Clinical study on nape cluster acupuncture for 50 cases of migraine
Qi Li-zhen (齐丽珍)
Shanghai Institute of Acupuncture and Meridian, Shanghai 200030, China
Special Topic Study
Clinical study on nape cluster acupuncture for 50 cases of migraine
Qi Li-zhen (齐丽珍)
Shanghai Institute of Acupuncture and Meridian, Shanghai 200030, China
Objective:To observe the clinical efficacy of nape cluster acupuncture in treating migraine.
Acupuncture Therapy; Needling Methods; Nape Cluster Acupuncture; Migraine; Pain Measurement; Depression; Points, Head and Neck
Migraine refers to a group of recurrent vascular headache caused by vascular and neurological dysfunction, characterized by episodic and pulsating unilateral headache, sometimes affecting both sides, usually accompanied by nausea, vomiting, and visual disorders. The headache often attacks on seasonal changes, drug discontinuation and infection, and may be coupled with a number of autonomic nervous system symptoms. There are various inducing factors for migraine, among which, tension, anxiety and depression account for 56%-75%[1]. Recurrent headache seriously affects the work and life of patients. Therefore, it’s of great clinical and social significance to safely and effectively treat migraine. I adopted nape cluster acupuncture to treat 50 cases of migraine, and the report is given as follows.
1 Clinical Materials
1.1 Diagnostic criteria
By referring to the diagnostic criteria of migraine from theInternational Classification of Headache Disorders(ICHD-Ⅱ) stipulated by International Headache Society (IHS), including migraine without and with aura[2].
1.2 Inclusion criteria
Conforming to the above diagnostic criteria; aged 18-65 years old; each attack lasting over 4 h; attack frequency at 1-6 times per month; disease duration over 1 year, and the initial attack at a age <50 yearsold; neurologic system tests showed negative, intracranial CT scan or MRI examination showed normal; without cardiovascular diseases or hypertension.
1.3 Exclusion criteria
Headache induced by cerebral ischemia, cerebral infarction, vascular malformation, or arteritis; headache caused by intracranial hypertension; headache caused by cluster headache; headache caused by painful ophthalmoplegia.
1.4 Headache gradingMild: Headache that didn’t affect work and daily life. Moderate: Headache that influenced work and daily life.
Severe: Headache that affected work and daily life, and bed-resting was needed.
1.5 General data
The 50 subjects were from the Outpatient of Shanghai Institute of Acupuncture and Meridian between 2007 and 2013, including 11 males and 39 females; aged from 24 to 55 years old, mean age at 38 years old; disease duration between 12 and 72 months, averaged at 39 months, 29 cases with a duration <36 months, while 21 cases >36 months; 11 cases were migraine with aura, and 39 cases without aura; 6 subjects had a mild headache, 26 cases had a moderate level, and 18 cases belonged to severe level; 33 cases were coupled with depression, and the rest 17 cases didn’t present with depression.
1.6 Statistical method
All data were analyzed by using SPSS 11.0. Measurement data were expressed byand analyzed by pairedt-test before and after treatment; numeration data were by usingRiditanalysis or Chi-square test.
2 Treatment Methods
2.1 Acupoint selection
Nape cluster acupuncture was adopted by longitudinally selecting Xianaohu (Extra, locates at the depression right below the occipital bone), Fengfu (GV 16) and Yamen (GV 15). Then it’s evenly divided into 6 parts between Fengfu (GV 16) and Wangu (GB 12), and each part was taken as an acupoint, 12 points in total covering both sides. Therefore, totally 15 points were selected. See Figure 1 for the details.
2.2 Method
The patient took a sitting or prone position. After routine sterilization, filiform needles of 0.30 mm in diameter and 40 mm in length were used to perpendicularly puncture into the points by about 1 cun, applied by mild lifting-thrusting manipulations till there was tight and sinking feeling beneath the needle and the patient felt distending in the local area. The needles were retained for 30 min, and the treatment was given twice a week. After 2-month treatment, the therapeutic efficacy was evaluated.
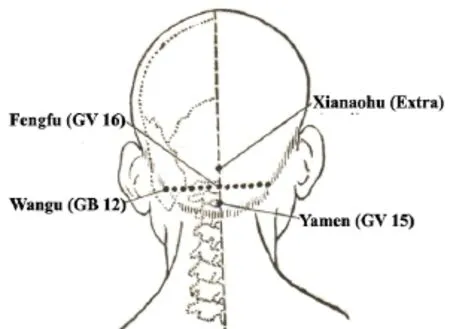
Figure 1. Acupoint location
3 Treatment Result
3.1 Measurement items
All the subjects were evaluated at outset and after 2-month treatment by the short-form of McGill pain questionnaire (SF-MPQ)[3]and self-rating depression scale (SDS)[4].
3.1.1 SF-MPQ
SF-MPQ consisted of three parts: pain rating index (PRI), including 11 sensory words and 4 affective words, graded as no pain, mild pain, moderate pain, and severe pain, respectively scored 0, 1, 2, and 3; visual analogue scale (VAS), evaluated by using a 100 mm line marked from 0 to 100, 0 standing for no pain and 100 for extreme pain, and then the patients were asked to mark on the line, and the distance from 0 to the mark stood for the pain intensity; present pain intensity (PPI) divided pain into 6 levels: no pain, mild, discomforting, distressing, horrible, and excruciating, respectively scored 0, 1, 2, 3, 4, and 5.
3.1.2 SDS
There are 20 questions on SDS that rate the associated symptoms, scored based on the replies: ‘no or a little of the time’ scored 1, ‘some of the time’scored 2, ‘a good part of the time’ scored 3, and ‘most of the time’ scored 4. Of the 20 items, question 2, 5, 6, 11, 12, 14, 16, 17, 18, and 20 were inverse questions, i.e. the higher the score, the less serious the symptom. It would be diagnosed as depression if the score >50.
3.2 Criteria of therapeutic efficacy
The criteria of therapeutic efficacy were made by referring that of migraine in theGuiding Principles for Clinical Study of New Chinese Medicines[5].
Cured: The symptoms were gone; study, life, and work were back to normal.
Markedly effective: Symptoms were obviously reduced; patients could go on studying and working.
Effective: Symptoms were reduced, and the attack frequency decreased.
Invalid: Symptoms showed no change.
3.3 Treatment result
3.3.1 General therapeutic efficacy
After 2-month nape cluster acupuncture, of the 50 subjects, 4 were cured, 19 showed markedly effective, 20 showed effective, 7 failed in the treatment, and the total effective rate was 86.0%.
3.3.2 Comparison of SF-MPQ before and after treatment
After treatment, the positive word number, sensory PRI (S-PRI), affective PRI (A-PRI), total PRI (T-PRI), VAS, and PPI scores were changed significantly (P<0.01), indicating that nape cluster acupuncture can markedly improve the pain in migraine (P<0.01), decrease headache intensity, and reduce the attack frequency (Table 1).
3.3.3 Comparison of SDS before and after treatment
Before treatment, 33 subjects had a SDS score >50 points, indicating that the occurrence rate of depression was 66.0%. The average SDS score was (56.42±8.12) points before treatment versus (41.08±5.73) points after treatment, and the comparison showedt=16.59,P<0.01, showing that the depression degree was obviously improved after nape cluster acupuncture in migraine patients.
3.3.4 Comparison of therapeutic efficacy between different disease durations
The total effective rate was 93.1% in patients with a disease duration <36 months, and was 76.2% in patients with a disease duration >36 months, and theRiditanalysis showedu=2.631,P<0.05, suggesting that the therapeutic efficacy was higher in patients with a shorter disease duration (Table 2).
3.3.5 Comparison of therapeutic efficacy between different headache intensities
The total effective rate was 93.8% in the mild-moderate headache patients, while was 72.2% in the severe headache patients, and theRiditanalysis showedu=3.638,P<0.01. It indicates that acupuncture produced a more significant effect on mild-moderate headache patients than on severe headache patients (Table 3).
3.3.6 Therapeutic efficacy and depression.
The total effective rate was 81.8% in the migraine patients with depression, while was 94.1% in the patients without depression, andRiditanalysis showedu=-1.526,P>0.05, indicating that nape cluster acupuncture tended to produce a more significant effect on migraine patients without depression than those with depression (Table 4).
Table 1. Comparison of SF-MPQ (n=50,point )

Table 1. Comparison of SF-MPQ (n=50,point )

Table 2. Comparison of therapeutic efficacy between different disease-duration groups (case)
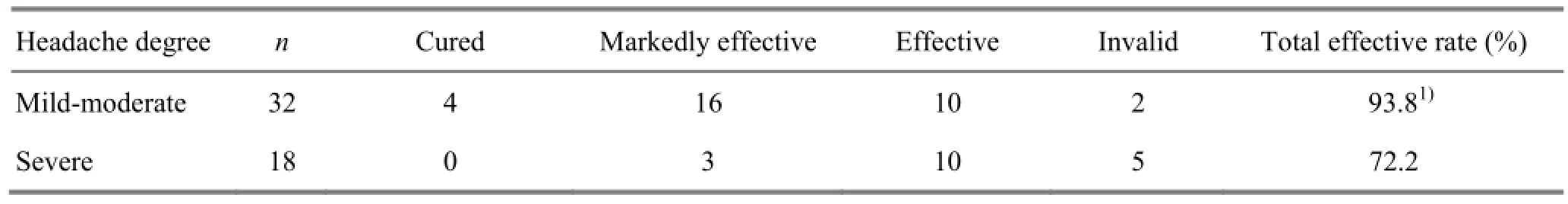
Table 3. Comparison of therapeutic efficacy between different headache-degree groups (case)

Table 4. Comparison of therapeutic efficacy between depression and non-depression groups (case)
4 Discussion
As a common neurological disease, migraine is a chronic neuro-vascular disorder and its pathogenesis is not clear, though the genetic factor, endocrine, vascular factor, neurotransmitters, and immune factor are possibly involved. In traditional Chinese medicine (TCM), head is considered as the joint of yang and the house of clear yang qi. The essence of five Zang organs and clear yang qi of six Fu organs all go to head. When the six pathogenic factors attack the vertex and block the clear yang qi, or internal disorders induce qi-blood stagnation or the turbid phlegm blocking collaterals, malnutrition of brain, spasm of cerebral vessels, the migraine will occur.
Nape cluster acupuncture adopted in this study was invented by the late acupuncture master Hua Yan-ling[6], working to treat lots of brain-related diseases, benefiting and tonifying brain, regulating the Governor Vessel and anchoring mind. Nape cluster acupuncture is usually performed along the Governor Vessel, Bladder Meridian of Foot Taiyang, and Gallbladder Meridian of Foot Shaoyang. The Governor Vessel runs through spine and belongs to the kidney, its branch is connected to the kidney and runs through the heart, and its qi reaches to brain. Therefore, the Governor Vessel can be used to treat brain-related diseases, functioning to nourish brain and soothe mind. The Governor Vessel is also the junction of yang meridians, working to govern yang qi, and when punctured, it can tonify yang qi, reinforce essence and marrow, and nourish brain and mind. Migraine is closely related to the Gallbladder Meridian of Foot Shaoyang, as migraine affects head, where majorly runs the Gallbladder Meridian. Thus, nape cluster acupuncture can achieve a satisfactory result in treating migraine, because it’s closely associated with the Governor Vessel, Foot Taiyang Meridian, and Foot Shaoyang Meridian.
Western medicine holds that migraine is related to the cranial vasomotor instability brought by various factors, and also the dysfunction of central nerves which are in charge of regulating vasomotion. Acupuncture can adjust the cerebral vasomotion in a positive manner, improve cerebral blood flow, and correct the asymmetry of blood flow. By analyzing the data provided by transcranial Doppler (TCD), some scholars found that acupuncture at scalp acupoints can affect the patients with vasobasilar insufficiency (VBI) of a low blood flow velocity, manifested by the increase of diastolic blood flow velocity, systolic blood flow velocity, and average blood flow velocity immediately after acupuncture, and at 20 min and 24 h[7]. Another report said that acupuncture at Fengchi (GB 20) (this point is selected in nape cluster acupuncture) can regulate the blood flow velocity in a bidirectional way by modulating adrenaline and cholingergic nerve fibers in VBI[8]. Tang SX, et al[9]adopted acupuncture at scalp acupoints to treat migraine, meanwhile detecting the levels of endothelin (ET) and nitric oxide (NO). The results were compared to those of healthy subjects. The half-a-year follow-up study showed that the ET and NO levels were back to normal after acupuncture. Besides, acupuncture also affects the limbic system which is related to emotional reaction and some key nuclei in basal ganglion, and thus can reduce pain reactions, increase pain threshold and pain tolerance[10]. Nape cluster acupuncture can regulate topical vasomotion and nerve function, working to unblock meridians, harmonize qi and blood, release spasm, and cease the pain. This clinical study showed that the total effective rate was 86.0% in the treatment of migraine with nape cluster acupuncture. Besides, the patients with a shorter disease duration achieved a better efficacy than the one with a longer disease duration (P<0.05); patients with mild-moderate headache achieved a better efficacy than the one with a severe headache (P<0.01); patients without depression achieved a higher total effective rate than the one with depression.
SF-MPQ is a multi-factor pain assessment method, combining cognition, affection, and sensation factors, focused on observing pain and its nature, characteristic, intensity, and accompanied conditions, as well as various factors that patients experience after treatment, and thus SF-MPQ can offer a comparatively correct evaluation of pain intensity and nature. Associated with grading, PRI not only can reflect pain nature, but also can measure pain intensity. The measurement of VAS is correct to 1 mm, with high sensitivity. Patients are asked to mark on the scale by themselves, which avoids the influence from external environment. It’s effective and practical to use PRI, VAS, and PPI together, as they are all quantitative indexes, which is convenient for computer to manage the data, and also provides convenience to clinical study on pain[3]. In the 50 subjects from the current study, the positive items, S-PRI, A-PRI, T-PRI, VAS, and PPI scores were significantly changed after intervention (P<0.01), indicating that nape cluster acupuncture can effectively improve the headache in migraine patients.
With a comparatively high reliability and validity, SDS is easy-to-operate, and it can comprehensively, precisely, and quickly reflect the intensity and variation of the symptoms related to depression. Of the 50 subjects recruited in this study, SDS >50 points in 33 patients before the intervention, and the occurrence rate of depression was 66.0%; the SDS scores decreased significantly after the treatment (P<0.01), indicating that the depression state was markedly improved after nape cluster acupuncture in migraine patients.
The results of the study suggest that nape cluster acupuncture can obviously reduce pain degree and improve the depression state in migraine patients, and thus this method is worth promotion in clinic.
Conflict of Interest
The author declared that there was no conflict of interest in this article.
Acknowledgments
This work was supported by Shanghai Leading Academic Discipline Project (上海市重点学科建设项目,No. S30304).
Statement of Informed Consent
Informed consent was obtained from all individual participants included in this study.
Received: 5 March 2015/Accepted: 16 April 2015
[1] Xu C. Analysis of risk factors for migraine. Shijie Zuixin Yixue Xinxi Wenzhai, 2015, (5): 45, 49.
[2] Headache Classification Committee of the International Headache Society. Classification and diagnostic criteria for headache disorders, cranial neuralgia, and facial pain. Cephalagia, 1998, 8(Supp17): 1-96.
[3] Luo YJ. Evaluation of the clinical application of short-form McGill pain questionnaire. Zhongguo Kangfu, 1992, 7(4): 160-164.
[4] Zhang MY. Handbook of Psychiatric Questionnaires. Changsha: Hunan Science and Technology Press, 1998: 35-42.
[5] Ministry of Health of the People’s Republic of China. Guiding Principles for Clinical Study of New Chinese Medicines. Beijing: China Medical Science Press, 2002: 109.
[6] Qi LZ. Academic experience collection of Hua Yan-ling. Shanghai Zhenjiu Zazhi, 1995, 14(3): 97-98.
[7] Wang LP, Zhou W, Zhang YQ, Guo LZ. Clinical study on the effect of acupuncture at Houding (GV 19) on vertebrobasilar artery. Zhongguo Zhen Jiu, 1998, 18(4): 205-207.
[8] Yuan XJ, Hao XS, Lai ZP, Zhao H, Liu WY. Effect of acupuncture at Fengchi (GB 20) on cerebral blood flow. Zhongyi Zazhi, 1996, 37(5): 285-288.
[9] Tang SX, Xu ZH, Tang P, Luo MF. Clinical study on acupuncture regulating vasoconstrictive factor and vasodilatory factor in the patient of migraine. Zhongguo Zhen Jiu, 2004, 24(2): 103-104.
[10]Shi XM. Science of Acupuncture and Moxibustion. Shanghai: Shanghai Scientific & Technical Publishers, 1998: 286.
Translator: Hong Jue (洪珏)
项丛刺治疗偏头痛50例临床观察
目的:观察项丛刺治疗偏头痛的临床疗效。方法:对50例诊断明确的偏头痛患者采用项丛刺治疗, 并于入选时和治疗2个月后分别采用简化McGill疼痛问卷(short-form of McGill pain questionnaire, SF-MPQ)和抑郁自评量表(self-rating depression scale, SDS)进行临床评定。结果:患者治疗前后选词阳性项目数、疼痛分级指数(pain rating index, PRI)感觉分、PRI情绪分、PRI总分、视觉模拟量表评分(visual analogue scale, VAS)、现时疼痛强度(present pain intensity, PPI)差异均有统计学意义(均P<0.01); 治疗前SDS评分为(56.42±8.12)分, 治疗后为(41.08±5.73)分,治疗前后SDS评分差异有统计学意义(P<0.01)。治疗结束后总有效率为86.0%;病程短的患者疗效优于病程长者(P<0.05); 轻中度头痛患者疗效优于重度头痛患者(P<0.01); 不伴抑郁的患者总有效率优于伴抑郁的患者, 但疗效差异无统计学意义(P>0.05)。结论:项丛刺治疗偏头痛疗效确切, 对患者头痛和抑郁程度有明显的改善作用。
针刺疗法; 刺法; 项丛刺; 偏头痛; 疼痛测定; 抑郁; 穴位, 头颈部
R246.6 【
】A
Author: Qi Li-zhen, bachelor, chief physician.
E-mail: qlz60@163.com
Methods:Fifty patients with confirmed diagnosis of migraine were intervened by using nape cluster acupuncture, and were evaluated at the outset and after 2-month treatment by the short-form of McGill pain questionnaire (SP-MPQ) and self-rating depression scale (SDS).
Results:After treatment, the number of positive words, sensory pain rating index (S-PRI), affective pain rating index (A-PRI), total pain rating index (T-PRI), visual analogue scale (VAS), and present pain intensity (PPI) were significantly changed (P<0.01); the SDS score was (56.42±8.12) points before treatment versus (41.08±5.73) points after treatment, and the difference was statistically significant (P<0.01). The total effective rate was 86.0%; the therapeutic efficacy of the patients with a shorter disease duration was superior to that of the patients with a longer one (P<0.05); the efficacy of mild-moderate migraine was superior to that of severe one (P<0.01); the total effective rate of patients without depression was higher than that with depression, but without a significant difference in comparing the therapeutic efficacy (P>0.05).
Conclusion:Nape cluster acupuncture is effective in treating migraine, significantly improving headache and depression.
 Journal of Acupuncture and Tuina Science2015年5期
Journal of Acupuncture and Tuina Science2015年5期
- Journal of Acupuncture and Tuina Science的其它文章
- Survey on acupuncture treatment of neurogenic dysphagia and analysis of regularity of acupoint selection
- Combining acupuncture and copper-tube moxibustion for 39 cases of recurrent peripheral facial paralysis
- Study on metabolic intensity value changes of points on the face using thermal chromatography technology
- Tuina along the meridians combined with Chinese medicine for motor functions and activities of daily living in patients with post-stroke upper limb spasticity
- Clinical observation on acupuncture combined with Chinese medicine and rehabilitation training for subacute stroke patients
- Clinical effect observation on acupuncture for chronic obstructive pulmonary disease
