A West Malaysian study of pediatric ocular trauma
Fiona Chew Lee Min, Fazilawati Qamaruddin
·Original article·
A West Malaysian study of pediatric ocular trauma
Fiona Chew Lee Min, Fazilawati Qamaruddin
Department of Ophthalmology,Hospital Selayang, Lebuhraya Selayang-Kepong, Batu Caves 68100, Selangor Darul Ehsan, Malaysia
方法:回顾性研究。对所有2009-01/2013-12就诊于急诊创伤科的连续患者进行筛检,选取年龄在15岁以下的眼外伤患者纳入研究对象。排除随访患者。收集患者人口统计学数据、既往治疗和眼部病史资料。详细记录眼外伤情况,治疗和疾病发展情况。
结果:小儿眼外伤的患病率为每年17.6/100000。其中男性患者占69.5%(296/426例)。患者的平均年龄为6.08±2.24岁。家用工具(19.7%)和摔伤(19.7%)是致眼外伤最常见的原因。多数患者(79.9%)救诊时的视力≥6/12。眼前节(93.9%)最容易受伤,22.8%的患者需要手术治疗。相对性瞳孔传入障碍与闭合性眼球损伤程度(P=0.001)及不良视力预后(P=0.001)相关。大多数患者(92.7%)的最终视力≥6/12。
结论:须提高对小儿眼外伤的预防意识并及时进行治疗,以确保患者视力的最大程度恢复。
•AIM: To survey ophthalmological outcomes of pediatric patients who presented during a five-year period with ocular trauma to a tertiary referral center in West Malaysia.
•METHODS: All consecutive patients presenting to the Accident and Emergency Department from Jan. 2009 to Dec. 2013 were identified. Patients were recruited as study subjects if they were less than 15y of age and had sustained ocular trauma. Follow-up patients were excluded. Data collected including the subjects’ demographic data and past medical and ocular history. Ocular injury, treatment and progress details were also recorded.
•RESULTS: The prevalence of pediatric ocular trauma was 17.6/100000 per year. Males represented 69.5% of the 426 subjects recruited. Mean subject age was 6.08 years [standard deviation (SD): 2.24]. Domestic tools (19.7%) and falls (19.7%) represented the commonest causes of trauma. Most subjects (79.9%) had presenting visual acuity (VA) of 6/12 or better. The anterior segment of the eye (93.9%) was most commonly injured, and 22.8% of subjects required surgery. Relative afferent pupillary defect was associated with closed globe injury (P=0.001) and poorer final VA (P=0.001). Final VA in most subjects (92.7%) was 6/12 or better.
•CONCLUSION: Increased awareness is necessary for the prevention and early ophthalmological intervention of pediatric ocular trauma, to ensure optimum visual rehabilitation for these patients.
pediatric eye trauma; ocular trauma; children; eye injury
INTRODUCTION
Visual disabilities resulting from ocular trauma have a life-long impact on a child’s life. A child with visual impairment has greater difficulty performing motor skills especially in relation to locomotion and objectcontrol[1]. In addition, traditional school examination papers are biased towards visual tasks and experiences[2]. Hence, a child with visual impairment faces an uphill task of integrating into normal society both physically and socially[3]. Morrisetal[4]reported that 34.8% of ocular injury patients had a poor visual outcome. In view the series of events leading to ocular trauma are potentially preventable; there is a need to focus on the potential risk factors of ocular trauma in the pediatric population to look for preventive measures.
Malaysia comprises of a federation of states and federal territories, and can be divided into East and West Malaysia. West Malaysia is more urbanized with facilities comparable to developed nations while East Malaysia is less developed, with some areas lacking basic amenities such as electricity and water supply. The difference in urbanization has lead to variations of demography and social interactions between East and West Malaysia.
Gohetal[5]noted that 17.1% of Malaysian school-age children had visual impairment of 20/40 or worse, while Pateletal[6]estimated the prevalence of blindness in children in Malaysia to be 3/10000 children. Madhusudhanetal[7]reported that for open globe injuries in Kelantan, a state in the East Coast of Malaysia, domestic-related injury was the most common cause for children below 16y of age. Most of the study patients however were adults and only a third of their children were pre-school children. This differed from Tanetal’s[8]study who noted that pre-school children represented more than half of the patients (58.2%) aged less than 12y of age who presented to the ophthalmology department for ocular trauma in Sarawak, East Malaysia. Soongetal[9]also looked at ocular trauma over a period of 1y in Kuala Lumpur, in the West Coast of peninsular Malaysia, however most of the patients in the study were adult patients.
In view the demography between East and West Malaysia varies dramatically, our study aimed to conduct a retrospective review to document the risk factors, incidence and visual outcomes of pediatric ocular trauma over a 5y period in Hospital Selayang, a general hospital with tertiary ophthalmic services, situated in the state of Selangor, West Malaysia.
SUBJECTS AND METHODS
This retrospective study, conducted from Oct. 2014 to Jan. 2015, conformed to all local laws and was compliant with the guidelines of the Declaration of Helsinki. Ethical approval was obtained from the Medical Research and Ethics Committee of Malaysia [NMRR-14-1469-22852 (IIR)]. In view this was a retrospective study, informed consent was not obtained from subjects, no subjects received stipend and there was no patient contact with the investigative team. Consecutive patients presenting to the Accident and Emergency Department from Jan. 2009 to Dec. 2013 were identified from a computerised admission database. The inclusion criteria were ocular trauma patients aged less than 15y. Exclusion criteria were patients coming to the hospital for follow-up appointments. Demographic data and subjects’ past medical history and history of any previous trauma were noted. Details related to the ocular injury were also recorded. Data from the injured eye was used for data analysis. The eye that sustained the most ocular injury was used for data analysis in subjects who sustained trauma in both eyes. Subject’s ocular findings were documented and Birmingham Eye Trauma Terminology System[10]was used for classification of the sustained ocular injury. The presence of relative afferent pupillary defect (RAPD) was defined as paradoxical pupillary dilatation in response to light noted during the swinging flashlight test[11]. Treatment received and ophthalmological follow-up was recorded.
StatisticsData collected was entered into an Excel spreadsheet (Microsoft Excel for Mac 2011, version 14.5.7, Redmont, Washington,USA). SPSS version 13 (SPSS Statistics: Windows Student Version 13, Chicago, Illinois, USA) was used for data analysis. Categorical data was analysed using Fisher’s exact test and multinomial logistic regression. APvalue of less than 0.05 was taken as statistically significant.
Table 1Demography of study subjects
Characteristics(n=426)Age<7a7-10a11-14aPGender M18683270.337 F95287Ethnicity Malay21278230.910 Chinese28105 Indian41236Medicalillness Y291520.562 N2529632Previoustrauma Y3100.780 N27811034Placeofinjury Home1915180.005 School35366 Street472119 Other831Eyeinvolvement Right14548150.386 Left1185918 Both1841
RESULTS
A total of 484 833 patients aged less than 15y of age presented as new cases to Selayang Hospital with 523 patients having sustained ocular trauma. Of these 523 patients, 97 patients were excluded, as they were follow-up patients. The final number of study subjects totaled 426 patients, where boys represented 69.5% (296/426) of subjects. Subjects’ age ranged from 1mo to 14y of age with a mode age of 2y [mean: 6.08y, standard deviation (SD: 2.24)]. Majority of the subjects were Malays 73.5% (313/426), followed by Indians (16.4%, 70/426) and Chinese(10.1%, 43/426) Most subjects did not have history of previous trauma (422/426, 99.1%) or previous medical illness (380/426, 89.2%). Nine patients had developmental delay(Table 1).
Ocular trauma occurred mostly at home (58.7%, 250/426) and on the streets (20.4%, 87/426). School-going age children (40.7%, 59/145) were less likely to sustain ocular trauma at home in comparison to pre-school children (68.0%,191/281;P=0.005). Most ocular trauma events (80%) were reported to have occurred after 12 p.m. Although most subjects presented less than 24h post injury, 22.3% (95/426) had delayed hospital presentation. The time of delayed presentation ranged from 1.2 to 30d with a mean of 3.1d (SD: 3.9). Reasons for the delay included delayed reporting of the injury by the patient themselves (42.1%, 40/95), under-recognition of the eye injury by subjects parents (30.5%, 29/95), late referral by medical staff (16.8%, 16/95) and logistic concerns (10.5%, 10/95).
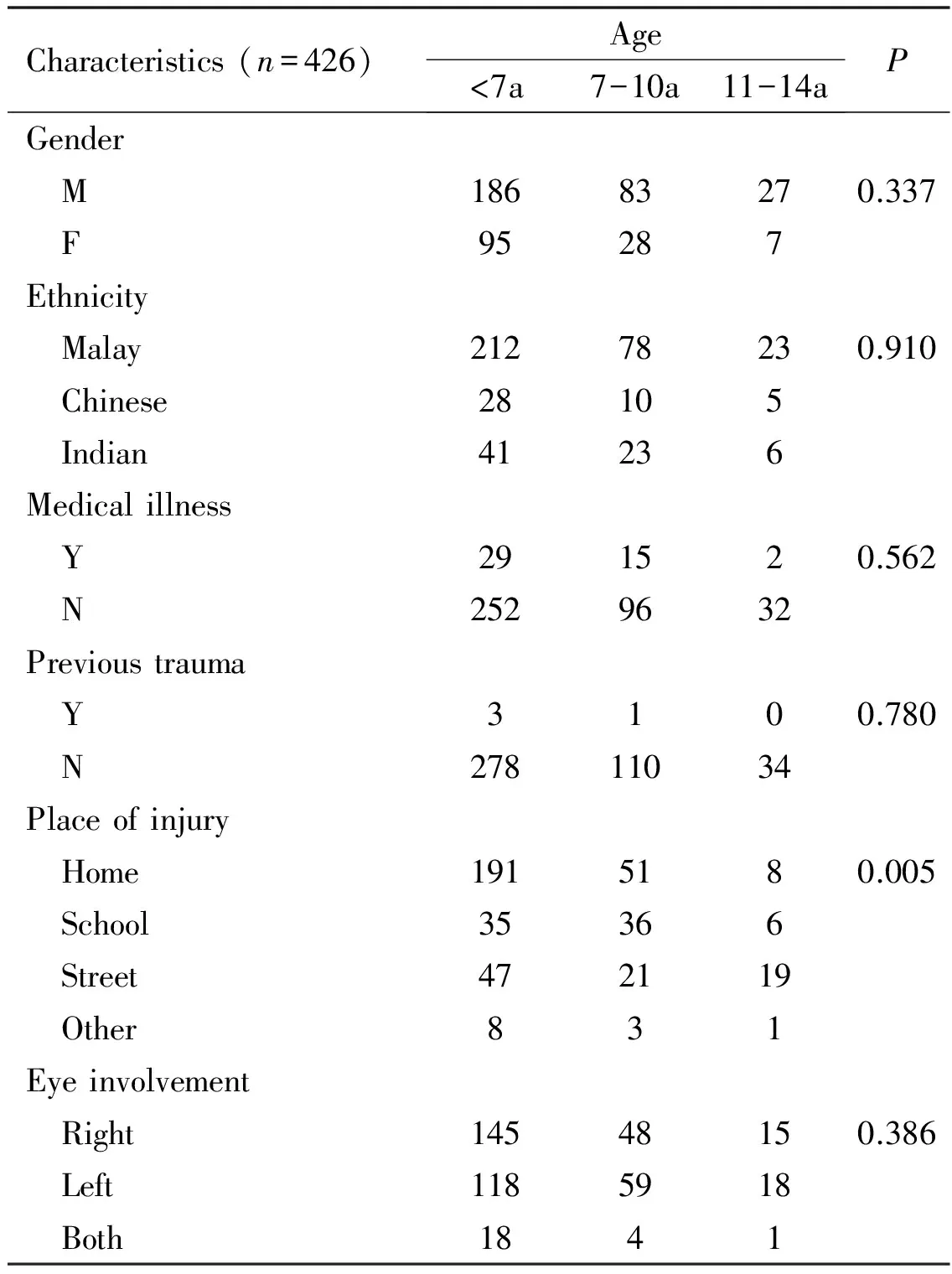
DOmestic tools such as cradle hooks, screwdriver, furniture and cleaning apparatus comprised of 19.7% (84/426) of the causes of ocular trauma. Falls from staircase, chairs, beds and into drains contributed 19.7% (84/426). Projectile toys such as toy gun bullets (35/50) and sharp toy edges(15/50) caused 11.7% (50/426) of the injuries sustained. Majority of the subjects involved in motor vehicle accidents (MVA) were motorcycle passengers (17/47) who fell off and sustained injury. Documentation regarding the usage of safety helmets was not available. Seven patients aged 14y were driving motorcycle alone when the accident occurred. Subjects involved in car accidents (12/47) sustained injury from hitting the car seat or windscreen impact injuries. None of the subjects involved used a child car seat. Pen, pencil and ruler were the commonest items of stationery involved in subjects’ ocular trauma. The cause of injury in 9(2.1%) patients was not known as the incident happened in the absence of eyewitnesses (Figure 1).
Presenting visual acuity was recorded in 359 subjects (84.3%). Most subjects (79.9%, 287/359) had presenting visual acuity (VA) of better than 6/12. Subjects with bilateral eye involvement comprised of 5.4% (23/426) of the study population. Seven subjects (1.4%) had relative afferent pupillary defect (RAPD). The anterior segment of the eye was the commonest area of injury (93.9%). Sixteen patients (3.5%) sustained open globe injuries, out of which 5 patients had scleral perforation and 11 patients had corneal perforation. Corneal or conjunctival abrasion was the most common injury in all three age groups (Figure 2). Less patients with closed globe injury (3/407, 0.74%) had RAPD in comparison to patient’s with open globe injury (4/16, 25.0%) (P=0.001).
Most subjects (314/426, 73.7%) did not require hospitalization. For subjects who required hospitalization, the duration of hospitalization for the ocular injury ranged from 1 to 12d with a mean of 1.01d (SD: 2.17). Most patients were compliant to treatment however 7 patients (1.6%) refused treatment. Surgical intervention for study subjects comprised of toilet and suturing of the eyelids (83.2%, 79/95) and repair of open globe injuries (16.8%, 16/95). Out of the 95 subjects who required surgical intervention, 9 patients proceeded to have a second surgery for traumatic cataract. Post-trauma follow-up ranged from 1d to 5y (mean: 46.2d, SD: 194.4). Most subjects (92.7%) had a final VA of better than 6/12. RAPD was associated with poorer final VA where more patients with vision worse than 6/12 (28.6%, 6/21) had RAPD in comparison with patients with vision better than 6/12(0.38%, 1/269) (P=0.001, Fisher’s exact test). At final follow-up, 2 patients were transferred to another healthcare facility and 31% (132/426) patients defaulted their follow-up visit.
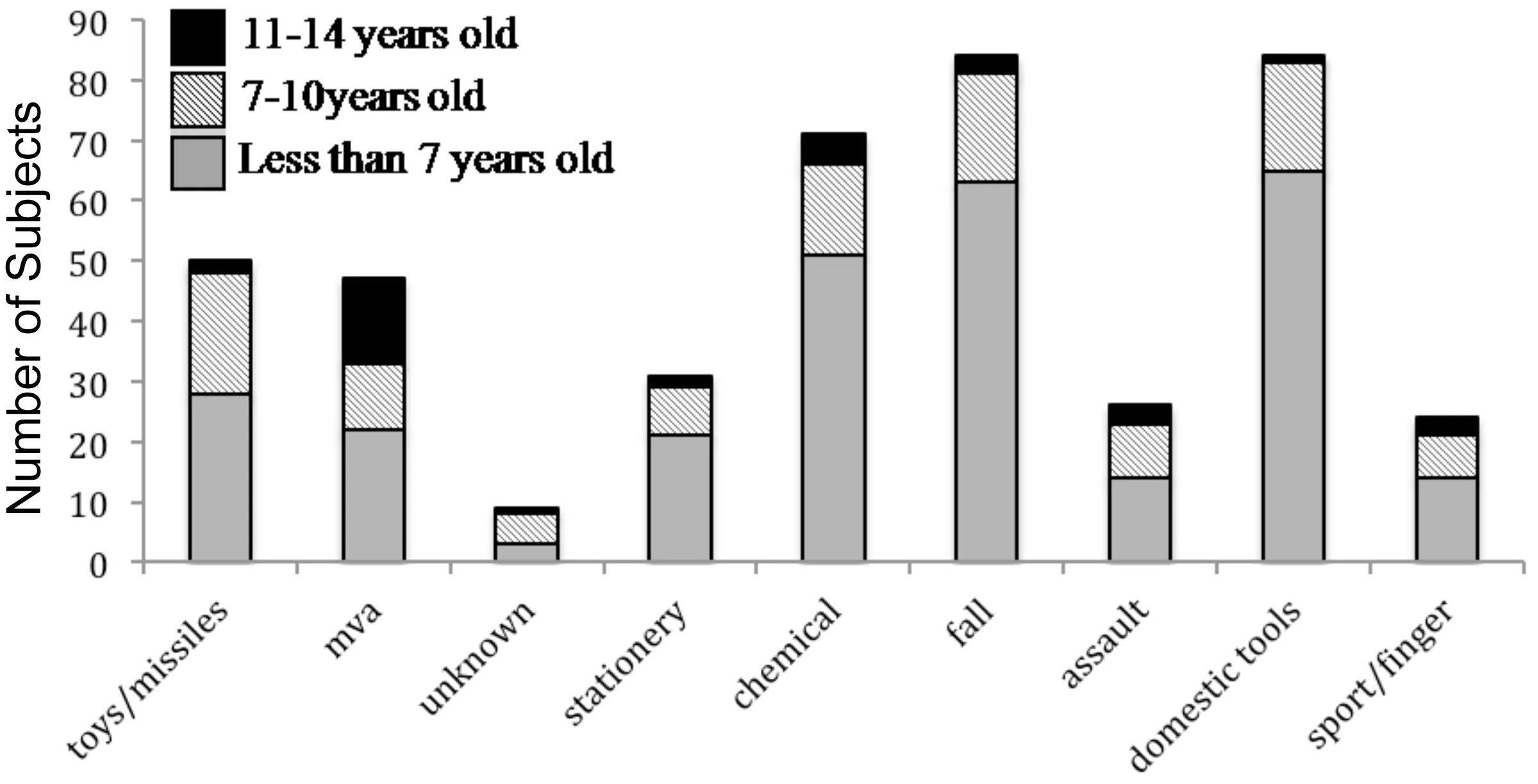
Figure 1Causes of pediatric ocular.
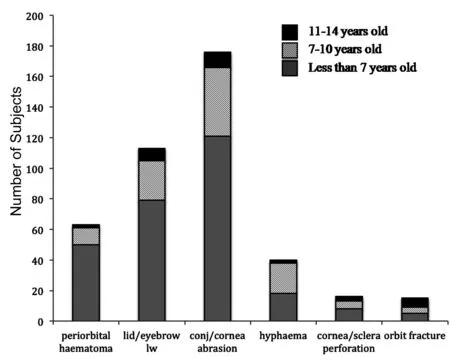
Figure 2Injuries sustained among study subjects.
DISCUSSIONOur study prevalence of pediatric ocular trauma was 17.6/100000 per year. Variation in cumulative incidence rates in other countries of 8.85-300/100 000 per year[12-14]could result from ethnic, cultural or social-economic differences. The preponderance of males in our study echoed the observation of male gender being a risk factor for ocular trauma[9,14-17]. Most subjects (66.0%, 281/426) were less than 7y of age. This corresponded to previously reported data[7,18].
Pre-school subjects suffered more injury involving domestic tools. This reflected the amount of time spent at home by this age-group. Projectile toys were responsible for all the cases of hyphema in the middle-childhood group. Largely preventable toy-related injuries revealed the need for judicious selection of age-appropriate toys[18]. Bhallaetal[19]reported that globally, 75% of children involved in road traffic accidents are either pedestrians or vehicle occupants. Kulanthayanetal[20]reported that only 27.4% of Malaysian drivers used child safety seats (CSS) and most families who owned a CSS did not have one CSS per age-appropriate child. The lack of usage of car seats, seatbelts and motorcycle helmets by the subjects involved in motor vehicle accidents in our study suggested an urgency for increased awareness regarding road safety for children.
Most subjects sustained closed globe injuries. This differed from regional data where open globe injuries were reported as being more common[8,21-24]. This could be due to different population demography and the inclusion of outpatients as well as inpatients in our subject recruitment. Our study findings of RAPD being associated with open globe injury and a poorer visual outcome was similar to previously reported data[25].
Zuckermanetal[26]noted that at least 42% of children’s parents experienced at least one barrier to seeking speciality healthcare for their children. These barriers included leaving work, childcare, transportation and communication issues. Kemperetal[27]reported that 24.4% of children who had abnormal preschool vision screening testing defauted their follow-up ophthalmology appointments. Our study also found potential barriers to seeking ophthalmological healthcare where one fifth of our study subjects delayed seeking ophthalmological care, and nearly a third of our subjects defaulted their ophthalmological follow-up. More research need to be done in this area.
Our study limitations were that it was retrospective in nature and involved a single tertiary referral center. Also, documentation of subjects’ visual acuity at first presentation was sparse, limited by the child’s vocabulary and cooperation. Our study however is still relevant as it is the largest study from Malaysia reporting results of pediatric ocular trauma in West Malaysian and the first to report the prevalence for pediatric ocular trauma in Malaysia. In conclusion, pediatric ocular trauma is largely preventable. Lack of awareness regarding child safety and barriers to healthcare remain issues, which need to be addressed in future research.
1 Matthias MO, Haibach PS, Lieberman LJ. Gross motor skill performance in children with and without visual impairments-Research to practice.ResDevDisabil2013;34(10):3246-3252
2 Cobb R. Assessing the attainment of children with visual impairment in public tests and examinations.IntCongrSer2005;1282:806-810
3 Movahedi A, Mojtahedi H, Farazyani F. Differences in socialization between visually impaired student-athletes and non-athletes.ResDevDisabil2011; 32(1): 58-62
4 Morris DS, Willis S, Minassian D, Foot B, Foot B, Desai P, MacEwen CJ. The incidence of serious eye injury in Scotland: a prospective study.Eye(Lond) 2014;28(1):34-40
5 Goh PP, Abqariyah Y, Pokharel GP, Ellwein LB. Refractive Error and Visual Impairment in School-Age Children in Gombak District, Malaysia.Ophthalmology2005;112(4):678-685
6 Patel DK, Tajunisah I, Gilbert C, Subrayan V. Childhood blindness and severe visual impairment in Malaysia: a nationwide study.Eye(Lond) 2011;25(4): 436-442
7 Madhusudhan AP, Evelyn-Tai LM, Zamri N, Adil H, Wan-Hazabbah WH. Open globe injury in Hospital Universiti Sains Malaysia-a 10-year review.IntJOphthalmol2014;7(3):486-490
8 Tan A, Mallika P, Asokumaran T, Mohamad Aziz S, Intan G. Paediatric Ocular Trauma in Kuching, Sarawak, Malaysia.MalaysianFamilyPhysician2011;6(2-3): 68-71
9 Soong TK, Koh A, Subrayan V, Loo AV. Ocular trauma injuries: a 1-year surveillance study in the University of Malaya Medical Centre, Malaysia. 2008.GraefesArchClinExpOphthalmol2011;249(12):1755-1760
10 Kuhn F, Morris R, Witherspoon CD, Mester V. The Birmingham Eye Trauma Terminology System (BETT).JFrOphthalmol2004;27(2):206-210
11 Broadway DC. How to test for a relative afferent pupillary defect (RAPD).CommunityEyeHealth2012; 25(79-80):58-59
12 Desai P, MacEwen CJ, Baines P, Minassian DC. Incidence of cases of ocular trauma admitted to hospital and incidence of blinding outcome.BrJOphthalmol1996;80(7):592-596
13 Strahlman E, Elman M, Daub E, Baker S. Causes of pediatric eye injuries. A population-based study.ArchOphthalmol1990; 108(4): 603-606
14 Khatry SK, Lewis AE, Schein OD, Thapa MD, Pradhan EK, Katz J. The epidemiology of ocular trauma in rural Nepal.BrJOphthalmol2004;88(4): 456-460
15 Loon SC, Tay WT, Saw SM, Wang JJ, Wong TY. Prevalence and risk factors of ocular trauma in an urban south-east Asian population: the Singapore Malay Eye Study.ClinExperimentOphthalmol2009;37(4):362-367
16 Abbott J, Shah P. The epidemiology and etiology of pediatric ocular trauma.SurvOphthalmol2013;58(5):476-485
17 Acar U, Tok OY,Acar DE, Burcu A, Ornek F. A new ocular trauma score in pediatric penetrating eye injuries.Eye(Lond) 2011;25(3):370-374
18 Rashid RA, Heidary F, Hussein A Hitam WH, Rashid RA, Ghani ZA, Omar NA, Mustari Z, Shatriah I. Ocular burns and related injuries due to fireworks during the Aidil Fitri celebration on the East Coast of the Peninsular Malaysia.Burns2011;37(1):170-173
19 Bhalla K, Mohan D. Safety of young children on motorized two-wheelers around the world: A review of the global epidemiological evidence.IATSSResearch2015;38(2):83-91
20 Kulanthayan S, Razak A Ellen Schenk E. Driver characteristics associated with child safety seat usage in Malaysia: A cross-sectional study.AccidentAnalPrev2010;42(2):509-514
21 Al-Mahdi HS, Bener A, Hashim SP. Clinical pattern of pediatric ocular trauma in fast developing country.IntEmergNurs2011;19(4):186-191
22 Ram J, Verma N, Gupta N, Chaudhary M. Effect of penetrating and blunt ocular trauma on the outcome of traumatic cataract in children in northern India.JTraumaAcuteCareSurg2012;73(3):726-730
23 Liu ML, Chang YS, Tseng SH, Cheng HC, Huang FC, Shih MH, Hsu SM, Kuo PH. Major Pediatric Ocular Trauma in Taiwan.JPediatrOphthalmolStrabismus2010;47(2):88-95
24 Cao H, Li L, Zhang M, Li H. Epidemiology of Pediatric Ocular Trauma in the Chaoshan Region, China, 2001-2010.PLoSOne2013;8(4):e60844
25 Yu Wai Man C, Steel D. Visual outcome after open globe injury: a comparison of two prognostic models- the Ocular Trauma Score and the Classification and Regression Tree.Eye(Lond) 2010; 24(1):84-89
26 Zuckerman KE, Perrin JM, Hobrecker K, Donelan K. Barriers to Specialty Care and Specialty Referral Completion in the Community Health Center Setting.JPediatr2013;162(2): 409-414
27 Kemper AR, Uren RL, Clark SJ. Barriers to Follow-up Eye Care After Preschool Vision Screening in the Primary Care Setting: Findings From a Pilot Study.JAAPOS2006;10(5): 476-478
马来西亚西部小儿眼外伤研究
Fiona Chew Lee Min, Fazilawati Qamaruddin
(作者单位:68100马来西亚雪兰莪州黑风洞甲洞士拉央大道士拉央医院眼科)
Fiona Chew Lee Min. sabrefmin@gmail.com
目的:调查5a期间就诊于马来西亚西部三级转诊中心的小儿眼外伤患者的视力结果。
小儿眼外伤;眼外伤;儿童;眼损伤
Fiona Chew Lee Min. Department of Ophthalmology, Hospital Selayang, Lebuhraya Selayang-Kepong, Batu Caves 68100, Selangor Darul Ehsan, Malaysia. sabrefmin@gmail.com
2015-12-23Accepted: 2016-04-19
10.3980/j.issn.1672-5123.2016.7.03
Chew FLM, Qamaruddin F. A West Malaysian study of pediatric ocular trauma.GuojiYankeZazhi(IntEyeSci) 2016;16(7):1212-1215
引用:Chew FLM, Qamaruddin F. 马来西亚西部小儿眼外伤研究.国际眼科杂志2016;16(7):1212-1215

