经尿道前列腺铥激光汽化术与等离子切除术治疗前列腺增生疗效的5年随访比较
杨中华,刘同族,王行环
(武汉大学中南医院泌尿外科,湖北武汉 430071)
经尿道前列腺铥激光汽化术与等离子切除术治疗前列腺增生疗效的5年随访比较
杨中华,刘同族,王行环
(武汉大学中南医院泌尿外科,湖北武汉430071)
目的比较经尿道前列腺铥激光汽化术前列腺剜除术(ThuLEP)与经尿道前列腺等离子双极电切术(PKRP)治疗良性前列腺增生症(BPH)导致下尿路梗阻的中长期有效性、安全性。方法158例保守治疗无效的BPH患者随机分为两组,分别接受ThuLEP及PKRP手术各79例。评估患者术前及术后3 ~ 5年国际前列腺症状评分评估(IPSS)、生活质量评分(QoLS)最大尿流率(Qmax)及残余尿量 (PVR)等。结果共80例患者完成了5年随访。两组病例术前参数无显著性差异,术中无1例发生电切综合征,无1例因失血而输血,术后均无尿失禁。与PKRP相比,ThuLEP手术时间较长[(65.4±22.2)vs. (47.4±15.9) min,P=0.022],术中出血少血红蛋白下降[ (1.5±0.2)vs. (3.0±0.3) g/dL,P=0.045]。ThuLEP能减少术后膀胱冲洗量[(12.4±6.4)vs. (27.2±5.2) L,P=0.022],缩短术后留置尿管时间[(2.1±0.8)vs. (3.5±1.2)d,P=0.031]。术后60个月的随访期间,两组病例在Qmax、QoLS、IPSS、PVR方面没有显著差异(P>0.05)。 结论ThuLEP和PKRP对于缓解BPH引起的下尿路症状同样安全、有效。在止血、术后恢复方面ThuLEP优于PKRP,但切割速度不及PKRP。经过长达5年随访,两种术式在Qmax、QoLS、IPSS、PVR方面无显著差异。
前列腺增生症;等离子;铥激光;经尿道前列腺电切术
良性前列腺增生症(benign prostatic hyperpla-sia,BPH)发病率随年龄的增长而增加,严重影响患者日常生活[1]。30多年来经尿道前列腺切除术( transurethral resection of prostate,TURP)一直是手术治疗BPH的金标准,近年其并发症率显著降低。REICH等[2]的一项多中心评价提示TURP围手术期死亡率已降至0.1%,然而其并发症率仍高达11.1%。经尿道前列腺等离子双极电切术,如经尿道前列腺等离子双极电切术( transurethral resection of prostate plasma bipolarelectric cut method,PKRP)和经尿道前列腺激光汽化术,如铥激光前列腺汽化术(transurethral thulium laser vaporization of the prostate surgery,ThuLEP)是TURP的重大改进。这些技术解决了传统TURP的根本缺陷,避免了电切综合征的发生[3]。临床试验表明PKRP[4-6]及ThuLEP[7-9]在改善排尿方面与单极TURP同样有效,有望成为BPH手术治疗的新的金标准。本研究旨在通过临床随机对照研究,比较ThuLEP与PKRP治疗良性前列腺增生症导致下尿路梗阻的中长期有效性、安全性。
1 资料与方法
1.1临床资料将2009年5月至2010年6月在我中心就诊的药物治疗无效的158例BPH患者,随机分为ThuLEP治疗组和PKRP治疗组各79例。该研究获武汉大学伦理委员会批准,所有受试者在纳入研究前均给予知情同意书。入选标准为年龄小于85岁,最大尿流率(maximum flow rate,Qmax)<15 mL/s,残余尿(postvoid residual urine volume, PVR)尿量<150 mL,药物治疗失败,和经直肠超声(transrectal ultrasound, TRUS)前列腺体积<100 mL;排除标准:前列腺体积小于30 mL,证实或怀疑前列腺癌、神经源性膀胱、膀胱结石、憩室、尿道狭窄和最大膀胱容量>500 mL。
术前评估所有患者的国际前列腺症状评分(International Prostate Symptom Score, IPSS)、生活质量评分(quality of life score, QoLS)、经直肠前列腺指诊、经直肠前列腺彩超、血清前列腺特异性抗原(prostate specific antigen, PSA)、Qmax、PVR (尿量>250 mL)。
1.2设备和技术ThuLEP手术参照王行环等[10]方法。应用意大利Quanta公司生产的Cyber TM150 2 μm连续波医用激光手术治疗系统,功率70~150 W。硬膜外麻醉,截石位,术中以生理盐水作灌洗液。采用经尿道“分割式”前列腺气化切除术,将光纤探头通过激光电切镜操作通道送至前列腺尿道部,首先汽化切除中叶:于5、7点位置,从膀胱颈部至精阜两侧各切1条深沟,深达包膜,随后分块汽化、切割中叶组织,形成从膀胱颈部至精阜近端的通道;在12点处切一深沟至包膜,长度从膀胱颈部至精阜垂直水平,并将切割后分开的两侧腺体沿包膜向下剥离;将精阜两侧的前列腺尖部组织沿包膜用操作鞘剜起后,再从12点处剥离的组织向下正向切割,直至与中叶切割平面汇合。切割顺序由膀胱颈部开始,从上至下,从内到外,直到剜起的前列腺尖部腺体。同法汽化切割另一侧叶。最后沿前列腺包膜汽化修整创面。术后组织块经操作镜鞘冲出。留置F22三腔气囊导尿管,生理盐水膀胱冲洗。
PKRP手术均采用等离子系统进行(英国佳乐公司),根据标准程序手术:术中以生理盐水作灌洗液,使用等离子电切环在电切镜的配合下,依次切除前列腺中叶、左右侧叶以及尖部,术中电凝止血,冲洗清除脱落的前列腺组织后置入F22三腔导尿管,术毕生理盐水膀胱冲洗。
1.3评估和随访记录围手术期相关参数,包括手术时间、血红蛋白降低、术后尿管留置时间、冲洗量、住院时间、并发症等情况。当尿液的颜色清晰时,导管被清除。分别在术后1、2、3、4和5年评价术后排尿相关参数如IPSS、Qmax、QOLS及PVR等。
2 结 果
2.1两组患者术前情况比较两组患者在年龄、腺瘤体积、PSA水平、IPSS评分、最大尿流率及残余尿等方面无显著差异(P>0.05,表1)。

表1 两组患者术前临床资料 ±s)
2.2两组患者围手术期情况比较所有患者均成功完成手术。无TURS发生,无1例患者需要输血。术后第1周内, PKRP和ThuLEP术患者分别有3例和1例出现由前列腺创面血凝块引起的尿潴留的,均经膀胱镜直视下冲洗成功处理。在随访期间两组均无尿道及膀胱颈狭窄、尿失禁发生(表2)。
与PKRP相比,ThuLEP手术时间较长[(65.4±22.2)vs.(47.4±15.9)min,P=0.022],术中出血少,血红蛋白下降[(1.5±0.2)vs.(3.0±0.3)g/dL,P=0.045]。ThuLEP能减少术后膀胱冲洗量[(12.4±6.4)vs.(27.2±5.2)L,P=0.022],缩短术后留置尿管时间[(2.1±0.8vs.(3.5±1.2)d,P=0.031]。
2.3两组患者随访情况比较所有病例均完成了第1年的随访;共80例患者完成了5年的随访,其中PKRP组41例,ThuLEP组39例。5年随访结果如表3所示,与术前相比,两组Qmax、PVR、IPSS及QoLS显著改善(P<0.05)。在1、3和5年随访中,PKRP及ThuLEP组间上述参数无显著性差异(P>0.05)。
表2围手术期临床资料

指标PKRP(n=79)ThuLEP(n=79)t值P值手术时间(min)47.4±15.965.4±22.21.3380.022切割速度(g/min)2.1±0.51.4±0.31.3270.021留置尿管时间(d)3.5±1.22.1±0.83.3670.031膀胱冲洗量(L)27.2±5.212.4±6.44.3190.022Hb降低(g/dL∗)0.30±0.030.15±0.022.1530.045住院时间(d)4.6±1.42.5±1.42.8760.026
*分别在手术开始时和手术结束后采血检测血红蛋白。
表3两组患者5年随访结果比较
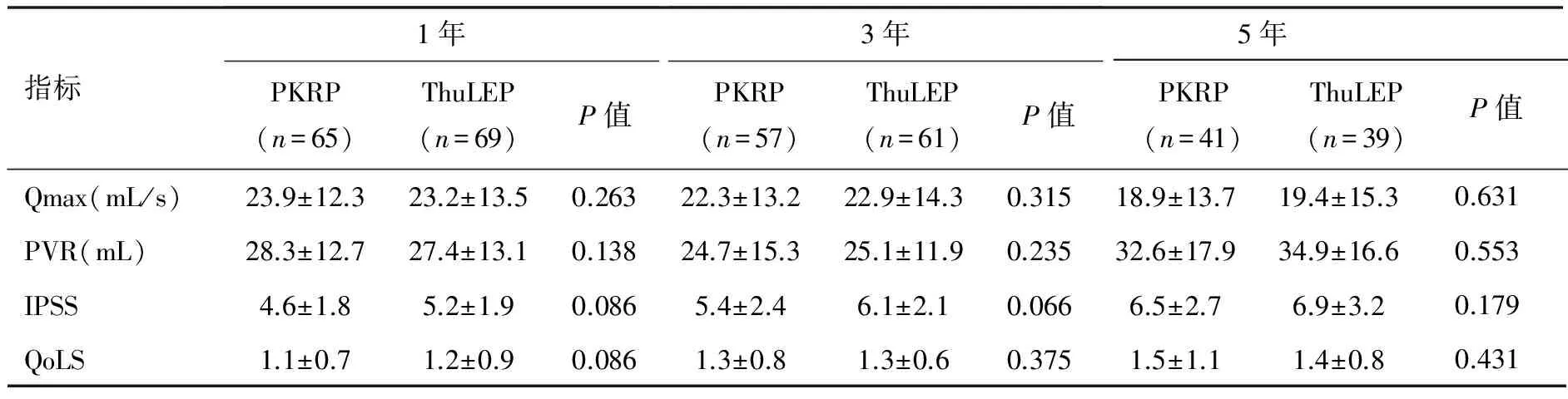
指标1年PKRP(n=65)ThuLEP(n=69)P值3年PKRP(n=57)ThuLEP(n=61)P值5年PKRP(n=41)ThuLEP(n=39)P值Qmax(mL/s)23.9±12.323.2±13.50.26322.3±13.222.9±14.30.31518.9±13.719.4±15.30.631PVR(mL)28.3±12.727.4±13.10.13824.7±15.325.1±11.90.23532.6±17.934.9±16.60.553IPSS4.6±1.85.2±1.90.0865.4±2.46.1±2.10.0666.5±2.76.9±3.20.179QoLS1.1±0.71.2±0.90.0861.3±0.81.3±0.60.3751.5±1.11.4±0.80.431
3 讨 论
TURP是治疗前列腺增生的金标准,但也存在诸多不足:术中使用5%甘露醇或葡糖液等非电解质灌洗液,其大量吸收可致体内水电解质平衡失调,甚至出现TURS;TURP创面凝固层厚度为 0.1~0.3 mm,凝固层薄,止血效果差,失血较多[11]。等离子双极电切术及铥激光汽化/切除术是TURP的技术改进,可使用生理盐水作为灌洗液,且具有较强止血效果,避免了TURS的发生,降低了大出血的风险。这些改进使得在切除较大体积前列腺时不会因为担心失血和TURS的发生而导致前列腺切除不完全。
多中心、大样本荟萃分析表明在短期临床疗效方面,双极和单极TURP无显著性差异,但双极电切术因无电切综合征和止血效果好而更具安全性;而激光治疗则可以进一步减少TURS和大出血的风险。目前已有多种激光设备应用于临床,其中绿光汽化和钬激光剜除术应用最为广泛,可望取代TURP而成为新的金标准[12]。铥激光中心波长1.75~2.22 μm,其能量可导致组织表面瞬间汽化和凝固,深度达500~2 000 μm,从而达到安全切割和充分止血目的[13]。
在本研究中,PKRP术中因出血少而视野清晰,切割创面光滑,切割速度快[ (47.4 ±15.9)vs.(65.4±22.2) min,P<0.05],腺体及周围包膜结构清晰可辨,因而降低了切穿包膜及术后疤痕狭窄的风险;ThuLEP术中几乎无出血,因此缩短术后膀胱冲洗时间[(12.4±6.4)vs.(27.2±5.2)L,P<0.05]、缩短留置尿管时间[(2.1±0.8)vs. (3.5±1.2)d,P<0.05],但创面光滑程度不及PKRP。
在术后随访中,两组Qmax、PVR、IPSS及QoLS较与术前相比均获显著改善,且无尿失禁及尿道狭窄发生。在1、3和5年随访中,PKRP及ThuLEP组间上述参数无显著性差异,表明PKRP及ThuLEP在改善症状方面同样有效。
[1] ALCARAZ A, CARBALLIDO J, UNDA M, et al. Quality of life in patients with lower urinary tract symptoms associated with BPH: change over time in real-life practice according to treatment-the QUALIPROST study[J]. Int Urol Nephrol,2016,48(5):645-656.
[2] REICH O, GRATZKE C, BACHMANN A, et al. Morbidity, mortality and early outcome of transurethral resection of the prostate: a prospective multicenter evaluation of 10,654 patients[J]. J Urol, 2008, 180(1):246-249.
[3] CORNU JN. Bipolar, Monopolar, photovaporization of the prostate, or holmium laser enucleation of the prostate: how to choose what’s best[J]. Urol Clin North Am, 2016, 43(3):377-384.
[4] YANG EJ, LI H, SUN XB, et al. Bipolar versus monopolar transurethral resection of the prostate for benign prostatic hyperplasia: safe in patients with high surgical risk[J]. Scientific reports, 2016,6:21494.
[5] HIRIK, BOZKURT A, KARABAKAN M, et al. Safety and efficacy of bipolar versus monopolar transurethral resection of the prostate: a comparative study[J]. Urology,2015,12(6):2452-2456.
[6] DA SILVA RD, BIDIKOV L, MICHAELS W, et al. Bipolar energy in the treatment of benign prostatic hyperplasia: a current systematic review of the literature[J]. Canad J Urol, 2015, 22 (Suppl 1):30-44.
[7] BARBOZA LE, MALAFAIZ O, SLONGO LE, et al. Holmium laser enucleation of the prostate (HoLEP) versus transurethral resection of the Prostate (TURP) [J]. Revista do Colegio Brasileiro de Cirurgioes, 2015, 42(3):165-170.
[8] DUSING MW, KRAMBECK AE, TERRY C, et al. Holmium laser enucleation of the prostate: efficiency gained by experience and operative technique. [J] J Urol, 2010, 184(2):635-640.
[9] AL-ANSARI A, YOUNES N, SAMPIGE VP, et al. GreenLight HPS 120-W laser vaporization versus transurethral resection of the prostate for treatment of benign prostatic hyperplasia: a randomized clinical trial with midterm follow-up [J]. Eur Urol, 2010, 58(3):349-355.
[10] YANG Z, WANG X, LIU T. Thulium laser enucleation versus plasmakinetic resection of the prostate: a randomized prospective trial with 18-month follow-up[J]. Urology,2013, 81(2):396-400.
[11] CORNU JN, AHYAI S, BACHMANN A, et al. A Systematic review andmeta-analysis of functional outcomes and complications following transurethral procedures for lower urinary rract symptoms resulting from benign prostatic obstruction: an update[J]. Eur Urol, 2015, 67(6):1066-1096.
[12] ZHOU Y, XUE B, MOHAMMAD NA, et al. Greenlight high-performance system (HPS) 120-W laser vaporization versus transurethral resection of the prostate for the treatment of benign prostatic hyperplasia: ameta-analysis of the published results of randomized controlled trials[J]. Lasers Med Sci,2016, 31(3):485-495.
[13] SUN F, HAN B, CUI D, et al. Long-term results of thulium laser resection of the prostate: a prospective study at multiple centers [J]. World J Urol,2015, 33(4):503-508.
(编辑何宏灵)
Comparison of thulium laser enucleation and plasmakinetic resection of the prostate in a randomized prospective trial with 5-year follow-up
YANG Zhong-hua, LIU Tong-zu, WANG Xing-huan
(Department of Urology, Zhongnan Hospital of Wuhan University, Wuhan 430071, China)
ObjectiveTo compare the clinical outcomes between thulium laser transurethral enucleation of the prostate (ThuLEP) and plasmakinetic bipolar resection of the prostate (PKRP) for benign prostatic hyperplasia (BPH) in a prospective randomized trial with 5 years of follow-up. Methods A total of 158 consecutive patients with BPH were randomized to ThuLEP (n=79) and PKRP (n=79) group. All cases were evaluated preoperatively and part of them were evaluated 3~5 years postoperatively with International Prostate Symptom Score (IPSS), quality of life score (QoLS), maximum flow rate (Qmax) and postvoid residual urine volume (PVR). Results A total of 80 patients completed the 5-year follow-up. There were no significant differences in preoperative parameters. Compared with PKRP, ThuLEP required longer operation time [(65.4±22.2)vs.(47.4±15.9)min,P=0.022], less catheterization time [(2.1±0.8)vs.(3.5±1.2)d,P=0.031] and irrigated volume [(12.4±6.4)vs.(27.2±5.2)L,P=0.022], but resulted in less haemoglobin decrease [(1.5±0.2)vs.(3.0±0.3)g/dL,P=0.045]. During the 60-month follow-up, no significant differences in terms of Qmax, IPSS, PVR, and QoLS were observed between the two groups of patients. ConclusionBoth ThuLEP and PKRP can relieve lower urinary tract symptoms effectively and safely. ThuLEP is statistically superior to PKRP in blood loss, catheterization time, irrigated volume and hospital stay, but inferior to PKRP in operation time. There are no significant differences in terms of Qmax, IPSS, PVR, and QoLS between the two approaches.
benign prostatic hyperplasia; plasma; thulium laser; transurethral resection of the prostate
2016-06-09
2016-08-30
王行环,主任医师,教授,博士生导师.
E-mail:wangxinghuan@whu.edu.cn.
杨中华(1977-),男(汉族),主治医师,博士.研究方向:泌尿男生殖系疾病.E-mail:yangzhonghua@whu.edu.cn.
R699
ADOI:10.3969/j.issn.1009-8291.2016.10.007

