Clinical assessment indicators of postpartum hemorrhage:A systematic review☆
Ying Liu ,Ying Shen ,Wei Zhu ,Jing-Bo Qiu ,Qun Hung ,*,Wen-Qin Ye
aThe International Peace Maternity&Child Health Hospital Af f i liated to Shanghai Jiao Tong University,Shanghai 200030,China
bNursing Department,Changhai Hospital Af f i liated to the Second Military Medical University,Shanghai 200433,China
1.Introduction
Postpartum hemorrhage(PPH)leads to prominent causes of maternal death.The WHO estimated that the total number of maternal deaths worldwide is over 3 million and that severe blood loss,infection,hypertension,complications of pregnancy and unsafe abortion account for 75%of such deaths.1Although the incidence of severe PPH is decreasing,it remains a huge threat to both the mother and the health care personnel.
PPH has been defined as“the amount of blood loss over 500 ml in natural vaginal delivery,or 1000 mL in cesarean section,within a period of 24 h postpartum”.2However,this definition tends to be retrospective.Thus,PPH can only be diagnosed if the parturient has lost more than 500 mL or 1000 mL of blood.Another limitation of diagnosing PPH is that no ideal method to precisely calculate how much blood has been lost has been reported to date.3Visual estimation,which is the most convenient method of blood loss estimation,underestimates blood loss by half the actual amount.4The Hb or HCT method has a delayed effect since intensive hemorrhage might cause the blood to concentrate in a short time,leading to a false impression that the value is within normal limits.Although the National Postpartum Hemorrhage Control Group in China has suggested that the gravimetrical method and volume method be combined as a routine measurement,the heavy workload in the delivery rooms makes this recommendation impractical on the basis of such a large population.Therefore,some professionals suggest that other clinical indicators should be assessed to provide an early warning of the severity of the hemorrhage.Although guidelines5-7of PPH have been constantly updated,a detailed maternal assessment is never emphasized.Instead,these guidelines mainly presented recommendations on PPH prevention andintervention practices.Evidence demonstrates that timely assessment of vital signs can reduce the symptom-to-intervention period in those who experience PPH and significantly improve postintervention outcomes.8Early identi fication permits early intervention.
Clinical signs and symptoms are closely related to the severity of blood loss irrespective of the normal or maternal population.It is commonly believed that vital signs are of great value for assessment,but they remain unchangeable until mild shock is present.In addition to vital signs,other indicators,such as the fundus position and the hardness of the uterus,are routinely assessed in the postpartum period.The main indicators,the time interval of assessment and the thresholds of different severity of blood loss are basically formulated with clinical experience from the obstetricians and midwives.A systematic review revealed the relationship between shock index and blood loss among 9 indicators,including heart rate,systolic blood pressure,shock index,prehospital systolic blood pressure,mean arterial pressure,diastolic blood pressure,pulse pressure,body temperature and respiratory rate.9Nevertheless,the included articles focus mainly on trauma patients or maternal patients with other complications,such as ectopic pregnancy.Two other reviews that focused on hemostatic monitoring suggested the lack of conclusive evidence for optimal hemostatic resuscitation but arrived at the notion that viscoelastic hemostatic assays were useful for rapid assessment in treating PPH,including thrombelastography-or thromboelastometry-based tests.10,11A reduction in fibrinogen played a major role in PPH and could be considered an early predictor of the worsening of a patient's condition.12To our knowledge,maternal hemodynamic features differ from the non-pregnant population,indicating the necessity of postpartum assessment for this population.Thus,due to the lack of consensus on what clinical indicators should be assessed and the speci fic time point of each indicator signifying potential PPH,we conducted this review to identify clinical parameters that are essential for postpartum assessment to prompt health care providers of early warnings of PPH.
2.Materials and methods
The Preferred Reporting Items for Systematic reviews and Meta-Analyses(PRISMA)statement13and the Meta-Analysis of Observational Studies in Epidemiology(MOOSE)guidelines14were adopted in this systematic review.
2.1.Inclusion and exclusion criteria
Focused on the PPH population,all studies included met the following criteria:relationship between the assessment indicators and loss of blood should be explored,both prospectively and retrospectively;types of studies were observational;both English and Chinese studies were included.Articles were omitted because the indicator results or the severity of blood loss were excluded.Studies exclusively focused on hemostasis exclusively were not considered given that similar reviews exist.
2.2.Searching strategies
Before systematic search of primary studies related to assessment indicators,the Cochrane Library was searched to ensure that no systematic review was reported for this particular topic.Then,a literature search was conducted to identify articles published in PubMed,EMBASE,ProQuest,Springer,Elsevier,CINAHL,CBM(China Biology Medicine),CNKI(China National Knowledge Infrastructure)and Wanfang Databases from the establishment of each database to December 2016.Terms used to retrieve articles included“(postpartum hemorrhage/postpartum hemorrhage)&assess*&(vital signs/heart rate/blood pressure/temperature/respiratory rate/consciousness/oxygen saturation/urine output/shock/uterine contraction/fundus/birth canal injury/lower genital tract laceration/placenta completeness/placenta examination/laboratory test)”.In addition,important references of selected articles were considered for a complementary search.
2.3.Literature screening and critical appraisal
Two reviewers who were trained to conduct evidence-based nursing research independently read the title and abstract of each article.If inclusion criteria were met,we further reviewed the full article.Retained studies were crosschecked.After literature screening,the quality of those selected studies was judged by the two reviewers based on the 22-item Strengthening the Reporting of Observational Studies in Epidemiology(STROBE)Statement.15A third reviewer was involved if there were any disputation throughout the critical appraisal.
2.4.Data extraction and analysis
A data extraction sheet was identi fied to transfer the data of each selected study.The sheet contained the following information:author,year of publication,region of research,population,sample size,mode of delivery,treatment after delivery,severity of blood loss,indicators and its measurement,results of the relationship between assessment indicators and blood loss.The meta-analysis was not conducted given that most included studies did not share a common format of quantitative analysis.For example,both Lin's16and Lin's17studies recorded the heart rate(HR),blood pressure(BP),hemoglobin(Hb)and hematocrit(HCT),but accurate HR and BP data were not reported,and the reported times of Hb and HCT differed.Therefore,only a descriptive discussion is provided.
3.Results
A total of 2319 citations were identi fied throughout the search process,and 39 articles were retrieved for full-text review.Finally,11 articles were selected.The details of literature screening are presented in Fig.1.
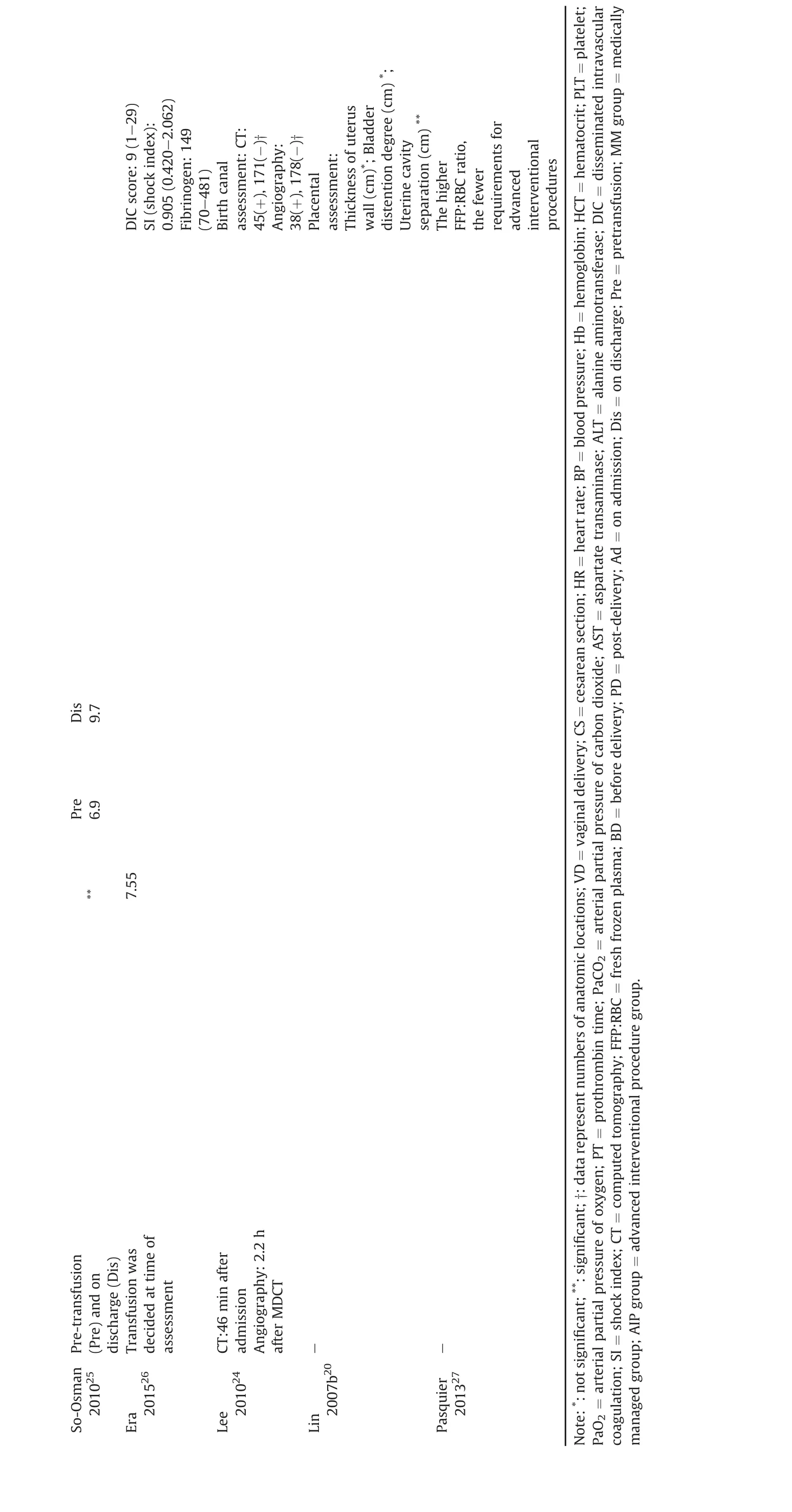
We separated the information extracted into two charts,including the characteristics of studies(Table 1)and the assessment indicators explored in each study(Table 2).Of the 11 studies,4 were conducted in China,2 in France,and the remaining five were from UK,Korea,Japan,Netherlands and Belgium,separately.The sample sizes ranged from 27 to 501,with a total of 1660 samples.The mode of delivery varies among each study,one of which was not specifically depicted given that the subjects were mostly transferred from primary or secondary hospitals.Treatment after delivery was basically administered according to institution rules,and the transferred patients were subjected to advanced interventional operations.Half of the studies(6 out of 11)described the method used to measure assessment indicators.The severity in 7 studies was represented as the amount of blood loss,and the patients in other four studies were previously suffering from PPH or severe PPH,which requires an immediate operation.
Both indicators and the assessment time of each indicator are summarized.The outcome of primary indicators included vital signs,lab tests,placenta completeness,birth canal injury assessment,and other indicators,such as hemodynamic parameters,arterial blood gas and blood biochemistry.In all the 5 studies that included vital signs as indicators,only heart rate and blood pressure were recorded.Hb and HCT were the two lab tests most frequently performed.The associations of these indicators and the severity of blood loss were not consistent across the studies.The study conducted by Lee compared the bleeding locations of birth canal with computed tomography(CT)and angiography,which technically was a diagnostic accuracy experiment.However,no articles about the degree of postpartum uterus contraction were reported,which the authors intended to include as part of the searching strategies.
Table 3 presents the quality judgment results of 11 studies.As previously mentioned,Lee's research was evaluated with the QUADAS-2(Quality Assessment of Diagnostic Accuracy Studies)tool,18whereas the remaining studies were judged with STROBE.Most(9 out of 11)were considered to exhibit high or moderate quality.The remaining two were ranked as low due to the lack of information,such as research design and purpose,detailed information about collecting data,or accurate data for some indicators.
4.Discussion
4.1.Literature screening
Although a total of 2319 studies were initially identi fied,most of them were excluded because the study was not related to PPH or did not focus on maternal assessment.Of those studies involving other diseases,gestational hypertension was a common disease.Other studies on PPH explored the effectiveness of prevention and intervention of PPHrather than assessment indicators.Forinstance,active management of the third stage of labor as a prevention method was discussed in primary studies,systematic reviews and even guidelines.Regarding intervention results,some of the medical treatment studies were not selected because they focused on the dose and incidence of adverse effects.Most of the evidence was obtained from developed countries,whereas no data were reported from Africa,where the prevalence of PPH is the highest.
4.2.Critical appraisal
Most of the articles were rated high or moderate.In these studies,potential bias was not mentioned or discussed as limitation in 5 studies.The data of HR and BP were not accurate in two Chinese studies;“not significantly different”was the only description provided,indicating a low reliability.
4.3.Assessment indicators

?

?
?
Assessing the clinical signs or symptoms of PPH in the parturient is necessary.As the condition worsens,more anomalous indicators are noted.These findings are important as they not only implicate potential PPH but also direct the obstetricians and anesthesiologists how manage the treatment.
Most of the 11 articles included HR,BP,Hb and HCT as primary indicators,whereas other indexes,such as placental assessment,birth canal assessment,and arterial blood gas(ABG)or blood biochemistry items,were less frequently mentioned.HR signi f icantly differed in the studies by Robson,Gayat and Karpati but not in Lin's and Lin's.The latter two studies analyzed visual estimation between groups and precisely measured the method of blood loss.The authors did not group all the subjects into a PPH group and non-PPH group;thus,we could not determine whether the similarity of HR in patients with PPH or those without actually exists.Robson's study compared the HR of the PPH and control groups,reporting a different HR.However,only 9 patients were included in the PPH group,given its incidence.In Gayat's research,all the subjects all had severe PPH and were grouped in the medical treatment group or advanced interventional practice group.The values of both groups reached the borderline,and the AIP group exhibited worse values.The subgroups were formed because the author sought to identify indicators of AIP,which also included abnormal placental implantation,PT<50%,fibrinogen<2 g/L and detectable troponin I.This information helps the obstetricians to make a quicker decision on surgical treatment.The data on admission and discharge of Intensive Care Unit(ICU)were compared in Karpati's study,and the difference was found because patients'conditions were deteriorating when admitted to the ICU.A similar situation was noted for BP,except for the lack of a difference in BP reported in Gayat's study.In the systematic review of Pacagnella,shock index was con firmed as an accurate indicator of compensatory changes related to blood loss.9Shock index is the ratio of HR over Systolic Blood Pressure(SBP).Thus,our findings of HR and BP changes in PPH or severe PPH are to some degree consistent with the present review.It is generally recognized that bleeding less than 500 mL does not cause any clinical symptoms in the mother as the blood volume of full-term pregnant women increase by approximately half.The strong compensation ability allowed the vital signs to be maintained even when the amount of blood loss from hemorrhage reaches 1000 mL.HR and BP are typically two of the vital signs recommended for assessment,28but reports on respiratory rate or temperature changes if the patient starts to suffer severe PPH have not been published.
Hb also differed in Ping's research,wherein two methods of blood loss estimation served as the variables.The incongruity with Lins'results might be explained by the fact that all subjects underwent cesarean section,which typically involves more blood loss.A combined effect of Hb and HCT was not examined given that the assessment time of each article was distinctive.The correlation between Hb or HCT and blood loss can be more complicated in the context of a prescribed blood transfusion.However,the results listed in Table 2 indicate that mild hemorrhage would notresult in a reduction of Hb and HCT,but the values became exacerbated as the hemorrhage worsens.Although Kodkany claimed that mothers who lost less than 500 mL of blood with minor clinical symptoms should be exempted from routine tests,4it would be too late to determine whether the values decrease.Therefore,identifying the best time to run the test can duly signify early interventions.
In Lee's research,the locations of bleeding were rapidly identified with CT compared with traditional angiography or more commonly adopted inspection of the genital tract.This rarely used method of orientation was added to determine extrauterine bleeding with a higher sensitivity than the angiography method.This was the only article that we found regarding birth canal assessment through the search process,implying that either inspection was more prevalent or that genital assessment might be neglected by researchers,clinicians or midwives.
Placental assessment was noted in several studies,mostly using the ultrasound approach for retention.In Lin's research,the 95%con fidence interval of the length of anteroposterior uterine walls(APD)was 5.8-6.4 cm.The larger the length,the more likely PPH will occur.Normal urinary retention is one cause of uterine atony;however,Lin found that the degree of bladder distention was not related to PPH.Detailed results and explanations were not provided in the text;therefore,the reliability of the reported value seemed questionable.The authors concluded that clinicians should regularly use ultrasound as an approach to monitor the APD of the uterine to identify PPH as early as possible.It is recommended that the birth attendants regularly assess the completeness of the placenta.29The necessity of ultrasound in placental assessment needs to be confirmed given that the incidence of placenta accreta or retention is comparatively low,whereas the examination expenses are high.In addition,the effectiveness of ultrasound in identifying the residual tissue was limited;however,this finding is disputed.30Hence,cost-effectiveness analysis should be further performed for routine ultrasound application.
The coagulation function tests were mostly performed in cases of severe PPH,of which platelet and fibrinogen were the most frequently assessed parameters with significant changes.Other indicators that we assessed included ABG,blood biochemistry and hemodynamic parameters,but these parameters exhibited greater alterations in ICU patients and more rarely assessed.The patient's heart pumps more blood swiftly to provide suf ficient blood to vital organs,resulting in an increased velocity integraland stroke volume.Severe PPH could potentially lead to myocardial injury with an elevated TnI,whereasthe liverand kidney function remained normal.

Table 3Quality of included studies.
4.4.Limitations
Given that our literature search focused on English and Chinese studies,studies reported in other languages were not identi fied with the exception of 2 French and 1 Spanish articles,which were excluded through screening.Therefore,data from other countries might not be available.In addition,given the varied subjects of these studies,including both mild PPH and severe PPH patients,and different assessment time points for each indicator,the metaanalysis cannot be further implemented.The generality of the assessment should be deliberated accordingly.
5.Conclusions
According to our findings,assessment indicators and assessment time vary widely among institutions.Existing studies mainly focused on indicators of HR,BP,Hb,HCT,coagulations,blood biochemistry,arterial blood gas,hemodynamic parameters,uterine ultrasound for placental assessment and genital injury assessment,but the postpartum assessments of uterine contraction,level of consciousness,temperature,respiratory rate and bladder filling were not assessed.The association between blood loss and clinical symptoms is not conclusive based on the present studies,and speci fic cut-off points could not be formulated to determine the approximate amount of blood loss.However,some cut-off points can be regarded as a warning for the need for advanced interventions,such as heart rate,prothrombin time,and placental implantation.Further studies on comprehensive assessment and cut-off points should be performed such that birth attendants can distinguish PPH as early as possible.
Conflicts of interest
All authors have none to declare.
1.WHO U,UNFPA,World Bank Group and the United Nations Population Division.Trends in Maternal Mortality:1990 to 2015:Estimates by WHO,UNICEF,UNFPA,WorldBankGroupandtheUnitedNationsPopulationDivision.Switzerland:World Health Organization;2015.
2.WHO.WHO Recommendations for the Prevention and Treatment of Postpartum Haemorrhage.Switzerland:World Health Organization;2012.
3.Lalonde A,International Federation of Gynecology and Obstetrics.Prevention and treatment of postpartum hemorrhage in low-resource settings.Int J Gynaecol Obstet.2012;117:108-118.
4.Kodkany BS,Derman RJ,Sloan NL.Pitfalls in Assessing Blood Loss and Decision to Transfer.A Comprehensive Textbook of Postpartum Hemorrhage.2nd ed.2012:8.
5.American College of Obstetricians and Gynecologists.ACOG practice bulletin:clinical management guidelines for obstetrician-gynecologists number 76,October 2006:postpartum hemorrhage.Obstet Gynecol.2006;108:1039-1047.
6.WHO Guidelines Approved by the Guidelines Review Committee.WHO Recommendations for the Prevention and Treatment of Postpartum Haemorrhage.Geneva:World Health Organization;2012.
7.Clinical Practice Obstetrics Committee.Active management of the third stage of labour:prevention and treatment of postpartum hemorrhage:No.235 October 2009(Replaces No.88,April 2000).Int J Gynaecol Obstet.2010;108:258-267.
8.Behling DJ,Renaud M.Development of an obstetric vital sign alert to improve outcomes in acute care obstetrics.Nurs Womens Health.2015;19:128-141.
9.Pacagnella RC,Souza JP,Durocher J,et al.A systematic review of the relationship between blood loss and clinical signs.PLoS One.2013;8:e57594.
10.Ekelund K,Hanke G,Stensballe J,Wikkelsøe A,Albrechtsen CK,Afshari A.Hemostatic resuscitation in postpartum hemorrhage-a supplement to surgery.Acta Obstet Gynecol Scand.2015;94:680-692.
11.Solomon C,Collis RE,Collins PW.Haemostatic monitoring during postpartum haemorrhage and implications for management.Br J Anaesth.2012;109:851-863.
12.de Lange NM,Lanc′e MD,de Groot R,Beckers EA,Henskens YM,Scheepers HC.Obstetric hemorrhage and coagulation:an update.Thromboelastography,thromboelastometry,and conventional coagulation tests in the diagnosis and prediction of postpartum hemorrhage.Obstet Gynecol Surv.2012;67:426-435.
13.Moher D,Liberati A,Tetzlaff J,Altman DG,PRISMA Group.Preferred reporting items for systematic reviews and meta-analyses:the PRISMA statement.PLoS Med.2009;6:e1000097.
14.Zhan SY.How to report systematic review and meta-analysis:an interpretation of QUAROM and MOOSE.Chin J Evid Based Pediatr.2010;5:60-63(in Chinese).
15.Vandenbroucke JP,von Elm E,Altman DG,et al.Strengthening the Reporting of Observational Studies in Epidemiology(STROBE):explanation and elaboration.Epidemiology.2007;18:805-835.
16.Lin AY,Gao MY,Li XW,et al.Reassessment of postpartum hemorrhage after normal delivery.Chin J Thromb Haemost.2007;13:272-273(in Chinese).
17.Lin JH,Lin QD,Liu JH,Pan ZR,Hu LW,Wang L.Re-estimation of postpartum hemorrhage.Chin J Pract Gynecol Obstetr.2002;6:89-91(in Chinese).
18.Whiting PF,Rutjes AW,Westwood ME,et al.QUADAS-2:a revised tool for the quality assessment of diagnostic accuracy studies.Ann Intern Med.2011;155:529-536.
19.Ping YM,Zheng JM,Wu LX.Comparison of two methods on postpartum hemorrhage assessment of ceserean and its cause analysis.Chin J Hum Sex.2015;24:87-90(in Chinese).
20.Lin Y,Zhou XQ,Yuan H.The clinical values of ultrasound examinations for predicting postpartum hemorrhage.JClinRes.2007;24:1382-1383(in Chinese).
21.Robson SC,Boys RJ,Hunter S,Dunlop W.Maternal hemodynamics after normal delivery and delivery complicated by postpartum hemorrhage.Obstet Gynecol.1989;74:234-239.
22.Gayat E,Resche-Rigon M,Morel O,et al.Predictive factors of advanced interventional procedures in a multicentre severe postpartum haemorrhage study.Intensive Care Med.2011;37:1816-1825.
23.Karpati PC,Rossignol M,Pirot M,et al.High incidence of myocardial ischemia during postpartum hemorrhage.Anesthesiology.2004;100:30-36.
24.Lee NK,Kim S,Kim CW,Lee JW,Jeon UB,Suh DS.Identi fication of bleeding sites in patients with postpartum hemorrhage:MDCT compared with angiography.Air Am J Roentgenol.2010;194:383-390.
25.So-Osman C,Cicilia J,Brand A,Schipperus M,Berning B,Scherjon S.Triggers and appropriateness of red blood cell transfusions in the postpartum patient-a retrospective audit.Vox Sang.2010;98:65-69.
26.Era S,Matsunaga S,Matsumura H,Murayama Y,Takai Y,Seki H.Usefulness of shock indicators for determining the need for blood transfusion after massive obstetric hemorrhage.J Obstet Gynaecol Res.2015;41:39-43.
27.Pasquier P,Gayat E,Rackelboom T,et al.An observational study of the fresh frozen plasma:red blood cell ratio in postpartum hemorrhage.Anesth Analg.2013;116:155-161.
28.QMNCGP.Primary postpartum haemorrhage.In:Program QMaNCG.Brisbane:Queensland Government;2013.
29.Cunningham FG,Gant NF,Leveno KJ,Gilstrap LC,Hauth JC,Wenstrom KD.Williams Obstetrics.24th ed.Beijing:Peking University Medical Press;2014(in Chinese).
30.Malvern J,Campbell S,May P.Ultrasonic scanning of the puerperal uterus following secondary postpartum haemorrhage.J Obstet Gynaecol Br Commonw.1973;80:320-324.
- Frontiers of Nursing的其它文章
- A study on clinical nursing research trends and hotspots based on bibliometric analysis☆
- A study of clinical psychological nursing research hotspots in China and variation trends based on word frequency analysis and visualization analysis☆
- Effectiveness of flipped classrooms in nursing education:Systematic review and meta-analysis
- Current research status and research hotspots in Chinese geriatric medicine:Data retrieved from the Chinese Journal of Geriatrics☆

