隐匿性胰液反流与胆道疾病间的相关性
杨慧慧 李会兵 刘爽 刘贤英
·论著·
隐匿性胰液反流与胆道疾病间的相关性
杨慧慧李会兵刘爽刘贤英
目的探讨隐匿性胰液反流(OPR)与胆道疾病间的相关性。方法收集44例原发性胆道疾病患者,取血检测血清淀粉酶活性,收集胆总管胆汁,测定胆汁淀粉酶活性,计算胆总管的Δ胆汁淀粉酶活性(即胆总管胆汁淀粉酶活性-血清淀粉酶活性)。以胆总管胆汁淀粉酶活性高于血清淀粉酶活性视为该患者存在OPR,将其纳入OPR组,反之则纳入未发生OPR的对照组。结果44例胆道疾病患者中32例存在OPR,发生率为72.7%。OPR组患者胆汁淀粉酶、血清淀粉酶活性分别为(1 513±2 725)、(45±21)U/L,对照组为(18±14)、(38±16)U/L,OPR组胆汁淀粉酶活性显著高于对照组,差异有统计学意义(P<0.05),而两组血清淀粉酶活性差异无统计学意义。OPR组中单纯胆总管结石患者的OPR发生率为100%,胆汁淀粉酶活性为(1 048±1 317)U/L,Δ胆汁淀粉酶活性为(996±1 322)U/L;胆总管结石合并胆囊结石患者分别为75%,(2 457±3 312)、(2 412±3 320)U/L;单纯胆囊结石患者分别为80%,(95±82)、(57±76)U/L;胆总管恶性肿瘤患者为50%,(73±54)、(40±37)U/L。结论OPR的发生与胆总管结石、胆总管结石合并胆囊结石密切相关,OPR可能是发生胆系结石的主要致病因素之一。
隐匿性胰液反流;胆道疾病;胆汁;淀粉酶类
胰液反流入胆管往往被认为是胆系恶性肿瘤的重要危险因素。既往研究发现胰液反流多发生于胰胆管合流异常的患者。近年来有研究报道,胰液反流不仅发生于胰胆管合流异常的患者,也发生于隐匿性胰液反流(occult pancreaticobiliary reflux, OPR)人群。关于OPR以及其对胆道疾病影响的研究以国外居多,国内文献报道甚少。本研究收集原发性胆系疾病患者的胆总管胆汁,通过测定血清及胆总管胆汁的淀粉酶活性判断其是否存在OPR,探讨OPR与胆系疾病发生的关系,以期为临床提供有意义的客观指标。
材料与方法
一、研究对象
收集经彩色多普勒超声、MRCP、CT证实为原发性胆道疾病拟行治疗的患者。患者排除条件:(1)经影像学检查确诊为胰胆管合流异常的患者,即胆总管与主胰管汇合后的共同管道长度>15 mm;(2)经影像学检查确诊为胆管狭窄的患者;(3)既往有Oddi括约肌切开史;(4)无法收集到足够量的胆汁;(5)术前血清淀粉酶活性增高者。共纳入44例患者,其中男性22例,女性22例,年龄22~90岁,平均年龄(58±16)岁。诊断:胆总管结石9例,胆囊结石5例,胆总管结石合并胆囊结石15例,肝内胆管结石1例,肝内胆管结石合并胆总管结石2例,胆总管恶性肿瘤10例,胆囊结石合并胆囊幽门腺上皮组织转化1例,胆管炎1例。
二、研究方法
术前48 h内抽取患者静脉血,离心分离血清,测血淀粉酶活性。胆总管胆汁收集主要通过以下途径:(1)手术中抽取患者胆总管胆汁3~5 ml;(2)ERCP术中在注射造影剂之前用注射器抽取3~5 ml胆总管胆汁(为排除干扰因素,将第一管胆汁弃去)。收集的胆汁立即离心取上清,测胆汁的淀粉酶活性。胆总管胆汁的淀粉酶活性高于血淀粉酶活性视为该患者存在OPR,纳入OPR组,反之则纳入不存在OPR的对照组。
三、统计学处理
结 果
一、不同胆道疾病患者的胆汁、血清淀粉酶活性及OPR的发生率
不同胆道系统疾病患者的胆汁、血清淀粉酶活性见表1。44例胆道疾病患者中32例存在OPR,发生率为72.7%,其中胆总管结石患者的OPR发生率最高,达100%。
二、OPR组患者与对照组患者淀粉酶活性比较
OPR组胆汁、血清淀粉酶活性分别为(1 513±2 725)、(45±21)U/L;对照组为(18±14)、(38±16)U/L。OPR组胆汁淀粉酶活性显著高于对照组,差异有统计学意义(Z=-4.443,P=0.000),而两组血清淀粉酶活性差异无统计学意义。
三、OPR组内不同胆道疾病患者胆汁、血清淀粉酶活性比较
胆总管结石、胆总管结石合并胆囊结石患者的胆汁淀粉酶活性分别为(1 048±1 317)、(2 457±3 312)U/L,血清淀粉酶活性分别为(52±20)、(45±23)U/L,胆汁淀粉酶活性均显著高于血清淀粉酶活性,差异均有统计学意义(Z值分别为-3.103、-3.223,P值均<0.01);单纯胆囊结石及胆总管恶性肿瘤患者的胆汁淀粉酶活性分别为(95±82)、(73±54)U/L,血清淀粉酶活性分别为(37±15)、(33±18)U/L,差异无统计学意义。
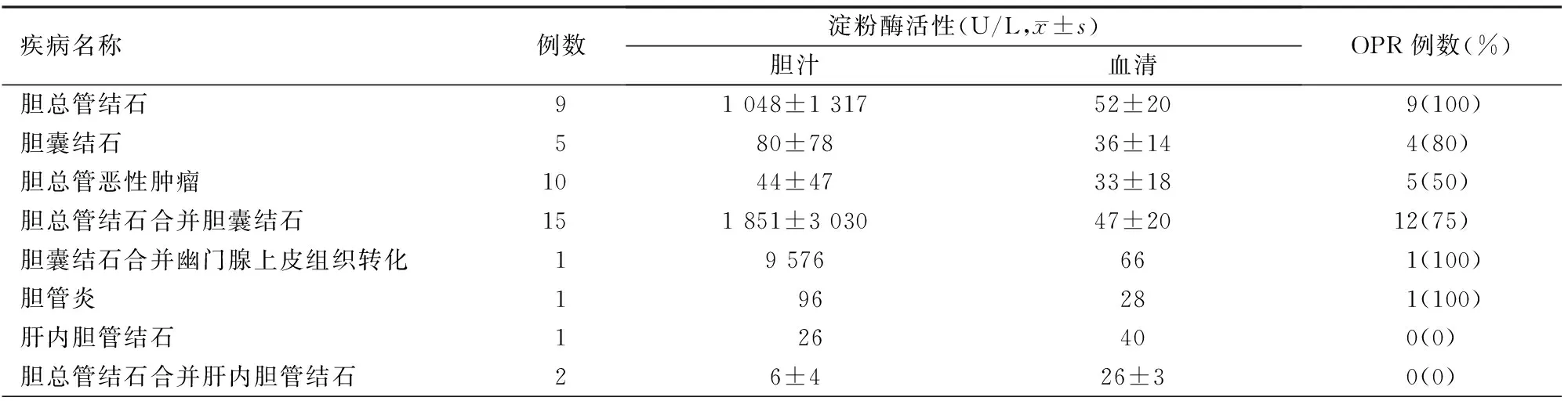
表1 不同胆道疾病胆汁淀粉酶和血清淀粉酶活性及OPR发生情况
胆总管结石、胆总管结石合并胆囊结石、胆囊结石、胆总管恶性肿瘤患者的Δ胆汁淀粉酶活性(即胆总管胆汁淀粉酶活性-血清淀粉酶活性)分别为(996±1 322)、(2 412±3 320)、(57±76)、(40±37)U/L,4组间的差异有统计学意义(H=9.053,P=0.029)。其中胆总管结石与胆总管恶性肿瘤、胆总管结石合并胆囊结石与胆囊结石、胆囊结石与胆总管恶性肿瘤的差异均有统计学意义(Z=-2.208,P=0.027;Z=-2.160,P=0.031;Z=-2.160,P=0.031),而胆总管结石与胆总管结石合并胆囊结石、胆总管结石与胆囊结石、胆总管结石合并胆囊结石与胆总管恶性肿瘤的差异均无统计学意义(Z值分别为-1.868、-0.577、-0.289,P值均>0.05)。
讨 论
OPR发生的原因可能是由于Oddi括约肌功能失调[1]。正常情况下,胰胆管汇合处有Oddi括约肌,它可以防止胰液反流和(或)胆汁反流[2]。胆汁淀粉酶活性往往作为胰液反流入胆管的生物化学指标,它是由血清淀粉酶经肝脏过滤和胰液反流入胆管而来[1,3-4]。OPR患者Oddi括约肌功能障碍导致胰液反流入胆管并长期刺激胆管壁致使胆管壁上皮细胞慢性炎症,加快上皮细胞的增殖速度,从而导致上皮细胞增生和组织转化,最终导致癌症发生[5-7]。
既往研究[8-9]都将胰胆管合流正常患者的胆汁淀粉酶活性大于血清淀粉酶活性正常上限值定义为OPR。本研究将胆汁淀粉酶活性大于自身血清淀粉酶活性视为OPR,这样可避免因血清淀粉酶活性的个体差异而造成研究结果上的偏差,且更加贴近OPR本身的含义。文献报道的有关OPR研究所收集的胆汁部位不尽相同[8-9]。有研究[10-11]报道,不合并胆管扩张的胰胆管合流异常患者的胆囊胆汁淀粉酶活性明显高于胆总管胆汁淀粉酶活性。Itokawa等[10]收集同一患者胆囊胆汁和胆总管胆汁,发现58%的胆囊胆汁淀粉酶活性高于胆总管胆汁。本研究参照了Horaguchi等[8]的方法,收集胆总管的胆汁。
Anderson等[11]报道,胆道疾病患者中OPR的发生率为81%。Beltran等[7]报道胆囊疾病患者中OPR的发生率为84.2%;胆总管结石合并胆囊结石患者OPR的发生率为100%。本研究的OPR总发生率为72.7%,其中胆总管结石患者的发生率高达100%,胆总管结石合并胆囊结石患者OPR的发生率也高达75%,与文献报道的结果相近。
Horaguchi等[8]研究显示,OPR中胆总管结石患者胆汁淀粉酶平均活性较高。本研究结果显示,OPR患者胆汁淀粉酶平均活性为(1 513±2 725)U/L,其中胆总管结石合并胆囊结石患者胆汁淀粉酶活性最高,其次为胆总管结石患者,且均显著高于他们自身的血清淀粉酶活性,同时这两组患者OPR的发生率也最高,提示OPR的发生与胆总管结石、胆总管结石合并胆囊结石密切相关,OPR可能是发生胆管结石的主要致病因素之一。而胆总管恶性肿瘤患者胆汁淀粉酶平均活性较低, OPR的发生率也相对较低,与Horaguchi等[8]的研究相同。
本研究在国内首次探讨了OPR与胆道疾病间的相关性,但样本量有限,需收集更多的病例进一步加以证实。
[1]Sai JK, Ariyama J, Suyama M, et al. Occult regurgitation of pancreatic juice into the biliary tract: diagnosis with secretin injection magnetic resonance cholangiopancreatography[J]. Gastrointest Endosc,2002,56(6):929-932.
[2]张宗明,苑海明,张翀.双镜联合同期治疗胆囊结石合并胆总管结石的策略[J].中华消化外科杂志,2015,14(4):280-283. DOI:10.3760/cma.j.issn.1673-9752.2015.04.005.
[3]Donaldson LA, Joffe SN, McIntosh W,et al. Amylase activity in human bile[J]. Gut,1979,20(3):216-218.
[4]邹树,田伏洲. 胆汁中淀粉酶过高的临床意义[J]. 肝胆胰脾外科杂志,1997,3(3):188-189.
[5]Tashiro S, Imaizumi T, Ohkawa H, et al. Pancreaticobiliary malj unction:retrospective and nationwide survey in Japan[J]. J Hepatobiliary Pancreat Surg, 2003,10(5):345-351.
[6]Matsubara T, Sakurai Y, Sasayama Y, et al.K-ras point mutations in cancerous and nonc ancerous biliary epithelium in patients with pancreaticobiliary maljunction[J]. Cancer, 1996,77 (8 Suppl):1752-1757.
[7]Beltran MA, Vracko J, Cumsille MA, et al. Occult pancreaticobiliary reflux in gallbladder cancer and benign gallbladder diseases[J].J Surg Oncol,2007,96(1):26-31.
[8]Horaguchi J, Fujita N, Noda Y, et al. Amylase levels in bile in patients with a morphologically normal pancreaticobiliary ductal arrangement[J]. J Gastroenterol,2008,43(4):305-311.
[9]Aoki T, Tsuchida A, Kasuya K, et al. Is preventive resection of the extrahepatic duct necessary in cases of pancreaticobiliary maljunction without dilatation of the bile duct[J]? Jpn J Clin Oncol, 2001,31(3):107-111.
[10]Itokawa F,Itoi T,Nakamura K,et al. Assessment of occult pancreatobiliary reflux in patients with pancreaticobiliary disease by ERCP[J]. J Gastroenterol, 2004,39(10):988-994.
[11]Anderson MC, Hauman RL, Suriyapa C, et al. Pancreatic enzyme lever in bile of patients with extrahepatic biliary tract disease[J]. Am J Surg, 1979,137(3):301-306.
(本文编辑:屠振兴)
Relationship between occult pancreaticobiliary reflux and biliary diseases
YangHuihui,LiHuibing,LiuShuang,LiuXianying.
DepartmentofUltrasound,AnyangSixthPeople′sHospital,Anyang455000,China
Correspondingauthor:LiuXianying,Email:liuxianying66@hotmail.com
ObjectiveTo investigate the relationship between occult pancreaticobiliary reflux (OPR) and biliary diseases. MethodsForty-four patients with primary biliary diseases was enrolled, and serum amylase level was determined, and the bile in common bile duct (CBD) was collected to measure the amylase level, then the Δ amylase was calculated, which equals bile amylase level minus serum amylase level. OPR was confirmed if bile amylase level was higher than serum amylase level, otherwise it would be defined as the control group. ResultsAmong the 44 patients with primary biliary diseases, the incidence of OPR was 72.7% (n= 32). The bile and serum amylase activity of patients with OPR were (1 513±2 725), (44±21)U/L; and they were (18±14) and (38±17) U/L in the control group. The bile amylase level in OPR group was significantly higher than that in the control group, and the difference was statistically significant (P<0.05), while there was no significant difference in serum amylase activity between the two groups. The incidence of OPR in patients with CBD stones was 100%, and the bile amylase activity was (1 048±1 317)IU/L, and the Δ bile amylase activity was (996±1 322)U/L; the incidence of OPR in patients with choledocholithiasis and cholecystolithiasis was 75%, and the bile amylase activity was (2 457±3 312), the Δ amylase activity was (2 412±3 320)IU/L; and the corresponding values in patients with gallbladder stones were 80%, (95±82), (57±76)IU/L; and the corresponding values in patients with bile duct cancer were 50%, (73±51), (40±37)U/L. ConclusionsThe occurrence of OPR is closely related to CBD stones only, CBD stones and gallbladder stones, and it may be one of the main pathogenic factors of bile duct stones.
Occult pancreaticobiliary reflux;Biliary tract diseases;Bile;Amylases
10.3760/cma.j.issn.1674-1935.2016.01.007
455000河南安阳,河南省安阳市第六人民医院超声科(杨慧慧),神经外科(李会兵);吉林大学第二附属医院超声科(刘爽),科教科(刘贤英)
刘贤英,Email: liuxianying66@hotmail.com
2015-04-24)