amyloid plaques and neurofibrillary tangles. In fact, the pathway activated by NGF, a key neurotrophin for the metabolism of basal forebrain cholinergic neurons (BFCN), is one of the first homeostatic systems affected in prodromal AD. NGF signaling dysfunctions have been thought for decades to occur in AD late stages, as a mere consequence of amyloid-driven disruption of the retrograde axonal transport of neurotrophins to BFCN. Nowadays, a wealth of knowledge is potentially opening a new scenario: NGF signaling impairment occurs at the onset of AD and correlates better than amyloid load with cognitive decline. The recent acceleration in the characterization of anatomical, functional and molecular profiles of early AD is aimed at maximizing the efficacy of existing treatments and setting novel therapies. Accordingly, the elucidation of the molecular events underlying APP metabolism regulation by the NGF pathway in the septo-hippocampal system is crucial for the identification of new target molecules to slow and eventually halt mild cognitive impairment (MCI) and its progression toward AD.
Alzheimer's disease onset; NGF pathway disturbances; intraneuronal amyloid generation and release; basal forebrain cholinergic neurons
NGF Pathway Dysfunctions in Mild Cognitive Impairment and AD Neurodegeneration: Lessons from Human Studies and Animal Models
The basal forebrain cholinergic neurons (BFCN) provide the major cholinergic innervation to the hippocampus and neocortex, playing a role in cognition and attention behaviors through the release of the neurotransmitter acetylcholine. BFCN are located in the medial septum, diagonal band of Broca, nucleus basalis of meynert and striatum. They are found to be massively degenerated in late stages of sporadic Alzheimer’s disease (AD), one of the most diffuse and lethal disease of the elderly. However, in contrast with the so called “cholinergic hypothesis”, AD cannot be considered as a generalized brain cholinergic disease (Mesulam, 2004). Indeed, the cholinergic system undergoes only a mild reduction of synaptic density and a partial atrophy at the AD onset, while frank BFCN degeneration and death require more than a decade to appear (Mesulam, 2004). Functional BFCN synapses relay on continuous and activity-dependent release of nerve growth factor (NGF) by cortical and hippocampal neurons (Iulita and Cuello, 2014). NGF binds to two classes of cell surface receptors localized at the BFCN terminals: the specific NGF receptor tyrosine kinase A (TrkA) and the common neurotrophic receptor p75NTR. The NGF signal is retrogradely conveyed from axons and dendrites toward the nucleus of BFCN, where it modulates cholinergic gene expression. The requirement of an active NGF/TrkA pathway in forebrain-related cognition is confirmed by the positive correlation between TrkA levels and Mini-Mental Status Examination scores.
As mentioned above, a number of experimental results prompt the perturbation of the NGF pathway as an earlyevent in AD pathology. In fact, alterations of the NGF/TrkA signaling system correlate well, and even more robustly than the amyloid load, with cognitive deficits in MCI and in its progression toward AD. Moreover, single BFCN expression analysis indicates that TrkA mRNA is reduced in MCI, and suggests that decreased neurotrophin responsiveness may be an early AD biomarker (Mufson et al., 2012). Since the pro-apoptotic NGF precursor (proNGF) increases while TrkA levels diminish in the AD forebrain, it is conceivable that degenerative pathways may override NGF-TrkA survival signals during pre-sympthomatic AD (Mufson et al., 2012). Further, experimental findings from animal and cellular models indicate that the impairment of the NGF signaling system may be a critical event in the manifestation of this pathology. Accordingly, in vitro NGF deprivation in PC12-derived and primary hippocampal neurons induces an “Alzheimer’s like molecular syndrome” with both amyloid and tau accumulation (Calissano et al., 2010). Moreover, antibody-mediated neutralization of NGF promotes the appearance of histopathological signs typical of AD, including amyloid generation and neuronal deficits in the AD11 mouse model (Ruberti et al., 2000). Thus, it would seem reasonable to antagonize basal forebrain dysfunctions in AD by exogenous NGF administration. In line with this, intracerebral NGF supply has been found beneficial to cholinergic neurons and related behavior in rodents. In particular, nasal administration of NGF modulates secretases levels and reduces amyloid burden in APP/PS1 transgenic mice (Yang et al., 2014). Of note, NGF gene therapy has been attempted in a phase 1 clinical trial, which showed high tolerability and lack of side effects in AD patients. Also, the results of a 10 years long study confirmed safety and efficacy of the NGFtherapy, and reported long lasting brain responsivity to NGF in terms of activation of functional markers, hypertrophy, and axonal sprouting (Tuszinsky et al., 2015). As less invasive alternatives to intracerebral stereotaxic NGF delivery, the NGF administration via the ocular or nasal routes has also been performed in rodents and promoted cholinergic system neuroprotection. All together, these findings underline the importance of a proper homeostatic regulation of the neurotrophic pathway in the early phase AD and pinpoint the feasibility of NGF therapy, claiming the need for efficient, safe and long-lasting therapeutic approaches for the NGF treatment of AD.

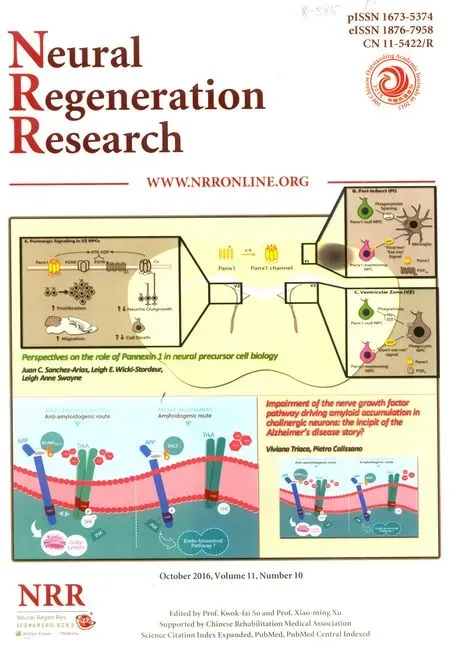
Figure 1 A schematic model illustrating amyloid precursor protein (APP) metabolism control by the nerve growth factor/tyrosine kinaseA NGF/TrkA signaling system in healthy basal forebrain cholinergic neurons (BFCN) (anti-amyloidogenic route, leTh), and the consequences of its perturbation in Alzheimer's disease (amyloidogenic route, right).
Signaling and Molecular Mechanisms Responsible for the Regulation of APP Processing by the NGF/TrkA Pathway in the Basal Forebrain
Activity-dependent release of NGF from cortical and hippocampal neurons has been demonstrated to sustain the cholinergic tone on BFCN target neurons via the muscarinic receptors 1 (M1). NGF has been thought to maintain neuronal homeostasis and forebrain-related cognition mainly through this interplay. In fact, M1 activation induces the physiological cleavage of APP to generate soluble APPα (sAPPα), which is neuroprotective per se, and it is also a potent inhibitor of the enzyme responsible for the amyloidogenic APP cleavage, the beta secretase 1 (BACE1).
Whether NGF directly regulates APP metabolism in BFCN has not been investigated so far. Indeed, we recently demonstrated that the NGF signaling pathway is able to modulate APP processing in BFCN both in vitro and in vivo (Triaca et al., 2016). We showed that stimulation of primary cholinergic septal neurons with NGF promotes binding of the NGF receptor TrkA with APP and the preferential APP trafficking to the Golgi compartment, where APP binding to and cleavage by BACE1is hampered. As a result, the levels of BACE-generated APP fragments, like soluble APP β (sAPPβ), C-terminal Fragment β (CTFβ) and beta amyloid (1-42), are strongly reduced.
In particular, we observed that binding of TrkA to APP is facilitated by NGF through the reduction of APP phosphorylation at the threonine 668 (T668) residue of its cytosolic tail. In fact, co-localization and co-immunoprecipitation analyses showed that TrkA fails to bind APP molecules phosphorylated at T668 (APPpT668), suggesting that APP phosphorylation prevents APP binding to TrkA as already observed for another APP interactor, namely Fe65. APP phosphorylation at T668 is a post-translational modification known to facilitate APP cleavage by BACE1and amyloid generation, and it was proposed as target for AD therapy (Lee et al., 2003). Thus, NGF exerts its anti-amyloidogenic action by lowering the fraction of APPpT668molecules, favoring TrkA-APP interaction and the subsequent APP processing along the anti-amyloidogenic route.
The early downstream molecular players involved in the control of APP metabolism have also been investigated. Upon NGF binding, TrkA activation promotes the phosphorylation of the isoform C of the SH2 containing sequence (Shc), the early TrkA adaptor expressed in adult BFCN. Afterward, ShcC activation inhibits the p54 isoform of the c-Jun N-terminal kinase p54 (JNK), a well known ser/thr APP kinase, thus reducing APPpT668levels, and promoting APP-TrkA binding (Figure 1).
The APP-TrkA interaction seems to have a pathological significance in AD. In fact, APP-TrkA interaction is specifically lost in AD affected tissues, like the hippocampus, while it seems to be preserved in the AD cerebellum, as well as in the hippocampus of patients affected by other neurodegenerative diseases, like Huntington’s disease. A deeper analysis of the APP-TrkA interaction in BFCN in vitro and in vivo by proximity ligation assay (PLA) and bimolecular fluorescence complementation (BiFC) is currently ongoing in our group.
Altogether, these findings suggest that the NGF system maintains amyloid levels within the physiological range in healthy BFCN by modulating APP processing by BACE1. Based on reduced TrkA and/or NGF levels observed in MCI and early AD, it is tempting to speculate that disturbances in attention and cognition may result from the perturbation of the NGF-TrkA-ShcC pathway in BFCN, inducing and/or contributing to synaptic deficits of their hippocampal and cortical target neurons.
Intraneuronal Amyloid Accumulation in BFCN during Mammalian Brain Ageing and Neurodegeneration: is Disrupted NGF Signaling the Culprit?
It is well known that BFCN are more vulnerable to AD, as compared to those located in the cerebellum. Higher forebrain susceptibility to intraneuronal amyloid accumulation has been suggested to account for this difference. Intraneuronal amyloid accumulation has been extensively demonstrated to occur during brain ageing and in AD pathology in the BFCN of mice, monkeys and humans by the Geula Lab (Baker-Nigh et al., 2015). A substantial increase of intraneuronal amyloid long before plaques formation has also been reported in 3xFAD transgenic mice (La Ferla et al., 2007). While intraneuronal amyloid is neuroprotective against oxidative stress at physiological levels (picomolar), higher concentrations have been reported to affect synaptic proteins content, spine density, and LTP. Therefore, intraneuronal amyloid accumulation has been prospected as a good predictor of synaptic and neuronal loss (Bayer and Wirths, 2010). As elegantly demonstrated by LaFerla et al. (2007), the newly generated amyloid first appears inside neurons and afterwards outside the cells, suggesting that intraneuronally generated amyloid can be released into the extracellular space causing plaque deposition in 3xFAD transgenic mice. Novelfindings from clinical examinations, amyloid imaging, and functional MRI provide evidence that not only neocortical regions, but also subcortical areas of the basal forebrain (e.g., striatum) show amyloid accumulation and neurodegeneration at the pre-symptomatic AD stage. Accordingly, early AD pathology is characterized by signs and symptoms of dysfunctional subcortical circuits (Shinohara et al., 2014). In line with this, the study of amyloid accumulation in the BFCN of mouse models lacking the mature NGF signaling will be instrumental in the pathological and molecular profiling of the AD onset.
Perspective
Based on the relevance of NGF signaling in the physiological control of APP processing in the basal forebrain, it can be hypothesized that lack of neurotrophic support may boost amyloid generation and intracellular accumulation in BFCN, thus promoting the initial synaptic disturbances seen in MCI and early AD. Here, we prospect that upon NGF withdrawal cholinergic neurons may primarily contribute to AD pathology and affect target neurons in the cortex and hippocampus by generating and releasing amyloid, possibly through the exosomal and/or synaptic routes. On the other hand, the newly generated amyloid is able to inhibit the endocytosis of the NGF/TrkA complex at the cholinergic terminals, in a negative feedback loop which settles the AD onset (Kim et al., 2016; Xu et al., 2016). Once age-related events (oxidative stress, astrogliosis, reduced amyloid clearance) occur, they compromise the brain buffering capacity and determine the overt neuronal loss of BFCN and their targets typical of late stage AD.
The fine analysis of the spatio-temporal sequence of amyloid appearance in the AD brain will hopefully provide important insights into the pathological drivers of this devastating neurodegenerative disease of the elderly, paving the way for novel targeted approaches in AD therapy.
Acknowledgments: We thank the Bioway Company (China), for generously providing the mouse salivary gland ß-NGF, all the coauthors/ collaborators, and Dr. E. Fico for technical help. A special thank to Dr. V. Sposato for the exceptional contribution to the experimental work and to A. Damiano for graphic elaboration of the illustration in Figure 1. The authors apologize for the scientific publications not acknowledged in this manuscript because of space restrictions.
Author contributions: Conceptual contents, bibliographic selection, manuscript writing, schematic modelling of the findings from “Triaca et al., 2016”. PC∶ Critical revision and final approval.
Conflicts of interest: None declared.
References
Baker-Nigh A, Vahedi S, Davis EG, Weintraub S, Bigio EH, Klein WL, Geula C (2015) Neuronal amyloid-β accumulation within cholinergic basal forebrain in ageing and Alzheimer’s disease. Brain 138:1722-1737.
Bayer TA, Wirths O (2010) Intracellular accumulation of amyloid-beta, a predictor for synaptic dysfunction and neuron loss in Alzheimer’s disease. Front Aging Neurosci 2:8.
Calissano P, Amadoro G, Matrone C, Ciafre S, Marolda R, Corsetti V, Ciotti MT, Mercanti D, Di Luzio A, Severini C, Provenzano C, Canu N (2010) Does the term ‘trophic’ actually mean anti-amyloidogenic?The case of NGF. Cell Death Differ 17:1126-1133.
Iulita MF, Cuello AC (2014) Nerve growth factor metabolic dysfunction in Alzheimer’s disease and Down syndrome. Trends Pharmacol Sci 35:338-348.
Kim S, Sato Y, Mohan PS, Peterhoff C, Pensalfini A, Rigoglioso A, Jiang Y, Nixon RA (2016) Evidence that the rab5 effector APPL1 mediates APP-β CTF-induced dysfunction of endosomes in Down syndrome and Alzheimer’s disease. Mol Psychiatry 21:707-716.
LaFerla FM, Green KN, Oddo S (2007) Intracellular amyloid-beta in Alzheimer’s disease. Nat Rev Neurosci 8:499-509.
Lee MS, Kao SC, Lemere CA, Xia W, Tseng HC, Zhou Y, Neve R, Ahlijanian MK, Tsai LH (2003) APP processing is regulated by cytoplasmic phosphorylation. J Cell Biol 163:83-95.
Mesulam M (2004) The cholinergic lesion of Alzheimer’s disease: pivotal factor or side show? Learn Mem 11:43-49.
Mufson EJ, He B, Nadeem M, Perez SE, Counts SE, Leurgans S, Fritz J, Lah J, Ginsberg SD, Wuu J, Scheff SW (2012) Hippocampal proNGF signaling pathways and β-amyloid levels in mild cognitive impairment and Alzheimer disease. J Neuropathol Exp Neurol 71:1018-1029. .
Ruberti F, Capsoni S, Comparini A, Di Daniel E, Franzot J, Gonfloni S, Rossi G, Berardi N, Cattaneo A (2000) Phenotypic knockout of nerve growth factor in adult transgenic mice reveals severe deficits in basal forebrain cholinergic neurons, cell death in the spleen, and skeletal muscle dystrophy. J Neurosci 20:2589-2601.
Shinohara M, Fujioka S, Murray ME, Wojtas A, Baker M, Rovelet-Lecrux A, Rademakers R, Das P, Parisi JE, Graff-Radford NR, Petersen RC, Dickson DW, Bu G (2014) Regional distribution of synaptic markers and APP correlate with distinct clinicopathological features in sporadic and familial Alzheimer’s disease. Brain 137:1533-1549.
Tuszynski MH, Yang JH, Barba D, U HS, Bakay RA, Pay MM, Masliah E, Conner JM, Kobalka P, Roy S, Nagahara AH (2015) Nerve growth factor gene therapy: activation of neuronal responses in Alzheimer disease. JAMA Neurol 72:1139-1147.
Xu W, Weissmiller AM, White JA 2nd, Fang F, Wang X, Wu Y, Pearn ML, Zhao X, Sawa M, Chen S, Gunawardena S, Ding J, Mobley WC, Wu C (2016) Amyloid precursor protein-mediated endocytic pathway disruption induces axonal dysfunction and neurodegeneration. J Clin Invest 126:1815-1833.
Yang C, Liu Y, Ni X, Li N, Zhang B, Fang X (2014) Enhancement of the nonamyloidogenic pathway by exogenous NGF in an Alzheimer transgenic mouse model. Neuropeptides 48:233-238.
10.4103/1673-5374.193224
*Correspondence to:
- 中国神经再生研究(英文版)的其它文章
- Recovery of an injured anterior cingulum to the basal forebrain in a patient with brain injury: a 4-year follow-up study of cognitive function
- Stem Cell Ophthalmology Treatment Study (SCOTS): bone marrow-derived stem cells in the treatment of Leber's hereditary optic neuropathy
- Combination of methylprednisolone and rosiglitazone promotes recovery of neurological function aTher spinal cord injury
- Human amniotic epithelial cells combined with silk fibroin scaffold in the repair of spinal cord injury
- Electrical stimulation promotes regeneration of injured oculomotor nerves in dogs
- Boric acid reduces axonal and myelin damage in experimental sciatic nerve injury