Effects of professional rehabilitation training on the recovery of neurological function in young stroke patients
Chao-jin-zi Li, Xiao-xia Du,, Kun Yang, Lu-ping Song, Peng-kun Li, Qiang Wang, Rong Sun, Xiao-ling Lin Hong-yu Lu Tong Zhang School of Rehabilitation Medicine, Capital Medical University, Beijing, China Department of Neurological Rehabilitation, Beijing Bo’ai Hospital, China Rehabilitation Research Center, Beijing, China Department of Neurology, Xi’an Gaoxin Hospital, Xi’an, Shaanxi Province, China Room of Medical Records, Beijing Bo’ai Hospital, China Rehabilitation Research Center, Beijing, China
RESEARCH ARTICLE
Effects of professional rehabilitation training on the recovery of neurological function in young stroke patients
Chao-jin-zi Li1,2, Xiao-xia Du1,2,*, Kun Yang3, Lu-ping Song1,2, Peng-kun Li1,4, Qiang Wang1,2, Rong Sun1,2, Xiao-ling Lin1, Hong-yu Lu1, Tong Zhang1,2
1 School of Rehabilitation Medicine, Capital Medical University, Beijing, China
2 Department of Neurological Rehabilitation, Beijing Bo’ai Hospital, China Rehabilitation Research Center, Beijing, China
3 Department of Neurology, Xi’an Gaoxin Hospital, Xi’an, Shaanxi Province, China
4 Room of Medical Records, Beijing Bo’ai Hospital, China Rehabilitation Research Center, Beijing, China
How to cite this article:Li CJZ, Du XX, Yang K, Song LP, Li PK, Wang Q, Sun R, Lin XL, Lu HY, Zhang T (2016) Effects of professional rehabilitation training on the recovery of neurological function in young stroke patients. Neural Regen Res 11(11):1766-1772.
Open access statement:This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Funding:This research was supported by the Special Fund of Basic Scientific Research Service Fee of Central Public Welfare Scientific Research Institute of China, No. 2014CZ-13.
Graphical Abstract
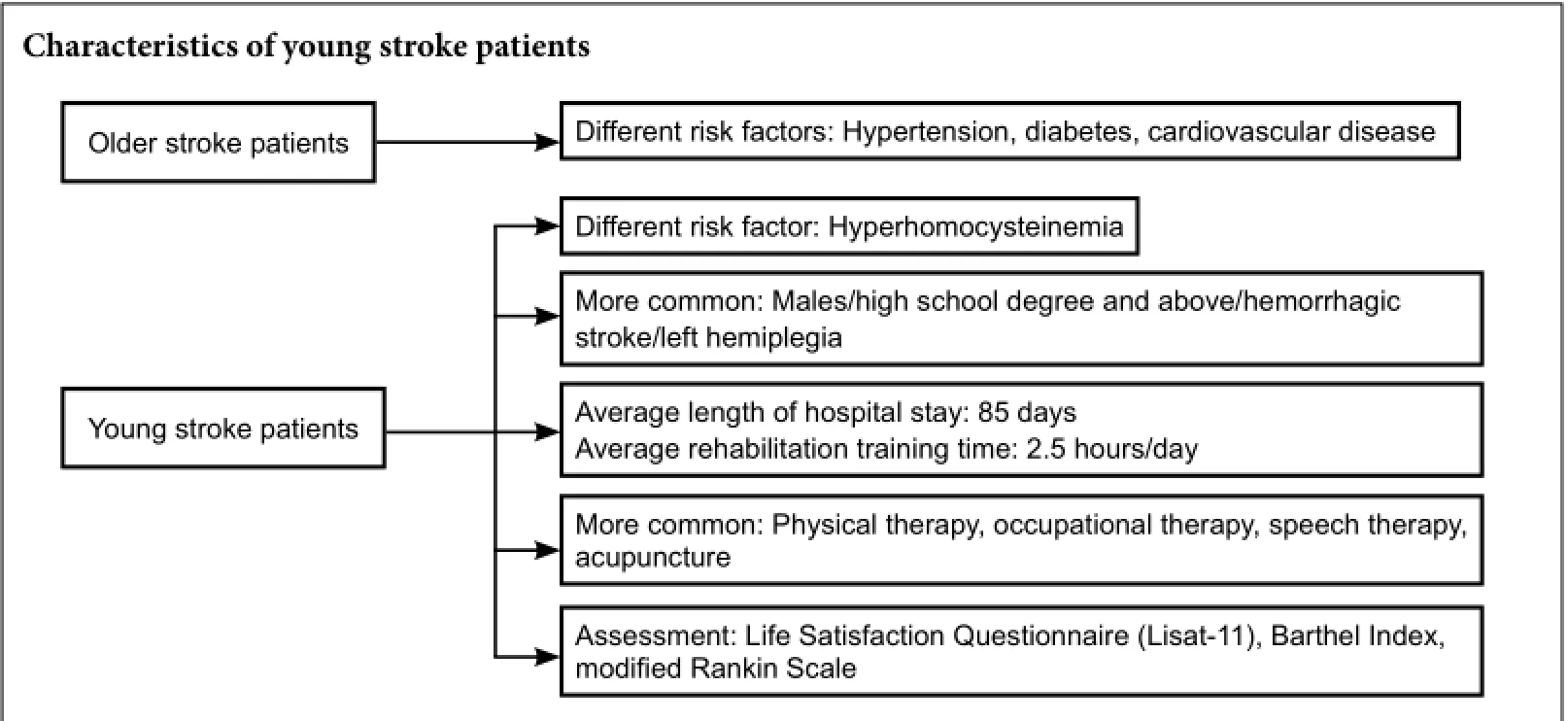
Young stroke patients have a strong desire to return to the society, but few studies have been conducted on their rehabilitation training items, intensity, and prognosis. We analyzed clinical data of young and middle-aged/older stroke patients hospitalized in the Department of Neurological Rehabilitation, China Rehabilitation Research Center, Capital Medical University, China from February 2014 to May 2015. Results demonstrated that hemorrhagic stroke (59.6%) was the primary stroke type found in the young group, while ischemic stroke (60.0%) was the main type detected in the middle-aged/older group. Compared with older stroke patients, education level and incidence of hyperhomocysteinemia were higher in younger stroke patients, whereas, incidences of hypertension, diabetes, and heart disease were lower. The average length of hospital stay was longer in the young group than in the middle-aged/older group. The main risk factors observed in the young stroke patients were hypertension, drinking, smoking, hyperlipidemia, hyperhomocysteinemia, diabetes, previous history of stroke, and heart disease. The most accepted rehabilitation program consisted of physiotherapy, occupational therapy, speech therapy, acupuncture and moxibustion. Average rehabilitation training time was 2.5 hours/day. Barthel Index and modified Rankin Scale scores were increased at discharge. Six months after discharge, the degree of occupational and economic satisfaction declined, and there were no changes in family life satisfaction. The degrees of other life satisfaction (such as friendship) improved. The degree of disability and functional status improved significantly in young stroke patients after professional rehabilitation, but the number of patients who returned to society within 6 months after stroke was still small.
nerve regeneration; young stroke patients; risk factors; recovery of neurological function; prognosis; Life Satisfaction Questionnaire; Barthel Index; modified Rank Scale; neural regeneration
Introduction
Stroke with high incidence and high disability seriously threatens human life and health. Stroke onset in young patients between 18 and 44 years, is inclusive. Morbidity has been reported between 7 and 15 cases per 100,000 individuals (Griffiths and Sturm, 2011). Morbidity accounts for 5–15% of all strokes (Bi and Beijing Neurologist Club, 2003). In recent years, the incidence of stroke is rising. The etiology and risk factors for young stroke patients differ from those for middle-aged and older stroke patients, and are complicated in young patients with ischemic stroke (Béjot et al., 2013; Sultan and Elkind, 2013). Numerous studies have shown that the onset of stroke in young people is associated with hypertension, family history of stroke, smoking and hyperhomocysteinemia in developing countries (Hill et al., 1991; Lee et al., 2002; Feigin et al., 2003; Benninger et al., 2009; De Silva et al., 2009; Onwuchekwa et al., 2009; Griffiths and Sturm, 2011; Park et al., 2014). Moreover, the proportion of stroke without any clear cause increases year by year, and different risk factors are reported in different studies (Hill et al., 1991; Lee et al., 2002; Feigin et al., 2003; Benninger et al., 2009; De Silva et al., 2009; Onwuchekwa et al., 2009; Griffiths and Sturm, 2011; Park et al., 2014).
Professional rehabilitation relieves dysfunction in stroke patients, and promotes and maintains the recovery of cognition, language, movement, psychology, and social function. The demand to return to society and work is high in young stroke patients, but there are few studies that focus on rehabilitation training items, intensity, or prognosis for young stroke patients. Indeed, a multicenter study demonstrated a current lack of unified evaluation criteria for the effect of rehabilitation therapy in stroke patients (Engbers et al., 2005; Kuptniratsaikul et al., 2009). No studies regarding the rehabilitation, strength, or prognosis for young stroke patients have been performed in China.
We sought to analyze the clinical data of stroke patients hospitalized over the course of one year in the Department of Neurological Rehabilitation, China Rehabilitation Research Center, Capital Medical University, China. We compared general data and risk factors between young stroke patients and middle-aged/older stroke patients. We first analyzed rehabilitation and strength in young stroke patients by comparing the degree of disability and functional status between the time of admission and the time of discharge. We also collected information regarding the degree of disability, functional changes, life satisfaction, and return to society 6 months after discharge in young stroke patients. This was done to help patients have better access to rehabilitation services and to improve their quality of life.
Subjects and Methods
Ethics statement
We obtained written approval for all procedures from the Clinical Research Ethics Committee of Beijing Boai Hospital, China (approval No. 2012N15). Patients or their legal representatives signed an informed consent. This study was conducted in accordance with theDeclaration of Helsinki, formulated by the World Medical Association.
Participants
We collected data from 324 stroke patients who were hospitalized in the Department of Neurological Rehabilitation, China Rehabilitation Research Center, Capital Medical University, China from February 2014 to May 2015. There were 135 young patients and 183 middle-aged/older patients. One hundred of these patients were randomly selected from each group. The specific method for random selection was as follows: (1) Number all the young patients and middle-aged/ older patients separately, and generate two random number tables (data insupplementary Tables 1and2 online). (2) In the young group, patients were chosen by extracting every other number starting in row 1, column 1 of the table from left to right, proceeding to the last column of the last row. In the elderly group, the numbers were extracted fromsupplementary Table 2 online, and the method is the same as the young group.
Inclusion criteria: Young group: (1) met World Health Organization (WHO) diagnostic criteria for stroke (no authors listed, 1988); (2) verified by CT or MRI of the head (cerebral infarction, cerebral hemorrhage, subarachnoid hemorrhage); (3) age ≥ 18 years and ≤ 44 years; (4) vital signs stable, could complete instructions to keep sitting for longer than 30 minutes; (5) Mini-Mental State Examination score (Tombaugh and McIntyre, 1992) ≥ 17,i.e., normal cognitive function and mild to moderate cognitive impairment. Middle-aged/ older group: (1) age ≥ 45 years; (2) other criteria were the same as the young group.
Exclusion criteria: (1) Brain tumor or brain injury; (2) other severe systemic diseases or death; (3) imperfect medical record data, unable to carry out the risk factor analysis.
Survey contents and methods
(1) General data
General data were obtained in the following respects. 1. General conditions: age, sex, type of stroke, side of hemiplegia, education level, and medical insurance; 2. Presence or absence of risk factors: hypertension, diabetes, heart disease, hyperlipidemia, hyperhomocysteinemia, previous stroke, history of smoking, and history of drinking.
Hypertension: In accordance with WHO diagnostic criteria, without taking any hypotensive medication, the average blood pressure was calculated after at least two measurements taken on different days. If systolic pressure was ≥140 mmHg or diastolic pressure was ≥ 90 mmHg, or if the patient had a history of hypertension, blood pressure was controlled with hypotensive medication to be below 140/90 mmHg (Chalmers, 1999).
Diabetes: In accordance with WHO criteria for diabetes (World Health Organization, 2006), diabetes was diagnosed if fasting blood glucose was ≥ 7.0 mM, 2-hour postprandial blood glucose was ≥ 11.1 mM, random blood sugar levels were ≥ 11.1 mM, or glycosylated hemoglobin was ≥ 6.5%.
Coronary atherosclerotic heart disease: including stable angina, non-ST-segment elevation acute coronary syndrome, ST-segment elevation acute myocardial infarction, and silent myocardial ischemia (Fraker et al., 2007; Rapezzi et al., 2008).
Heart disease was diagnosed if there was mitral stenosis,prosthetic valve replacement, coronary atherosclerotic heart disease, left ventricular mural thrombus, left ventricular aneurysm, persistent or paroxysmal atrial fibrillation, sick sinus syndrome, dilated cardiomyopathy, endocarditis, intracardiac tumor, or patent foramen ovale.
Hyperlipidemia was diagnosed if there was an abnormally elevated level of plasm or serum cholesterol and (or) triglycerides induced by lipid metabolism disorders. This included serum cholesterol levels > 5.72 mM (220 mg/dL), plasm triglycerides levels > 1.7 mM (150 mg/dL) (Joint Committee for Developing Chinese guidelines on Prevention and Treatment of Dyslipidemia in Adults, 2007). Because the WHO classification from 1970 was complicated, this study used the following clinical classification: hypercholesterolemia, hypertriglyceridemia, low high-density lipoprotein hyperlipidemia, and mixed hyperlipidemia (Beaumont et al., 1970; Lisak et al., 2013).
Hyperhomocysteinemia was diagnosed if the range of total plasma homocysteinemia concentration was 5–15 µM in an empty stomach. Abnormally high total homocysteinemia concentration is known as hyperhomocysteinemia (Petras et al., 2014).
Smoking: At least 1 cigarette every day for at least 1 year.
Drinking: At least twice every month for at least half the current year. Additionally, the amount of alcohol consumed was more than the standard amount of 120 mL wine, 360 mL beer, or 45 mL spirits.
(2) Evaluation criteria
1. Time from onset to arriving at the rehabilitation center and hospital stay; 2. Degree of disability, functional status in young stroke patients at admission, discharge, and 6 months after discharge. The Modified Rankin Scale was used to assess the degree of disability (score range: 0–6) (van Swieten et al., 1988). The Barthel Index was utilized to evaluate functional status of patients (Mahoney and Barthel, 1965; Muir et al., 2004) (independence: 95–100, slight dependence: 60–90, severe dependence: 0–55). 3. The Life Satisfaction Questionnaire (Lisat-11) (Röding et al., 2010; Bergström et al., 2011) was used to assess the degree of satisfaction with life at admission and 6 months after discharge. This included satisfaction in life on the whole, occupation, economy, entertainment, friendship, body, mind, and marital relationship. Score 0 represents nonapplication; scores 1–3 represent dissatisfied (1: very dissatisfied; 2: dissatisfied; 3: partially dissatisfied); scores 4–6 represent satisfied (4: partially satisfied; 5: satisfied; 6: very satisfied). 4. Rehabilitation items and intensity during hospitalization in young stroke patients.
Rehabilitation and intensity in young stroke patients
All patients in the young group received rehabilitation training, including physical therapy, occupational therapy, speech therapy, balance training, sports training, cognitive training, hyperbaric oxygen therapy, hydrotherapy, acupuncture, massage, suspension therapy, transcranial magnetic stimulation therapy, and biofeedback therapy. Physical therapy and occupational therapy were performed once or twice per day, each for 45 minutes, five times a week. Speech therapy, balance training, sports training, cognitive training, hyperbaric oxygen therapy, hydrotherapy, acupuncture, massage, and suspension therapy were conducted once a day, each for 30 minutes, five times a week. Transcranial magnetic stimulation therapy and biofeedback therapy were carried out once a day, each for 10 minutes, five times a week.
Follow-up
All patients in the young group were followed up at 6 months after discharge, and data were collected again for the Barthel Index, modified Rankin Scale scores, and Life Satisfaction Questionnaire.
Statistical analysis
All data were analyzed using SPSS 13.0 (SPSS, Chicago, IL, USA). Measurement data are expressed as the mean ± SD. The difference in Barthel Index for the young group at different time points was compared using a pairedt-test. Modified Rankin Scale scores were analyzed with paired rank sum test. The age between the two groups was analyzed using an independent samplest-test. Other general data and risk factors were analyzed with chi-square test. Usingt-tests to compare time from stroke to arrival at a rehabilitation center/hospital in two groups. Using a two-samples independentt-test to compare the difference in the amount the score changed between admission and discharge and between discharge and 6 months after discharge. AP≤ 0.05 was considered statistically significant using a two-sided test.
Results
General data
Of the 324 stroke patients who were hospitalized in the Department of Neurological Rehabilitation during the same period, 135 (41.7%) were young. From these, we randomly chose 100 for further analysis. The number of male patients was significantly greater than that of female patients (χ2= 3.889,P= 0.049). Young patients mainly suffered from hemorrhagic stroke (59.0%), but older patients were mainly affected by ischemic stroke (60.0%), showing significant differences between the two groups (P= 0.016). No significant difference in the hemiplegic side was detected between the two groups (P= 0.082). Education level was higher in the young group than in the middle-aged/older group (P= 0.013). The proportion of patients with medical insurance was similar between the two groups (P= 0.352). The main risk factors observed in young stroke patients were hypertension, drinking, smoking, hyperlipidemia, hyperhomocysteinemia, diabetes, previous history of stroke, and heart disease. The incidence of hyperhomocysteinemia was higher in the young group than in the middle-aged/ older group (P< 0.05). The incidences of hypertension, diabetes, and heart disease were higher in the middle-aged/older group than in the young group (P< 0.01;Table 1).
Rehabilitation
The course of diseases was similar between the two groups (P> 0.05), but mean hospital stay was longer in the younggroup than in the middle-aged/older group (P< 0.05;Table 2). Mean rehabilitation time was 2.5 hours per day in the young group, excluding family assistance and self-training. The most accepted training in the young group included physical therapy, occupational therapy, speech therapy and acupuncture (Table 3).
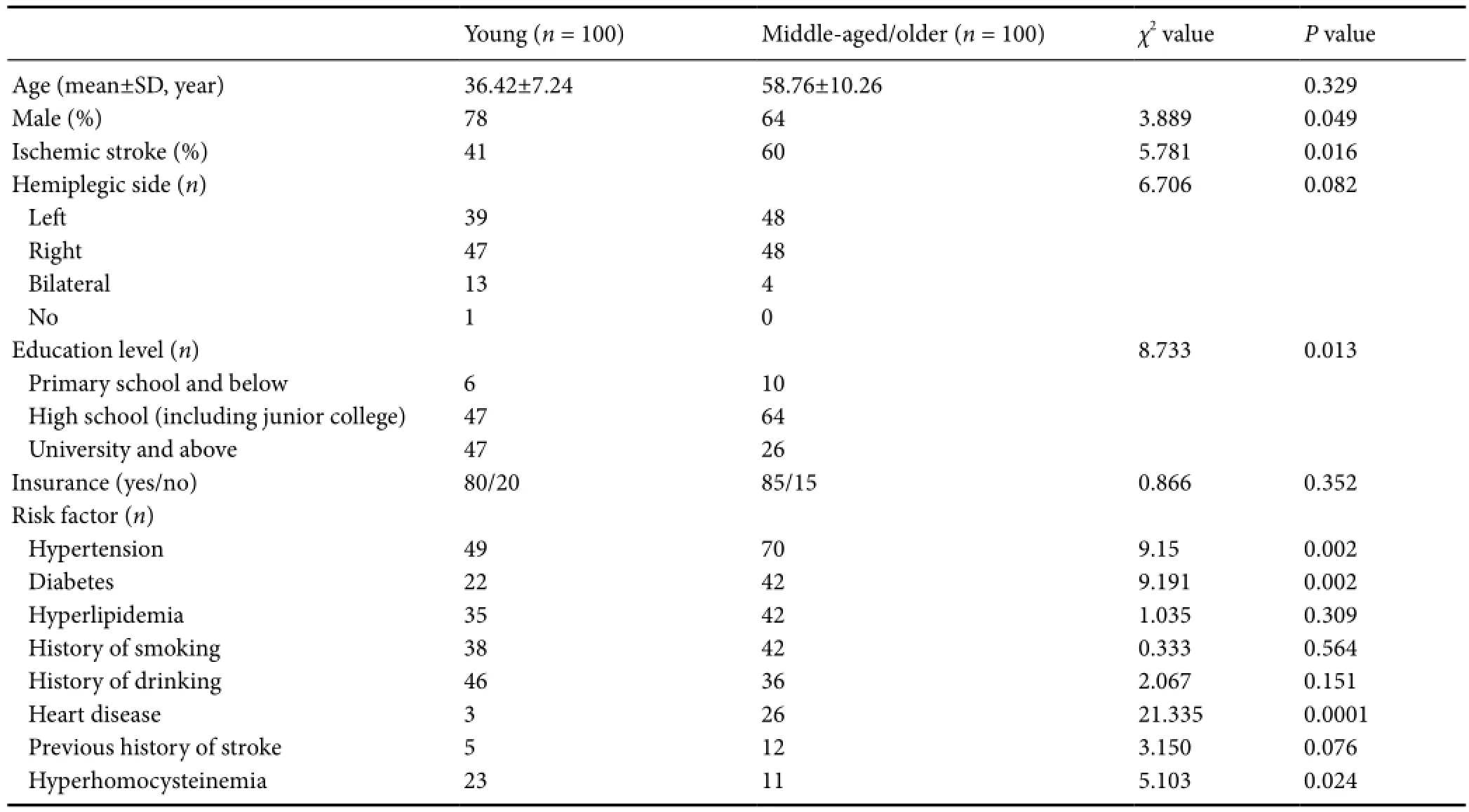
Table 1 General data of included stroke patients
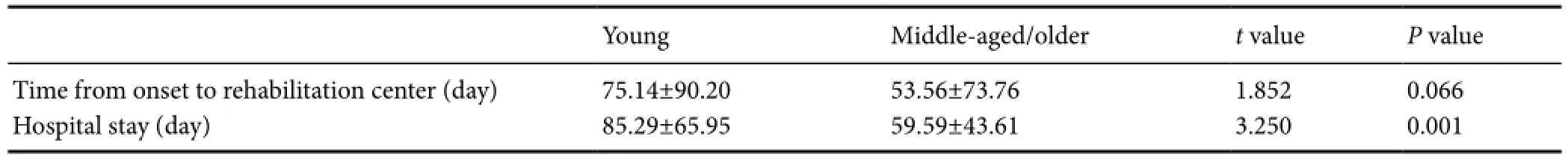
Table 2 Time from stroke to arrival at a rehabilitation center/hospital in young and middle-aged/older stroke patients

Table 5 Life satisfaction at admission and 6 months after discharge in young stroke patients
The degree of disability and functional status in young stroke patients
Barthel Index scores in the young group were significantly higher immediately after discharge than at admission (P< 0.05). Immediately after discharge, 13% of patients had achieved independence in daily life, 50% were slightly dependent, and37% were severely dependent. Barthel Index scores were higher 6 months after discharge than immediately after discharge (P< 0.05). At 6 months after discharge, 30% of patients had achieved independence in daily life, 53% were slightly dependent, and 17% were severely dependent (Table 4).
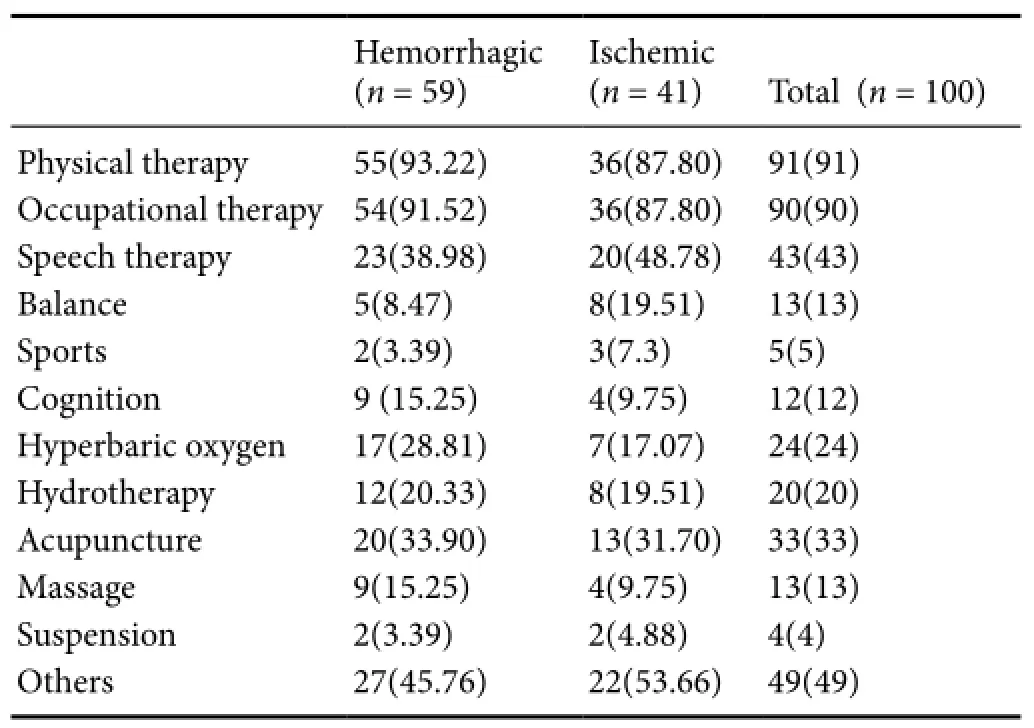
Table 3 Rehabilitation training items for young stroke patients
In the young group, comparison of conditions at discharge with those at admission showed that the functional status had improved in 47 patients, had not changed in 52 patients, and had worsened in 1 case (Z= –6.432,P= 0.000). Comparison of conditions 6 months after discharge with those immediately after discharge showed that stroke had improved in 41 patients, had not changed in 58 cases, and had become aggravated in 1 case (Z= –5.881,P= 0.000;Table 4).
We performed an analysis to determine how conditions after stroke changed over time. We calculated the change in Barthel Index between admission and discharge, and between discharge and 6 months after discharge. A pairedt-test showed that the amount of change in Barthel Index scores was significantly different (t= 4.006,P= 0.000) depending on the time period.
Changes in life satisfaction in young stroke patients
One hundred patients in the young group accepted a telephone follow-up 6 months after discharge. Excluding young patients with cognitive impairment, aphasia, or dysarthria, 30 patients finished the Life Satisfaction Questionnaire (Lisat-11). Results showed that compared with conditions at discharge, satisfaction in overall life, entertainment, friendship, sex life, self-care ability, spouse, physical health, and mental health had improved by 6 months after discharge, but that satisfaction in occupational and economic situations had decreased. Satisfaction in family life did not change (Table 5).
Young stroke patients returning to society 6 months after discharge
Among the 30 patients who completed the Life Satisfaction Questionnaire, eight had returned to work. Four had full-time jobs, one was working 50% of a normal work load, one was doing 75%, and two were doing 10–20%. Another seven were planning to return to work at 12 months after discharge.

Table 4 Self-care ability and disability in young stroke patients
Discussion
Among 100 young stroke patients in each group, 59% experienced hemorrhagic stroke. An epidemiological survey has reported that ischemic stroke was the primary stroke type detected in young stroke patients (Lee et al., 2002; Feigin et al., 2003). Inconsistent results may be related to an increased incidence of hypertension and heavy disability after intracerebral hemorrhage.
The risk factors for young stroke patients are complicated, and differ in developed and developing countries (Kwon et al., 2000; Cerrato et al., 2004; Dash et al., 2014). The onset of ischemic stroke was reported to be associated with hypertension, family history of stroke, and smoking in young patients of developing countries (Hill et al., 1991; Onwuchekwa et al., 2009). Our study demonstrated that hypertension is a high risk factor for young, middle-aged, and older stroke patients, and that the incidences of diabetes and heart disease were higher in the middle-aged/older group than in the young group, which was consistent with previous studies (Bevan et al., 1990; Tuomilehto et al., 1991; Carolei et al., 1993; Warlow, 1998; Chraa et al., 2014). The incidence of hyperhomocysteinemia was higher in the young group than in the middle-aged and elderly group, which was consistent with a previous study (Benninger et al., 2009). The number of drinkers was higher in the young group than in the middle-aged/older group. Recently, life pressure has increased for urban youth, and they stay out late at night, have anxiety, abuse drugs, and are more obese (Renna et al., 2014). Poor lifestyle and sleep apnea may also lead to an increasedincidence of stroke in young people, and risk factors have a long-term impact on the prognosis of young stroke patients (Ellekjaer et al., 2001; Kiyohara et al., 2003; Hardie et al., 2004; Waje-Andreassen et al., 2013).
Presently, few studies have been conducted on the shortterm and long-term prognosis of young stroke patients. For long-term follow-up, the Barthel Index can be used as a supplement for classifying the recovery of dysfunction using a modified Rankin Scale. The maximum sensitivity of the modified Rankin Scale is achieved 6 months after stroke (Cioncoloni et al., 2012). In this study, 13% of patients achieved independence in daily life, and 87% of patients had dysfunction at discharge. Six months after discharge, 70% of patients had dysfunction, and 57% with only moderate dysfunction (modified Rankin Scale score > 2), which was similar to what has been reported in other studies (Luengo-Fernandez et al., 2013; Synhaeve et al., 2014; Meyer et al., 2015).
Results from the Life Satisfaction Questionnaire (Lisat-11) in this study showed that satisfaction in overall life, entertainment, friendship, sex life, self-care ability, spouse, physical health, and mental health increased over time in young patients after discharge, but that satisfaction in occupational and economic situations decreased. A Swedish study found that independence in daily life markedly affected life satisfaction in young patients 1–2 years after stroke onset. However, even if daily life can be independent, some patients are still unable to work because they have difficulty maintaining attention or cannot drive to work, which decreases overall life satisfaction (Röding et al., 2010). Varona et al. (2004) reported that among 90% of young stroke patients with independent daily lives, only half returned to work, which impacts patients and family economics. Return to work positively affects life satisfaction (Vestling et al., 2005; Waje-Andreassen et al., 2013). The young patients with mild dysfunction, high education levels, and no risk factors are the most likely to return to work (Otero Palleiro and Barbagelata López, 2007; Trygged et al., 2011; Dash et al., 2014; Kawle et al., 2015). For patients who are mildly dependent in daily life, cognitive impairment, emotional disorders and aphasia impact their return to work. As a result, their degree of life satisfaction decreases. In the current study, among 100 young stroke patients, only 8 returned to work, and an additional 7 planned to work by 12 months after discharge. Even counting the additional 7, the proportion of patients returning to work was still low. The degree of life satisfaction was higher than that in previous studies, but could be attributed to the short discharge time, cultural differences, and family structure.
Currently, patients with acute stroke can be treated in a comprehensive or specialized hospital (Weaver and Liu, 2015). Nevertheless, there are few studies on rehabilitation programs and the costs for young stroke patients. Some patients with complications need specialized rehabilitation. Because rehabilitation hospitals are relatively few, only a small proportion of patients are treated. Our results confirmed that the average time from stroke onset to entering a rehabilitation center was 75.13 days. The average hospital stay was 85.29 days and the average time of rehabilitation training was 2.5 hours per day. These findings suggest that patients wait a long time for professional rehabilitation, and that the time of actual effective rehabilitation training is short. Patients outside Beijing primarily only receive physical therapy and occupational therapy, such as Chinese massage, acupuncture, and moxibustion. This might be related to advantages of traditional Chinese medicine and development of different rehabilitation medicine in different regions. This study has some limitations: (1) a small sample size; the patients in the middle-aged/older group were randomly selected. There may have been selection bias in the telephone follow-up. (2) Lack of imaging data might affect the statistical results and analysis. (3) Compulsory treatment, robot training, music therapy, and motor imagery were not analyzed, but these items may have effects on functional status (Rabadi, 2011).
We will continue to focus on the situation of rehabilitation training, medication, returning to society or not, working problems, family living conditions, specialized rehabilitation nursing and factors influencing life satisfaction.
Declaration of patient consent:The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/ have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Author contributions:XXD designed this study, and obtained the funding. CJZL wrote the paper, analyzed and ensured the integrity of the data. KY analyzed the data. LPS and TZ served as a principle investigator. PKL performed statistical analysis. QW, RS, XLL and HYL collected scale data. All authors approved the final version of the paper.
Conflicts of interest:None declared.
Supplementary information:Supplementary data associated with this article can be found, in the online version, by visiting www.nrronline.org.
Plagiarism check:This paper was screened twice using CrossCheck to verify originality before publication.
Peer review:This paper was double-blinded and stringently reviewed by international expert reviewers.
Béjot Y, Daubail B, Giroud M (2013) Epidemiology and prognosis of stroke in young adults. Rev Prat 63:926-929.
Beaumont JL, Carlson LA, Cooper GR, Fejfar Z, Fredrickson DS, Strasser T (1970) Classification of hyperlipidaemias and hyperlipoproteinaemias. Bull World Health Organ 43:891-915.
Benninger DH, Herrmann FR, Georgiadis D, Kretschmer R, Sarikaya H, Schiller A, Baumgartner RW (2009) Increased prevalence of hyperhomocysteinemia in cervical artery dissection causing stroke: a case-control study. Cerebrovasc Dis 27:241-246.
Bergström AL, Eriksson G, von Koch L, Tham K (2011) Combined life satisfaction of persons with stroke and their caregivers: associations with caregiver burden and the impact of stroke. Health Qual Life Outcomes 9:1.
Bevan H, Sharma K, Bradley W (1990) Stroke in young adults. Stroke 21:382-386.
Bi Q, Beijing Neurdogist Club (2003) Study on the risk factors among stroke in young people. Zhonghua Liu Xing Bing Xue Za Zhi 24:106-108.
Carolei A, Marini C, Ferranti E, Frontoni M, Prencipe M, Fieschi C (1993) A prospective study of cerebral ischemia in the young. Analysis of pathogenic determinants. The National Research Council Study Group. Stroke 24:362-367.
Cerrato P, Grasso M, Imperiale D, Priano L, Baima C, Giraudo M, Rizzuto A, Azzaro C, Lentini A, Bergamasco B (2004) Stroke in young patients: etiopathogenesis and risk factors in different age classes. Cerebrovasc Dis 18:154-159.
Chalmers J (1999) The 1999 WHO-ISH Guidelines for the Management of Hypertension. Med J Aust 171:458-459.
Chraa M, Louhab N, Kissani N (2014) Stroke in young adults: about 128 cases. Pan Afr Med J 17:37.
Cioncoloni D, Piu P, Tassi R, Acampa M, Guideri F, Taddei S, Bielli S, Martini G, Mazzocchio R (2012) Relationship between the modified Rankin Scale and the Barthel Index in the process of functional recovery after stroke. NeuroRehabilitation 30:315-322.
Dash D, Bhashin A, Pandit Ak, Tripathi M, Bhatia R, Prasad K, Padma MV (2014) Risk factors and etiologies of ischemic strokes in young patients: a tertiary hospital study in north India. J Stroke 16:173-177.
De Silva R, Gamage R, Wewelwala C, Gunarathna D, Kittner S, Sirisena D, Weerasinghe A, Amarasinghe P (2009) Young strokes in Sri Lanka: An unsolved problem. J Stroke Cerebrovasc Dis 18:304-308.
Ellekjaer H, Holmen J, Vatten L (2001) Blood pressure, smoking and body mass in relation to mortality from stroke and coronary heart disease in the elderly. A 10-year follow-up in Norway. Blood Press 10:156-163.
Engbers LH, Vollenbroek-Hutten MM, van Harten WH (2005) A comparison of patient characteristics and rehabilitation treatment content of chronic low back pain (CLBP) and stroke patients across six European countries. Health Policy 71:359-373.
Feigin VL, Lawes CM, Bennett DA, Anderson CS (2003) Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20thcentury. The Lancet Neurology 2:43-53.
Fraker TD et al. (2007) 2007 chronic angina focused update of the ACC/AHA 2002 guidelines for the management of patients with chronic stable angina: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines Writing Group to develop the focused update of the 2002 guidelines for the management of patients with chronic stable angina. J Am Coll Cardiol 50:2264-2274.
Griffiths D, Sturm J (2011) Epidemiology and etiology of young stroke. Stroke Res Treat 2011:209370.
Hardie K, Hankey GJ, Jamrozik K, Broadhurst RJ, Anderson C (2004) Ten-year risk of first recurrent stroke and disability after first-ever stroke in the Perth Community Stroke Study. Stroke 35:731-735.
Hill DJ, White VM, Gray NJ (1991) Australian patterns of tobacco smoking in 1989. Med J Aust 154:797-801.
Joint Committee for Developing Chinese guidelines on Prevention and Treatment of Dyslipidemia in Adults (2007) Chinese guidelines on prevention and treatment of dyslipidemia in adults. Zhonghua Xin Xue Guan Bing Za Zhi 35:390-419.
Kawle AP, Nayak AR, Lande NH, Kabra DP, Chandak NH, Badar SR, Raje DV, Taori GM, Daginawala HF, Kashyap RS (2015) Comparative evaluation of risk factors, outcome and biomarker levels in young and old acute ischemic stroke patients. Ann Neurosci 22:70-77.
Kiyohara Y, Kubo M, Kato I, Tanizaki Y, Tanaka K, Okubo K, Nakamura H, Iida M (2003) Ten-year prognosis of stroke and risk factors for death in a Japanese community: the Hisayama study. Stroke 34:2343-2347.
Kuptniratsaikul V, Kovindha A, Massakulpan P, Permsirivanich W, Kuptniratsaikul PS (2009) Inpatient rehabilitation services for patients after stroke in Thailand: a multi-centre study. J Rehabil Med 41:684-686.
Kwon SU, Kim JS, Lee JH, Lee MC (2000) Ischemic stroke in Korean young adults. Acta Neurol Scand 101:19-24.
Lee TH, Hsu WC, Chen CJ, Chen ST (2002) Etiologic study of young ischemic stroke in Taiwan. Stroke 33:1950-1955.
Lisak M, Demarin V, Trkanjec Z, Basić-Kes V (2013) Hypertriglyceridemia as a possible independent risk factor for stroke. Acta Clin Croat 52:458-463.
Luengo-Fernandez R, Paul NLM, Gray AM, Pendlebury ST, Bull LM, Welch SJV, Cuthbertson FC, Rothwell PM (2013) Population-based study of disability and institutionalization after transient ischemic attack and stroke: 10-year results of the Oxford Vascular Study. Stroke 44:2854-2861.
Mahoney FI, Barthel DW (1965) Functional evaluation: the barthel index. Md State Med J 14:61-65.
Meyer S, Verheyden G, Brinkmann N, Dejaeger E, De Weerdt W, Feys H, Gantenbein AR, Jenni W, Laenen A, Lincoln N, Putman K, Schuback B, Schupp W, Thijs V, De Wit L (2015) Functional and motor outcome 5 years after stroke is equivalent to outcome at 2 months: follow-up of the collaborative evaluation of rehabilitation in stroke across Europe. Stroke 46:1613-1619.
Muir KW, Lees KR, Ford I, Davis S, Intravenous Magnesium Efficacy in Stroke (IMAGES) Study Investigators (2004) Magnesium for acute stroke (Intravenous Magnesium Efficacy in Stroke trial): randomised controlled trial. Lancet 363:439-445.
No authors listed (1988) The World Health Organization MONICA Project (monitoring trends and determinants in cardiovascular disease): a major international collaboration. WHO MONICA Project Principal Investigators. J Clin Epidemiol 41:105-114.
Onwuchekwa AC, Onwuchekwa RC, Asekomeh EG (2009) Stroke in young Nigerian adults. J Vasc Nurs 27:98-102.
Otero Palleiro MM, Barbagelata López C (2007) Etiologic subtypes of ischemic stroke in young adults aged 18 to 45 years: a study of a series of 93 patients. Rev Clin Esp 207:158-165.
Park WB, Cho JS, Shin SD, Kong SY, Kim JJ, Lim YS, Yang HJ, Lee G (2014) Comparison of epidemiology, emergency care, and outcomes of acute ischemic stroke between young adults and elderly in Korean population: a multicenter observational study. J Korean Med Sci 29:985-991.
Petras M, Tatarkova Z, Kovalska M, Mokra D, Dobrota D, Lehotsky J, Drgova A (2014) Hyperhomocysteinemia as a risk factor for the neuronal system disorders. J Physiol Pharmacol 64:15-23.
Röding J, Glader EL, Malm J, Lindström B (2010) Life satisfaction in younger individuals after stroke: different predisposing factors among men and women. J Rehabil Med 42:155-161.
Rabadi MH (2011) Review of the randomized clinical stroke rehabilitation trials in 2009. Med Sci Monit 17:RA25-RA43.
Rapezzi C, Biagini E, Branzi A (2008) Guidelines for the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes: the task force for the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes of the European Society of Cardiology. Eur Heart J 29:277-278.
Renna R, Pilato F, Profice P, Della Marca G, Broccolini A, Morosetti R, Frisullo G, Rossi E, De Stefano V, Di Lazzaro V (2014) Risk factor and etiology analysis of ischemic stroke in young adult patients. J Stroke Cerebrovasc Dis 23:e221-e227.
Sultan S, Elkind MS (2013) The growing problem of stroke among young adults. Curr Cardiol Rep 15:421.
Synhaeve NE, Arntz RM, Maaijwee NAM, Rutten-Jacobs LCA, Schoonderwaldt HC, Dorresteijn LDA, de Kort PLM, van Dijk EJ, de Leeuw FE (2014) Poor long-term functional outcome after stroke among adults aged 18 to 50 years: Follow-Up of Transient Ischemic Attack and Stroke Patients and Unelucidated Risk Factor Evaluation (FUTURE) study. Stroke 45:1157-1160.
Tombaugh TN, McIntyre NJ (1992) The mini-mental state examination: a comprehensive review. J Am Geriatr Soc 40:922-935.
Trygged S, Ahacic K, Kåreholt I (2011) Income and education as predictors of return to working life among younger stroke patients. BMC Public Health 11:742.
Tuomilehto J, Bonita R, Stewart A, Nissinen A, Salonen JT (1991) Hypertension, cigarette smoking, and the decline in stroke incidence in eastern Finland. Stroke 22:7-11.
van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J (1988) Interobserver agreement for the assessment of handicap in stroke patients. Stroke 19:604-607.
Varona JF, Bermejo F, Guerra JM, Molina JA (2004) Long-term prognosis of ischemic stroke in young adults. Study of 272 cases. J Neurol 251:1507-1514.
Vestling M, Ramel E, Iwarsson S (2005) Quality of life after stroke: well-being, life satisfaction, and subjective aspects of work. Scand J Occup Ther 12:89-95.
Waje-Andreassen U, Thomassen L, Jusufovic M, Power KN, Eide GE, Vedeler CA, Naess H (2013) Ischaemic stroke at a young age is a serious event – final results of a population-based long-term follow-up in Western Norway. Eur J Neurol 20:818-823.
Warlow CP (1998) Epidemiology of stroke. Lancet 352 Suppl 3:SIII1-4.
Weaver J, Liu KJ (2015) Does normobaric hyperoxia increase oxidative stress in acute ischemic stroke? A critical review of the literature. Med Gas Res 5:11.
World Health Organization (2006) Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia. Report of a WHO/IDF consultation.
Copyedited by Phillips A, Maxwell R, Yu J, Li CH, Qiu Y, Song LP, Zhao M
*Correspondence to: Xiao-xia Du, M.D., 364906784@qq.com.
orcid: 0000-0001-7944-2474 (Xiao-xia Du)
10.4103/1673-5374.194746
Accepted: 2016-02-06
- 中国神经再生研究(英文版)的其它文章
- The status of Nrf2-based therapeutics: current perspectives and future prospects
- Targeting neuronal nitric oxide synthase as a valuable strategy for the therapy of neurological disorders
- Six psychotropics for pre-symptomatic & early Alzheimer’s (MCI), Parkinson’s, and Huntington’s disease modification
- Applicability of tooth derived stem cells in neural regeneration
- Cortical spreading depression-induced preconditioning in the brain
- Neuroinflammation, neurodegeneration and regeneration in multiple sclerosis: intercorrelated manifestations of the immune response

