Stroke due to Bonzai use: two patients
Baki Dogan, Hakan Dogru, Levent Gungor, Kemal Balci Department of Neurology, Faculty of Medicine, University of Ondokuz Mayis, Samsun 55055, Turkey Corresponding Author: Kemal Balci, Email: kemalbalcidr@yahoo.com
Stroke due to Bonzai use: two patients
Baki Dogan, Hakan Dogru, Levent Gungor, Kemal Balci Department of Neurology, Faculty of Medicine, University of Ondokuz Mayis, Samsun 55055, Turkey Corresponding Author: Kemal Balci, Email: kemalbalcidr@yahoo.com
World J Emerg Med 2016;7(4):310–312
INTRODUCTION
Synthetic cannabinoids are increasingly used all over the world as marijuana substitutes. They have various names such as spice and bonzai in different countries. Cardiovascular or cerebrovascular events associated with cocaine, heroin and amphetamine abuse have been frequently reported.[1]However, stroke associated with the synthetic cannabinoids use is rarely reported. There are only a few case reports in association with synthetic cannabinoids use.[2–4]Bernson-Leung et al[5]described 2 cases that introduce a previously unreported association between synthetic cannabinoids use and ischemic stroke in young adults. Here, we report two patients with stroke that occured shortly after synthetic cannabinoids use.
CASE 1
A 35-year-old man was brought to the emergency department with complaints of left sided weakness and facial paralysis starting 3 days before admission. He has no family history for hypercoagulability, congenital heart disease, arrhythmias, stroke, or stroke risk factors. His blood pressure on admission was 138/78 mmHg and electrocardiography revealed sinus tachycardia at 110 beats/minute. Diffusion weighted magnetic resonance and apparent diffusion coeffecient images showed right middle cerebral artery territory infarction (Figure 1). His laboratory investigations were all within normal limits. He stated smoking of bonzai (synthetic cannabinoids) a few hours prior to his symptoms onset and that hehad smoked marijuana in the past, but denied recent use. He also denied the use of any other street drugs. There were no radiographic signs of vasculitis or other arterial disease. Transthoracic and transesophageal echocardiography and full hypercoagulable panel (cardiolipin antibodies immunoglobulins factor V Leiden, antithrombin 3, lupus anticoagulant, protein C antigen and activity, and protein S antigen and activity) were unremarkable. He improved clinically and did not return for his follow up visit.
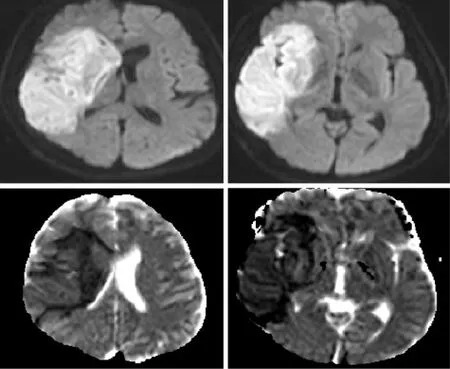
Figure 1. Diffusion weighted magnetic resonance and apparent diffusion coeffecient images showing right middle cerebral artery territory infarction (case 1).
CASE 2
A 28-year-old man was brought to the emergency department with complaints of loss of consciousness lasting a few minutes that started 4–6 hours after taking bonzai with alcohol. He denied previous use of bonzai or any other street drugs. His blood pressure was 140/75 mmHg with sinus tachycardia at 120 beats/ minute. His neurological examination was fully normal. His medical history was normal except for using bonzai and marijuana in the past. Diffusion weighted magnetic resonance and apparent diffusion coeffecient images revealed punctate ischemic lesions in pons, mesencephalone, middemporal gyrus, left occipital region, right parietosubcortical white matter regions (Figure 2). Hypercoagulable panel (factors 2, 5, 9; von Willebrand factor 8, antithrombin 3, lupus anticoagulant, protein C antigen and activity, and protein S antigen and activity) were unremarkable. Echocardiography and Cranio-cervical CT angiography investigations of the patient were normal.
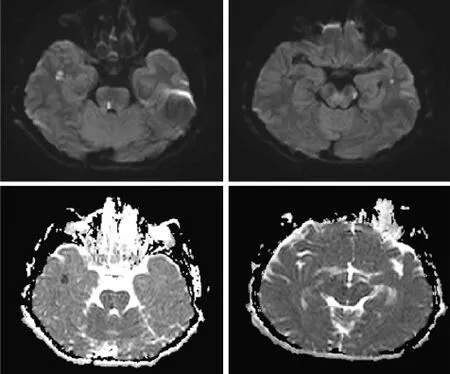
Figure 2. Diffusion weighted magnetic resonance and apparent diffusion coeffecien images revealing punctate ischemic lesions in pons, mesencephalone, middemporal gyrus, left occipital region, right parietosubcortical white matter regions (case 2).
DISCUSSION
The use of bonzai (synthetic cannabinoids) has increased among the young population due to easy accessibility in recent years.[6,7]It is usually smoked by rolling in a cigarette paper. It is known that each cigarette paper may contain different types of unidentified toxins in different amounts. Cannabinoids have two types of receptors; CB1 receptors are mainly located in the central nervous system, and CB2 receptors are found in lymphoid organs and immune cells. Synthetic cannabinoids are full agonists of CB1 receptors, and have more severe adverse effects than natural cannabinoids.[8,9]The common side effects of synthetic cannabinoids include vomiting, agitation, altered mood and perception, hallucination, epileptic seizures, hypertension, acute myocardial infarction, and kidney failure.[8–11]
To date, only a few cases of myocardial infarction and stroke have been reported due to the use of bonzai.[3–5]In this paper, we reported two young stroke cases in association with synthetic cannabinoids use. The temporal link between the use of bonzai and the occurrence of stroke were accepted as indication of a causal relationship in ourpatients. The vasoactive effects of synthetic cannabinoids may also play role in the mechanism of stroke. Our patients had increased blood pressure and heart rate. All tests investigating alternate causes of stroke returned normal.
The etiology of stroke in patients with synthetic cannabinoids use is not exactly known. In recent years, it is known that synthetic cannabinoids may also cause stroke due to direct effects on the cerebral circulation, orthostatic hypotension, central nervous system vasculitis, vasospasm, and arrhythmias.[3,12]Neuroimaging of our patients revealed a large middle cerebral artery territory infarction in patient 1 and multiple cortical and subcortical infarctions in patient 2. These images suggests the possibility of a cardioembolic etiology and/or cerebral vasospasm. Freeman et al[3]also reported two patients with acute onset cerebral infarction after smoking bonzai. They reported that the imagings of the patients have suggested an embolic etiology due to serious adverse cardiac events including tachyarrhythmias and myocardial infarctions.
In conclusion, synthetic cannabinoids are potentially harmful drugs of abuse. The use of synthetic cannabinoids among adolescents and young adults has been increasing. Emergency department physicians should be aware about the possible relationship between the occurence of stroke in young patients and synthetic cannabinoid consumption.
Funding: None.
Ethical approval: The study was approved by the Institutional Review Board of the hospital.
Conflicts of interest: The authors declare there is no competing interest related to the study, authors, other individuals or organizations.
Contributors: Dogan B proposed the study and wrote the first draft. All authors read and approved the fi nal version of the paper.
REFERENCES
1 Yeung M, Bhalla A, Birns J. Recreational drug misuse and stroke. Curr Drug Abuse Rev 2011; 4: 286–291.
2 Inal T, Köse A, Köksal O, Armagan E, Aydın SA, Ozdemir F. Acute temporal lobe infarction in a young patient associated with marijuana abuse: An unusual cause of stroke. World J Emerg Med 2014; 5: 72–74.
3 Freeman MJ, Rose DZ, Myers MA, Gooch CL, Bozeman AC, Burgin WS. Ischemic stroke after use of the synthetic marijuana“spice“. Neurology 2013; 81: 2090–2093.
4 Degirmenci Y, Kececi H, Olmez N. A case of ischemic stroke after bonzai: syntetic cannabinoid from Turkey. Neurol Sci 2016; 37: 299–300.
5 Bernson-Leung ME, Leung LY, Kumar S. Synthetic cannabinoids and acute ischemic stroke. J Stroke Cerebrovasc Dis 2014; 23: 1239–1241.
6 Castellanos D, Singh S, Thornton G, Avila M, Moreno A. Synthetic cannabinoid use: a case series of adolescents. J Adolesc Health 2011; 49: 347–349.
7 Auwärter V, Dresen S, Weinmann W, Müller M, Pütz M, Ferreirós N. Spice and other herbal blends: harmless incense or cannabinoid designer drugs? J Mass Spectrom 2009; 44: 832–837.
8 Harris CR, Brown A. Synthetic cannabinoid intoxication: a case series and review. J Emerg Med 2013; 44: 360–366.
9 Zawilska JB, Wojcieszak J. Spice/K2 drugs – more than innocent substitutes for marijuana. Int J Neuropsychopharmacol 2014; 17: 509–525.
10 Mills B, Yepes A, Nugent K. Synthetic cannabinoids. Am J Med Sci 2015; 350: 59–62.
11 Hermanns-Clausen M, Kithinji J, Spehl M, Angerer V, Franz F, Eyer F, et al. Adverse effects after the use of JWH-210-a case series from the EU Spice II plus project. Drug Test Anal. 2016 Jan 15. doi: 10.1002/dta.1936. [Epub ahead of print]
12 Singh NN, Pan Y, Muengtaweeponsa S, Geller TJ, Cruz-Flores S. Cannabis-related stroke: case series and review of literature. J Stroke Cerebrovasc Dis 2012; 21: 555–560.
Accepted after revision June 12, 2016
10.5847/wjem.j.1920–8642.2016.04.014
Clinical Image
February 1, 2016
 World journal of emergency medicine2016年4期
World journal of emergency medicine2016年4期
- World journal of emergency medicine的其它文章
- Instructions for Authors
- Subject index WJEM 2016
- Author index WJEM 2016
- Emergency department diagnosis of a concealed pleurocutaneous fi stula in a 78-year-old man using point-of-care ultrasound
- When gastroenteritis isn't: a case report of a 20-yearold male with Boerhaave's syndrome complicated by intra-abdomimal hemorrhage
- Clinical characteristics of childhood cancer in emergency room in a tertiary hospital in Pakistan
