Reversing multiple age-related pathologies by controlling the senescence-associated secretory phenotype of stem cells
Reversing multiple age-related pathologies by controlling the senescence-associated secretory phenotype of stem cells
Regenerative medicine by cell transplantation is a novel therapy for treating end-stage organ failure and tissue damage. Cell-based therapy based on the transplantation of neural stem/progenitor cells (NSPCs) represents an attractive strategy for the treatment of neurodegenerative diseases, but obtaining large numbers of these cells is difficult and their differentiation potential is strictly restricted in a spatiotemporally-regulated manner during central nervous system (CNS) development. Therefore, embryonic stem cells and induced pluripotent stem cells represent an attractive alternative for cell-transplantation therapy in regenerative medicine. The direct reprograming of astrocytes into neurons is also under investigation as another approach. However, these alternative approaches are hampered by the current lack of selective and efficient differentiation methods and transplanted cell tumorigenicity.
Mesenchymal stem/stromal cells (MSCs) have drawn attention as a source of various regenerative factors. For instance, TNF-α-stimulated protein 6 (TSG-6), monocyte chemoattractant protein-1 (MCP-1), and the ectodomain of sialic acid-binding Ig-like lectin-9 (Siglec-9) are anti-inflammatory factors secreted by MSCs (Lee et al., 2009; Matsubara et al., 2015). However, despite many reports describing the trophic effects of MSCs, no critical regenerative factors have been identified. In a recent study, we identified growth differentiation factor 6 (Gdf6; also known as Bmp13 and CDMP-2), a member of the transforming growth factor-β (TGF-β) superfamily, as a regenerative factor secreted by young MSCs (Hisamatsu et al., 2016). Upregulation of Gdf6 restored the differentiation capacity of old MSCsin vitroand exerted beneficial effectsin vivoon age-associated pathologies of multiple tissues, including the decline in neurogenesis and reduction in the number of Sox2-positive (Sox2+) neural progenitors and doublecortin (dcx)+neuroblasts (Figure 1).
miR-17 overexpression reverses the age-related functional disorders of MSCs:Senescent cells secrete various inflammatory cytokines, chemokines, and proteases, a phenotype termed the senescence-associated secretory phenotype (SASP) (Coppe et al., 2008). Although MSCs are a well-known source of various secretory factors, the changes that occur in the secretory properties of MSCs with age remain largely unclear. Therefore, we decided to compare the secretion profiles of purified MSCs (CD45–, CD31–, Ter119–, Pdgfra+and Sca-1+) that were isolated from young (2–3 months) and old (> 18 months) mice. Old MSCs expressed higher levels of representative inflammatory factors, such as interleukin 6, Gro1, and Gmcsf, and exhibited significant changes in the expression of several growth factors, as well as a decline in osteogenic and adipogenic differentiation potential and upregulation of a representative cellular senescence marker p21 and senescence-associated β-galactosidase activity (SA-β-gal). To obtain a global view of the expression profiles, we performed microarray and microRNA (miRNA) quantitative PCR (qPCR) array analyses of young and old MSCs. We identified secretary factors that were highly upregulated in young MSCs and downregulated in old MSCs. Consistent with previous reports, expression of miR-17 family members (miR-17, -18a, -19a/b, -20a/b, -25, -93, -92a, -106a/b, and -363) was downregulated in old MSCs. miRNA, a member of the non-coding family of RNAs with a typical length of 21–25 nucleotides, regulates gene expressions at the post-transcriptional level by binding to the 3′-untranslated regions of target mRNAs. In our previous reports, we identified miR-17 as a key regulator of the neurogenic-to-gliogenic transition in developing NSPCs (Naka-Kaneda et al., 2014) and demonstrated that its overexpression inhibited the acquisition of gliogenic competence and restored neuropotency in developmental stage-progressed gliogenic NSPCs. However, the effects of miR-17 on age-related changes in MSC properties remained unclear. As observed in NSPCs, we found that miR-17 overexpression restored the osteogenic and adipogenic potential of old MSCs. Moreover, transplantation of miR-17-overexpressing old MSCsviaintravenous injection attenuated age-dependent loss of B cells and improved the aged-associated myeloid skewing phenotype. Moreover, the transplanted cells were engrafted in lungs, but not in bone marrow, where is the place for hematopoiesis by hematopoietic stem cells, consistent with previous study (Lee et al., 2009; Mabuchi et al., 2013). Therefore, we hypothesized that the beneficial effect of MSC transplantation on lymphopoiesis was due to a secretory factor derived from the transplanted miR17-overexpressing MSCs.
Gdf6 ameliorates age-related pathologies in brain:To identify the critical secretory factors that restored lymphopoiesis in the MSC-transplantation experiments, we compared the gene expression profiles of young, old and miR-17-overexpressing old MSCs by microarray analyses in combination with Gene Ontology analyses. The results revealed 13 factors whose expression was restored by miR-17 overexpression in old MSCs. To evaluate these factors further, we generated conditioned media (CM) produced from 293T cells expressing each candidate factor and used them to determine which factor was specifically responsible for the restoration of lymphopoiesis by adding each one individually to osteogenic differentiation media. As a result, Gdf6 was identified as an osteogenesis-promoting factor in old MSCs. We also confirmed that Gdf6 expression depended on miR-17 expression by performing a loss-of-function experiment of miR-17 and its prologs miR-106a/b using a RNA decoy inhibitor.
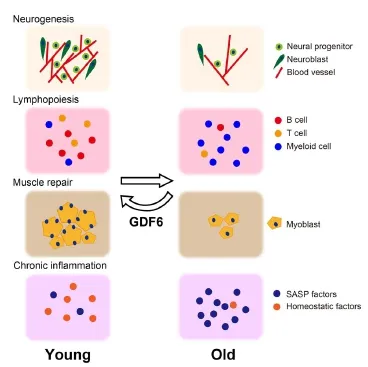
Figure 1 Scheme of reversing multiple age-related pathologies by upregulation of growth differentiation factor 6 (Gdf6).
Next, to confirm that Gdf6 was responsible for the restoration of lymphopoiesis in aged mice transplanted with old MSCs overexpressing miR-17, we transduced human GDF6 (hGDF6) into 20-month-old mice by intraperitoneal lentivirus injection. Thelentivirus infected cells in the peritoneum, subcutaneous adipose tissue, and a part of intestine, but not peripheral blood (PB) cells, and the upregulation of plasma level of hGDF6 sustained over 16 weeks. Although the plasma level of the active form of endogenous Gdf6 increased with age, its level was further increased by hGDF6 overexpression. hGDF6-overexpressing old mice also showed lymphocyte numbers similar to those of young mice.
Recently, GDF11, another member of the TGF-β superfamily, was identified as a regenerative factor that improves age-related pathologies including cardiac hypertrophy, insufficient muscle repair, and reduced neurogenesis (Loffredo et al., 2013; Katsimpardi et al., 2014; Sinha et al., 2014). Accordingly, we confirmed the effects of hGDF6 overexpression on neurogenesis in old brain. Overexpression of hGDF6 was effective in attenuating the age-dependent decrease in Sox2+neural progenitors expressed in wide brain regions, such as the subventricular zone (SVZ) and striatum. Moreover, the number of Dcx+neuroblasts in the SVZ of old mice overexpressing hGDF6 was higher than that in the brains of old control mice, and the improvements in the cerebrovascular networks of hGDF6-overexpressing old mice were similar to those of GDF11-injected mouse brains.
Gdf6 attenuates age-related pathologies in multiple tissues:Gdf6 overexpression in old mice had further beneficial effects on other age-related pathologies, such as its ability to increase the muscle repair capacity of tibialis anterior muscles (Hisamatsu et al., 2016). To clarify this effect, we injected cardiotoxin into the tibialis anterior muscles of hGDF6 overexpressing old mice, and evaluated muscle repair capacity by analyzing the formation of embryonic myosin heavy chain-positive (eMHC+) mononuclear myoblasts. Moreover, the eMHC+myotubes increased in hGDF6 overexpressing old mice, similarly to the results in young mice.
Previous studies demonstrate that some inflammatory SASP factors are systemically upregulated with age and impair tissue homeostasis. For instance, age-dependent increases in plasma levels of CCL11 and β2-microgloblin impair hippocampal neurogenesis and cognitive function, and C1q-mediated activation of Wnt-signaling impairs muscle repair by causing the dysfunction of skeletal muscle satellite cells (Villeda et al., 2011; Naito et al., 2012; Smith et al., 2015). Therefore, we investigated the plasma levels of various inflammatory factors by using luminex analysis. The results revealed that hGDF6 overexpression reduces plasma cytokine levels including SASP factors such as IL-6, IL1β, and CCL5, indicating that upregulation of hGDF6 suppresses chronic inflammation. Chronic inflammation accelerates systemic aging (Jurk et al., 2014). Taken together, the results suggest that attenuation of chronic inflammationviathe upregulation of a single factor GDF6 represents a possible mechanism for the repair of age-related pathologies in multiple tissues (Figure 1).
Conclusions:SASP and stem cell aging constitute two emerging mechanisms for connecting cellular senescence to tissue dysfunction. The study of the age-related changes in the secretory properties of MSCs has provided new insights into the SASP of stem cells. One aspect of SASP, namely upregulation of diverse inflammatory factors, has attracted an inordinate amount of attention; however, downregulation of homeostatic factors equally contributes to the induction of age-related cellular dysfunctions and, in turn, tissue level disorders. Additionally, certain growth factors can compensate for age-related reductions in homeostatic factors and assist in recovery from geriatric disorders; however, despite their potential importance, the nature of the underlying mechanisms remains largely unclear. A better understanding of the mechanisms underlying the regenerative effects of GDF6 in multiple tissues should lead to the development of novel therapeutic agents for the treatment of age-related disorders.
Daisuke Hisamatsu, Hayato Naka-Kaneda*
Laboratory for Stem Cell Competency, RIKEN Center for Integrative Medical Sciences (IMS), Kanagawa, Japan (Hisamatsu D, Naka-Kaneda H)
Department of Physiology, Keio University School of Medicine, Tokyo, Japan (Hisamatsu D)
*Correspondence to: Hayato Naka-Kaneda,Ph.D., hayato.kaneda@riken.jp.
Accepted:2016-11-04
Coppe JP, Patil CK, Rodier F, Sun Y, Munoz DP, Goldstein J, Nelson PS, Desprez PY, Campisi J (2008) Senescence-associated secretory phenotypes reveal cell-nonautonomous functions of oncogenic RAS and the p53 tumor suppressor. PLoS Biol 6:2853-2868.
Hisamatsu D, Ohno-Oishi M, Nakamura S, Mabuchi Y, Naka-Kaneda H (2016) Growth differentiation factor 6 derived from mesenchymal stem/stromal cells reduces age-related functional deterioration in multiple tissues. Aging (Albany NY) 8:1259-1275.
Jurk D, Wilson C, Passos JF, Oakley F, Correia-Melo C, Greaves L, Saretzki G, Fox C, Lawless C, Anderson R, Hewitt G, Pender SL, Fullard N, Nelson G, Mann J, van de Sluis B, Mann DA, von Zglinicki T (2014) Chronic inflammation induces telomere dysfunction and accelerates ageing in mice. Nat Commun 2:4172.
Katsimpardi L, Litterman NK, Schein PA, Miller CM, Loffredo FS, Wojtkiewicz GR, Chen JW, Lee RT, Wagers AJ, Rubin LL (2014) Vascular and neurogenic rejuvenation of the aging mouse brain by young systemic factors. Science 344:630-634.
Lee RH, Pulin AA, Seo MJ, Kota DJ, Ylostalo J, Larson BL, Semprun-Prieto L, Delafontaine P, Prockop DJ (2009) Intravenous hMSCs improve myocardial infarction in mice because cells embolized in lung are activated to secrete the anti-inflammatory protein TSG-6. Cell Stem Cell 5:54-63.
Loffredo FS, Steinhauser ML, Jay SM, Gannon J, Pancoast JR, Yalamanchi P, Sinha M, Dall’Osso C, Khong D, Shadrach JL, Miller CM, Singer BS, Stewart A, Psychogios N, Gerszten RE, Hartigan AJ, Kim MJ, Serwold T, Wagers AJ, Lee RT (2013) Growth differentiation factor 11 is a circulating factor that reverses age-related cardiac hypertrophy. Cell 153:828-839.
Mabuchi Y, Morikawa S, Harada S, Niibe K, Suzuki S, Renault-Mihara F, Houlihan DD, Akazawa C, Okano H, Matsuzaki Y (2013) LNGFR(+)THY-1(+)VCAM-1(hi+) cells reveal functionally distinct subpopulations in mesenchymal stem cells. Stem Cell Rep 1:152-165.
Matsubara K, Matsushita Y, Sakai K, Kano F, Kondo M, Noda M, Hashimoto N, Imagama S, Ishiguro N, Suzumura A, Ueda M, Furukawa K, Yamamoto A (2015) Secreted ectodomain of sialic acid-binding Ig-like lectin-9 and monocyte chemoattractant protein-1 promote recovery after rat spinal cord injury by altering macrophage polarity. J Neurosci 35:2452-2464.
Naito AT, Sumida T, Nomura S, Liu ML, Higo T, Nakagawa A, Okada K, Sakai T, Hashimoto A, Hara Y, Shimizu I, Zhu W, Toko H, Katada A, Akazawa H, Oka T, Lee JK, Minamino T, Nagai T, Walsh K, et al. (2012) Complement C1q activates canonical Wnt signaling and promotes aging-related phenotypes. Cell 149:1298-1313.
Naka-Kaneda H, Nakamura S, Igarashi M, Aoi H, Kanki H, Tsuyama J, Tsutsumi S, Aburatani H, Shimazaki T, Okano H (2014) The miR-17/106-p38 axis is a key regulator of the neurogenic-to-gliogenic transition in developing neural stem/ progenitor cells. Proc Natl Acad Sci U S A 111:1604-1609.
Sinha M, Jang YC, Oh J, Khong D, Wu EY, Manohar R, Miller C, Regalado SG, Loffredo FS, Pancoast JR, Hirshman MF, Lebowitz J, Shadrach JL, Cerletti M, Kim MJ, Serwold T, Goodyear LJ, Rosner B, Lee RT, Wagers AJ (2014) Restoring systemic GDF11 levels reverses age-related dysfunction in mouse skeletal muscle. Science 344:649-652.
Smith LK, He Y, Park JS, Bieri G, Snethlage CE, Lin K, Gontier G, Wabl R, Plambeck KE, Udeochu J, Wheatley EG, Bouchard J, Eggel A, Narasimha R, Grant JL, Luo J, Wyss-Coray T, Villeda SA (2015) beta2-microglobulin is a systemic pro-aging factor that impairs cognitive function and neurogenesis. Nat Med 21:932-937.
Villeda SA, Luo J, Mosher KI, Zou B, Britschgi M, Bieri G, Stan TM, Fainberg N, Ding Z, Eggel A, Lucin KM, Czirr E, Park JS, Couillard-Després S, Aigner L, Li G, Peskind ER, Kaye JA, Quinn JF, Galasko DR, et al. (2011) The ageing systemic milieu negatively regulates neurogenesis and cognitive function. Nature 477:90-94.
10.4103/1673-5374.194715
How to cite this article:Hisamatsu D, Naka-Kaneda H (2016) Reversing multiple age-related pathologies by controlling the senescence-associated secretory phenotype of stem cells. Neural Regen Res 11(11):1746-1747.
Open access statement: This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
- 中国神经再生研究(英文版)的其它文章
- The status of Nrf2-based therapeutics: current perspectives and future prospects
- Targeting neuronal nitric oxide synthase as a valuable strategy for the therapy of neurological disorders
- Six psychotropics for pre-symptomatic & early Alzheimer’s (MCI), Parkinson’s, and Huntington’s disease modification
- Applicability of tooth derived stem cells in neural regeneration
- Cortical spreading depression-induced preconditioning in the brain
- Neuroinflammation, neurodegeneration and regeneration in multiple sclerosis: intercorrelated manifestations of the immune response

