肺结核合并呼吸衰竭行小潮气量机械通气的疗效分析
吴恩东+宋丽红+韩芬+张楠+刘秋月+王秀军


[摘要] 目的 探讨小潮气量机械通气与常规潮气量机械通气治疗肺结核合并呼吸衰竭的临床效果。 方法 选取2011年1月~2014年4月首都医科大学附属北京胸科医院收治的肺结核合并呼吸衰竭患者96例,按照随机数字表法分为观察组和对照组,各48例。在常规治疗的基础上,观察组患者给予小潮气量机械通气治疗,对照组患者给予常规潮气量机械通气治疗,比较两组相关血气分析指标、机械通气时间、气压伤发生情况及预后情况。 结果 通气前,两组相关血气分析指标比较,差异无统计学意义(P > 0.05);通气后24 h,两组pH、氧分压(PaO2)明显比通气前高,二氧化碳分压(PaCO2)明显比通气前低,差异有高度统计学意义(P < 0.01);通气后24 h,两组pH比较,差异无统计学意义(P > 0.05);通气后24 h,观察组PaCO2、PaO2明显比对照组高,差异有高度统计学意义(P < 0.01)。观察组机械通气时间短于对照组,差异有高度统计学意义(P < 0.01)。观察组气压伤发生率低于对照组,差异有统计学意义(P < 0.05)。两组预后情况比较,差异有统计学意义(P < 0.05)。 结论 小潮气量机械通气治疗肺结核合并呼吸衰竭可有效提高患者的动脉血PaO2,降低气压伤发生率和死亡率,值得临床应用。
[关键词] 小潮气量;机械通气;肺结核;呼吸衰竭;呼吸机相关性肺损伤
[中图分类号] R521 [文献标识码] A [文章编号] 1673-7210(2015)10(b)-0097-04
Curative effect analysis of low tidal volume mechanical ventilation in pulmonary tuberculosis complicated with respiratory failure
WU Endong1 SONG Lihong2 HAN Fen1 ZHANG Nan1 LIU Qiuyue1 WANG Xiujun1▲
1.Intensive Care Unit, Beijing Chest Hospital Affiliated to Capital Medical University, Beijing 101149, China; 2.Department of Internal Medicine Ward 2, Beijing Chest Hospital Affiliated to Capital Medical University, Beijing 101149, China
[Abstract] Objective To investigate clinical effect of low tidal volume mechanical ventilation and conventional tidal volume mechanical ventilation in the treatment of pulmonary tuberculosis complicated with respiratory failure. Methods 96 cases of patients with pulmonary tuberculosis complicated with respiratory failure in Beijing Chest Hospital Affiliated to Capital Medical University from January 2011 to April 2014 were selected. And the patients were divided into observation group and control group according to the random number table method, each group of 48 cases. On the basis of conventional therapy, observation group was treated with low tidal volume mechanical ventilation, and control group was treated with conventional tidal volume mechanical ventilation. Relative indexes of blood gas analysis, time of mechanical ventilation, barotraumas and prognosis between two groups were compared. Results There were no statistical differences between two groups on relative indexes of blood gas analysis before ventilation (P > 0.05). After ventilation of 24 h, pH and PaO2 of two groups were obviously higher than those before ventilation, PaCO2 of two groups were obviously lower than those before ventilation, the differences were statistically significant (P < 0.01). After ventilation of 24 h, pH between two groups was compared, with no statistical difference (P > 0.05). After ventilation of 24 h, PaCO2 and PaO2 of observation group were obviously higher than those of control group, the differences were statistically significant (P < 0.01). Time of mechanical ventilation in observation group was shorter than that in control group, the difference was statistically significant (P < 0.01). Barotrauma incidence rate of observation group was lower than that of control group, with statistical difference (P < 0.05). Prognosis between two groups was compared, with statistical difference (P < 0.05). Conclusion Low tidal volume mechanical ventilation in the treatment of pulmonary tuberculosis complicated with respiratory failure can effectively improve the patient′s arterial blood PaO2, reduce barotrauma incidence rate and mortality rate, which is worthy of clinical application.endprint
[Key words] Low tidal volume; Mechanical ventilation; Pulmonary tuberculosis; Respiratory failure; Ventilator-induced lung injury
呼吸衰竭是由肺脏本身病变或其他某些原因引起呼吸功能严重损害,造成机体低氧和/或二氧化碳潴留所致的生理和代谢功能紊乱的临床综合征[1-4]。肺结核患者因其免疫力低下、长期能量消耗以及营养供应不足,易引发呼吸肌功能下降,从而最终导致呼吸衰竭,是临床上常见的肺结核并发症[5-7]。随着呼吸机辅助治疗技术的不断发展和完善,机械通气已经成为临床上治疗呼吸衰竭常用的有效手段[8-12]。为了解小潮气量机械通气与常规潮气量机械通气在治疗肺结核合并呼吸衰竭中的临床应用价值,笔者对首都医科大学附属北京胸科医院(以下简称“我院”)收治的96例肺结核合并呼吸衰竭患者进行研究。
1 资料与方法
1.1 一般资料
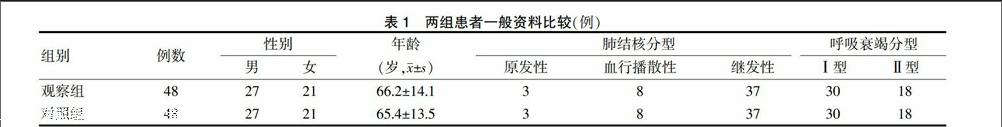
选择我院2011年1月~2014年4月收治的96例肺结核合并呼吸衰竭患者作为研究对象,均符合中华医学会结核病学分会2001年制订的肺结核诊断标准[8]和呼吸衰竭诊断标准[9]。入选患者中,男54例,女42例;年龄20~83岁,平均(65.7±13.8)岁;肺结核分型:原发性肺结核6例,血行播散性肺结核16例,继发性肺结核74例;呼吸衰竭分型:Ⅰ型呼吸衰竭60例,Ⅱ型呼吸衰竭36例。将所有患者按照随机数字表法分为观察组和对照组,两组患者一般资料比较,差异无统计学意义(P > 0.05),具有可比性。见表1。
1.2 方法
1.2.1 肺结核诊断标准 ①咳嗽、咳痰3周及其以上,低热可伴有盗汗、乏力、食欲下降、咯血、胸痛、呼吸困难等症状;②痰液标本镜检结果为阳性;③胸部X线片显示:明显肺部异常阴影,呈现渗出、增殖、纤维或干酪性病变,可伴有胸腔积液、胸膜增厚或粘连等;④胸部CT显示:粟粒阴影,气管或支气管病变[13-14]。
1.2.2 呼吸衰竭诊断标准 ①呼吸困难、口唇发绀、精神萎靡等症状,并发肺性脑病时,还可伴有消化道出血;②血气分析显示:静息状态吸空气时动脉血氧分压(PaO2)< 8.0 kPa(60 mmHg)、二氧化碳分压(PaCO2)> 6.7 kPa(50 mmHg)为Ⅱ型呼吸衰竭,单纯动脉血PaO2降低则为Ⅰ型呼吸衰竭[15-16]。
1.2.3 机械通气方法 入选患者均接受机械通气治疗,均采用PSV通气模式(PS+PEEP),通过调节PS以调整潮气量大小,参考动脉血气分析结果调整吸氧浓度,维持患者血氧饱和度在95%~98%,两组呼吸末正压均为0.5~0.8 kPa(5~8 cmH2O),其中观察组潮气量为5~7 mL/kg,对照组潮气量为9~11 mL/kg。
1.2.4 观察指标 两组均在机械通气前及通气后24 h进行血气分析检测并比较结果,指标包括pH、PaCO2、PaO2;统计两组机械通气时间、气压伤及预后情况。
1.3 统计学方法
采用SPSS 13.0统计软件对数据进行分析和处理,计量资料以均数±标准差(x±s)表示,采用t检验,计数资料采用χ2检验,以P < 0.05为差异有统计学意义。
2 结果
2.1 两组患者通气前后相关血气分析指标比较
通气前,两组相关血气分析指标比较,差异无统计学意义(P > 0.05);通气后24 h,两组pH、PaO2明显比通气前高,PaCO2明显比通气前低,差异有高度统计学意义(P < 0.01);通气后24 h,两组pH比较,差异无统计学意义(P > 0.05);通气后24 h,观察组PaCO2、PaO2明显比对照组高,差异有高度统计学意义(P < 0.01)。见表2。
表2 两组患者通气前后相关血气分析指标比较(x±s)
注:与对照组通气后24 h比较,△t = 5.713,P < 0.01;#t = 10.358,P < 0.01;PaCO2:二氧化碳分压;PaO2:氧分压;1 mmHg = 0.133 kPa
2.2 两组患者机械通气时间比较
观察组机械通气时间为(10.1±5.0)d,对照组机械通气时间为(13.5±5.7)d,观察组显著短于对照组,差异有高度统计学意义(t = 3.107,P < 0.01)。
2.3 两组患者气压伤及预后情况比较
观察组气压伤发生率较对照组低,差异有统计学意义(P < 0.05)。两组预后情况比较,差异有统计学意义(P < 0.05)。见表3。
表3 两组患者气压伤及预后情况比较[n(%)]
3 讨论
肺结核患者由于肺组织长期受结核病毒损伤,其肺组织顺应性变差,并且部分肺间质破坏导致肺泡融合,进而形成肺大泡、空洞等,在接受机械通气治疗时,会由于潮气量不适宜,导致气道压力过高,从而造成气压伤,甚至并发气胸,这种呼吸机相关性肺损伤不仅降低机械通气的治疗效果,而且对患者预后造成不良影响[17-18]。这些机制包括暴露于高通胀的跨肺压力(气压伤)、肺泡过度膨胀(容积伤)或重复开启和关闭肺泡。除了直接的结构破坏外,这些机械力可以触发一系列复杂的炎症介质,使局部和全身性炎性反应传播到非肺器官[19],导致多个系统器官功能障碍,最终死亡。临床发现,在进行机械通气治疗时,除了高气道压外,过度增加肺容积和肺组织过度扩张是导致呼吸机相关性肺损伤发生 的重要机制[20]。
目前认为,传统使用的大潮气量机械通气可导致肺损伤,而小潮气量可能具有肺保护作用。但是,过低的潮气量会导致通气量下降,可能引起二氧化碳潴留、小气道闭合、呼吸道分泌物潴留及肺不张,增加死腔量,造成肺内分流以及高碳酸血症,从而增加肺损伤。采用适当的呼气末正压可使塌陷的肺泡复张,减少呼吸死腔,改善肺的顺应性,以避免上述不良作用[21]。然而,过高的呼气末正压同样会增大气道压力,增加呼吸机相关性肺损伤的风险;同时,使静脉回流阻力、肺血管阻力、右心后负荷增加,心排量、回心血量下降,进而导致血压下降。endprint
本研究中,呼气末正压选择临床上常规使用的0.5~0.8 kPa(5~8 cmH2O),既可以维持一定的肺泡张力,又不会产生严重的呼吸机相关性肺损伤,也不会对循环系统造成严重影响。两组患者均采用相同的呼气末正压,减少其对研究结果的干扰,单纯研究小潮气量和常规潮气量机械通气在治疗肺结核合并呼吸衰竭中的辅助效果,结果表明,小潮气量(6 mL/kg)和常规潮气量(10 mL/kg)机械通气辅助治疗肺结核合并呼吸衰竭患者均可有效调节患者机体pH维持在正常水平,提高患者机体动脉血PaO2,促进机体排出二氧化碳;小潮气量机械通气辅助治疗肺结核合并呼吸衰竭还可以提高临床效果,缩短机械通气时间,有效减少气压伤和降低患者死亡率。
综上所述,小潮气量机械通气辅助治疗肺结核合并呼吸衰竭的临床效果较好,安全性高,值得临床推广应用。
[参考文献]
[1] Christie M,Roscoe J,Chee J,et al. Treatment of a hemodialysis patient with pulmonary calcification-associated progressive respiratory failure with sodium thiosulfate [J]. Transplantation,2013,96(1):e1-e2.
[2] Horne D,Lee JJ,Maas M,et al. Air transported pediatric rescue extracorporeal membrane oxygenation:a single institutional review [J]. World J Pediatr Congenit Heart Surg,2012,3(2):236-240.
[3] 蒋燕红,卢月飞,王建华,等.无创辅助通气联合机械振动排痰及药物治疗COPD急性加重期Ⅱ型呼吸衰竭的临床观察[J].中国药房,2015,26(17):2399-2401.
[4] 陈雄,王文,张静,等.非小细胞肺癌术后并发呼吸衰竭影响因素分析和静息肺功能检测临床价值[J].解放军医药杂志,2015,27(5):33-36.
[5] 崔朝勃,朱华栋,王丽华,等.慢性阻塞性肺疾病合并呼吸衰竭小潮气量机械通气治疗[J].临床肺科杂志,2011, 16(2):98-99.
[6] Komurcuoglu B,Senol G,Balci G,et al. Drug resistance in pulmonary tuberculosis in new and previously treated cases:experience from Turkey [J]. J Infect Public Health,2013,6(4):276-282.
[7] Gowrinath K. Treatment practices in pulmonary tuberculosis by private sector physicians of Meerut,Uttar Pradesh [J]. Indian J Chest Dis Allied Sci,2013,55(1):55.
[8] 中华医学会结核病学分会.肺结核诊断和治疗指南[J].中华结核和呼吸杂志,2001,24(2):70-74.
[9] 陈灏珠,林果为.实用内科学[M].13版.北京:人民卫生出版社,2009.
[10] Pan C,Wang J,Liu W,et al. Low tidal volume protects pulmonary vasomotor function from "second-hit" injury in acute lung injury rats [J]. Respir Res,2012,13:77.
[11] Wright BJ,Slesinger TL. Low tidal volume should not routinely be used for emergency department patients requiring mechanical ventilation [J]. Ann Emerg Med,2012,60(2):216-217.
[12] Mohr NM,Fuller BM. Low tidal volume ventilation should be the routine ventilation strategy of choice for all emergency department patients [J]. Ann Emerg Med,2012,60(2):215-216.
[13] Satoh D,Kurosawa S,Kirino W,et al. Impact of changes of positive end-expiratory pressure on functional residual capacity at low tidal volume ventilation during general anesthesia [J]. J Anesth,2012,26(5):664-669.
[14] Pires KM,Melo AC,Lanzetti M,et al. Low tidal volume mechanical ventilation and oxidative stress in healthy mouse lungs [J]. J Bras Pneumol,2012,38(1):98-104.endprint
[15] Wang W,Scharfstein D,Wang C,et al. Estimating the causal effect of low tidal volume ventilation on survival in patients with acute lung injury [J]. J R Stat Soc Ser C Appl Stat,2011,60(4):475-496.
[16] Fuchs H,Mendler MR,Scharnbeck D,et al. Very low tidal volume ventilation with associated hypercapnia—effects on lung injury in a model for acute respiratory distress syndrome [J]. PLoS One,2011,6(8):e23816.
[17] Yang J,Liu F,Zhu X. The influence of high positive end-expiratory pressure ventilation combined with low tidal volume on prognosis of patients with acute lung injury/acute respiratory distress syndrome:a Meta-analysis [J]. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue,2011,23(1):5-9.
[18] Russ M,Deja M,Ott S,et al. Experimental high-volume hemofiltration with predilutional tris-hydroxymethylamin omethane for correction of low tidal volume ventilation-induced acidosis [J]. Artif Organs,2011,35(6):E108-E118.
[19] Tremblay LN,Slutsky AS. Ventilator-induced injury:from barotraumato biotrauma [J]. Proc Assoc Am Physicians,1998,110(6):482-488.
[20] 冯艳妮,潘红飞,梁玉美.呼吸窘迫综合征呼吸机相关性肺损伤应用肺保护性通气策略的疗效分析[J].中国医药导报,2013,10(18):57-59.
[21] 宋俊杰,李海波.小潮气量保护性机械通气的进展[J].中华危重病急救医学,2013,25(10):633-635.
(收稿日期:2015-05-06 本文编辑:李亚聪)endprint

