小儿肺热咳喘口服液对小儿毛细支气管炎Th1/Th2细胞的影响研究
李静,董艳,张晶洁,潘鸿
·中医·中西医结合·
小儿肺热咳喘口服液对小儿毛细支气管炎Th1/Th2细胞的影响研究
李静,董艳,张晶洁,潘鸿
目的探讨小儿肺热咳喘口服液对小儿毛细支气管炎Th1/Th2细胞的影响。方法选择2013年9月—2014年12月北京市昌平区中西医结合医院儿科收治的毛细支气管炎住院患儿80例,按随机数字表法分为试验组和对照组,各40例。根据临床用药指南,两组患儿均给予抗感染和对症治疗,对照组患儿静脉滴注头孢曲松钠治疗,治疗组患儿在对照组基础上给予小儿肺热咳喘口服液治疗,疗程均为7 d。比较两组患儿临床疗效,治疗前后干扰素γ (IFN-γ)、白介素4(IL-4)水平及Th1细胞分数、Th2细胞分数、Th1/Th2细胞百分比变化,并观察治疗期间两组患儿不良反应发生情况。结果试验组患儿临床疗效优于对照组(P<0.05)。治疗前两组患儿血清IFN-γ、IL-4水平及Th1细胞分数、Th2细胞分数、Th1/Th2细胞百分比比较,差异无统计学意义(P>0.05);治疗后试验组患儿血清IFN-γ、IL-4水平及Th1细胞分数、Th2细胞分数、Th1/Th2细胞百分比低于对照组(P<0.05)。结论小儿肺热咳喘口服液治疗毛细支气管炎患儿临床疗效良好,可通过调节Th1/Th2细胞而增加患儿免疫功能。
毛细支气管炎;小儿肺热咳喘口服液;Th1-Th2平衡
李静,董艳,张晶洁,等.小儿肺热咳喘口服液对小儿毛细支气管炎Th1/Th2细胞的影响研究[J].实用心脑肺血管病杂志,2015,23(4):114-117.[www.syxnf.net]
Li J,Dong Y,Zhang JJ,et al.Impact of xiaoer-feire-kechuan oral solution on Th1/Th2 cells of infants with bronchiolitis[J].Practical Journal of Cardiac Cerebral Pneumal and Vascular Disease,2015,23(4):114-117.
毛细支气管炎是儿科常见疾病,多发于1岁尤其是6个月以下婴幼儿,春季为其高发季节[1]。毛细支气管炎是由呼吸道合胞病毒引起下呼吸道急性炎症所致的气道阻塞性疾病[2],近年来,该病在婴幼儿肺部病毒感染疾病中居首位[3]。其主要临床表现为呼吸困难、喘息且易反复发作,与一般炎症不同,患儿常为家族遗传性过敏体质[4]。临床研究显示,毛细
支气管炎的发病机制与哮喘极相似,且该病病后哮喘发生率高达25%~50%[5]。临床上治疗毛细支气管炎以抗感染及对症治疗为主,但患儿极易出现胃部不适等不良反应[6]。毛细支气管炎隶属中医“咳嗽”范畴,且临床多见痰热壅肺型[7]。小儿肺热咳喘口服液为中药合剂,由多种中草药提炼而成,其中包含了麻杏石甘汤及白虎汤两剂古方,加之现代经典方剂,具有解毒清热化痰、宣肺止咳平喘的功效[8-9]。有研究证实,小儿肺热咳喘口服液具有广谱抗菌、抗病毒的作用[10]。本研究探讨了小儿肺热咳喘口服液对小儿毛细支气管炎Th1/Th2细胞的影响,旨在为临床应用小儿肺热咳喘口服液治疗小儿毛细支气管炎提供参考。
1 资料与方法
1.1 纳入和排除标准纳入标准:(1)符合全国小儿呼吸疾病会议制定的相关诊断标准,以憋闷、喘息为主要临床表现,或伴有发热,双肺可闻及喘鸣音或湿啰音;(2)年龄<2岁; (3)首次发病,且无其他急、慢性疾病;(4)病程2~7 d; (5)经患儿家长同意并签署知情同意书。排除标准:(1)近2周有其他呼吸道炎症或感染者;(2)合并其他急、慢性疾病者;(3)过敏体质及有免疫系统疾病者;(4)有先天性疾病和其他遗传疾病者;(5)患儿家长拒绝接受治疗者。
1.2 一般资料选择2013年9月—2014年12月北京市昌平区中西医结合医院儿科收治的毛细支气管炎住院患儿80例,按随机数字表法分为试验组和对照组,各40例。两组患儿性别、月龄、白细胞计数(WBC)及病程比较,差异无统计学意义(P>0.05,见表1),具有可比性。
表1 两组患儿一般资料比较(±s)Table 1 Comparison of general information between the two groups

表1 两组患儿一般资料比较(±s)Table 1 Comparison of general information between the two groups
注:WBC=白细胞计数,*为χ2值
组别例数性别(男/女)月龄(月) WBC (×109/L)病程(d) 40 22/18 15.4±2.7 12.64±2.14 4.6±1.6试验组40 20/20 17.6±2.3 13.52±1.89 3.8±1.0 t(χ2)值对照组0.680 0.890 0.608 1.610 0.610 0.682 0.092 P值12.06*
1.3 治疗方法根据临床用药指南,两组患儿均给予抗感染和对症治疗,对照组患儿静脉滴注头孢曲松钠50~80 mg/kg,1次/d。治疗组患儿在对照组基础上给予小儿肺热咳喘口服液,具体用法:1岁以下患儿5 ml/次,2次/d;1~3岁患儿10 ml/次,3次/d。疗程均为7 d,且治疗期间注意患儿饮食及观察患儿临床症状、体征变化。
1.4 观察指标治疗后判定两组患儿临床疗效,比较两组患儿治疗前后干扰素γ(IFN-γ)、白介素4(IL-4)水平及Th1细胞分数、Th2细胞分数、Th1/Th2细胞百分比变化,并观察治疗期间两组患儿不良反应发生情况。
1.4.1 血清IFN-γ、IL-4水平检测清晨空腹采集静脉血3 ml,1 200 r/min离心,离心半径为3 cm,分离血清,待检。采用双抗体夹心酶联免疫吸附试验(ELISA)法测定血清IFN -γ和IL-4水平,操作步骤严格按照试剂盒说明书进行操作。
1.4.2 Th1/和Th2细胞检测取患者外周静脉血3 m l,采用FACSCalibur流式细胞仪检测Th1细胞分数、Th2细胞分数,计算Th1/Th2细胞百分比。
1.5 临床疗效判定标准显效:咳嗽、喘息及肺部啰音等临床症状显著改善;有效:咳嗽、喘息及肺部啰音等临床症状好转,体温恢复正常;无效:咳嗽、喘息及肺部啰音等临床症状未见好转或出现加重,其他临床症状未见改善。
1.6 统计学方法采用SPSS 19.0统计学软件进行数据处理,计量资料以(±s)表示,采用两独立样本t检验;计数资料采用χ2检验;等级资料采用秩和检验。以P<0.05为差异有统计学意义。
2 结果
2.1 两组患儿临床疗效比较试验组患儿临床疗效优于对照组,差异有统计学意义(u=1.816,P<0.05,见表2)。

表2 两组患儿临床疗效比较〔n(%)〕Table 2 Comparison of clinical effect between the two groups
2.2 两组患儿血清IFN-γ和IL-4水平比较治疗前两组患儿血清IFN-γ、IL-4水平比较,差异无统计学意义(P>0.05);治疗后试验组患儿血清IFN-γ、IL-4水平低于对照组,差异有统计学意义(P<0.05,见表3)。
表3 两组患儿治疗前后血清IFN-γ、IL-4水平比较(±s,μg/L)Table 3 Comparison of serum levels of IFN-γ,IL-4 between the two groups before and after treatment

表3 两组患儿治疗前后血清IFN-γ、IL-4水平比较(±s,μg/L)Table 3 Comparison of serum levels of IFN-γ,IL-4 between the two groups before and after treatment
注:IFN-γ=干扰素γ,IL-4=白介素4
组别例数IFN-γ治疗前治疗后对照组治疗后IL-4治疗前40 4.53±1.44 4.19±1.22 3.19±1.19 1.95±0.71试验组40 4.72±1.18 4.16±1.04 3.28±1.07 1.18±0.37 t 1.021 2.971 0.681 3.551 P值值0.605 0.005 0.523 0.001
2.3 两组患儿Th1、Th2细胞分数及Th1/Th2细胞百分比比较
治疗前两组患儿Th1、Th2细胞分数及Th1/Th2细胞百分比比较,差异无统计学意义(P>0.05);治疗后试验组患儿Th1、Th2细胞分数及Th1/Th2细胞百分比低于对照组,差异有统计学意义(P<0.05,见表4、图1~2)。
表4 两组患儿治疗前后Th1细胞分数、Th2细胞分数及Th1/Th2细胞百分比比较(±s,%)Table 4 Comparison of Th1,Th2 cell counts and Th1/Th2 cell percentage between the two groups before and after treatment
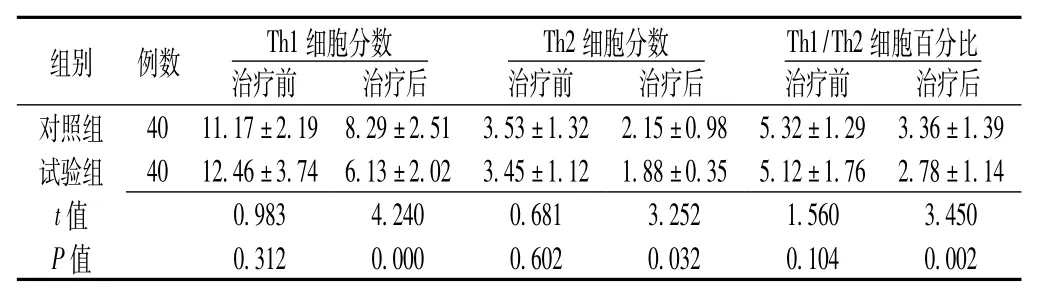
表4 两组患儿治疗前后Th1细胞分数、Th2细胞分数及Th1/Th2细胞百分比比较(±s,%)Table 4 Comparison of Th1,Th2 cell counts and Th1/Th2 cell percentage between the two groups before and after treatment
组别例数Th1细胞分数治疗前治疗后对照组40 11.17±2.19 8.29±2.51 3.53±1.32 2.15±0.98治疗后Th2细胞分数治疗前治疗后Th1/Th2细胞百分比治疗前5.32±1.29 3.36±1.39试验组40 12.46±3.74 6.13±2.02 3.45±1.12 1.88±0.35 5.12±1.76 2.78±1.14 t 0.983 4.240 0.681 3.252 1.560 3.450 P值值0.312 0.000 0.602 0.032 0.104 0.002

图1 两组患儿Th1流式细胞图Figure 1 Flow cytometry of Th1 between the two groups

图2 两组患儿Th2流式细胞图Figure 2 Flow cytometry of Th2 between the two groups
3 讨论
毛细支气管炎又称“喘息性肺炎”,是婴幼儿特有的呼吸道感染性疾病,其主要临床表现为呼吸急促、发热咳嗽、喘息憋闷及吸气性胸部凹陷等[11]。目前,毛细支气管炎的发病机制尚未明确,多数学者认为其是由病毒直接作用所致,如流感病毒、鼻病毒、副流感病毒、人类偏肺病毒等,且50%以上是由吸道合胞病毒引起;还有学者认同神经致病机制及免疫病理机制等[12-13]。由于小儿为纯阳之体而易感邪化热,因此,治疗应以清肃肺热、解毒平喘为主[14]。小儿肺热咳喘口服液方中所含麻杏石甘汤主宣肺止咳,白虎汤清热生津,配以金银花、鱼腥草清理肺热,知母、麦冬滋阴解郁除烦,组方合理精辟[15]。本研究结果显示,小儿肺热咳喘口服液可以降低毛细支气管炎患儿Th1和Th2细胞水平,从而提高患儿免疫功能。
Smith等[16]研究显示,毛细支气管炎患儿因Th2源性细胞因子作用而易转变为哮喘,临床已证实支气管哮喘发病机制是Th1/Th2细胞和功能失衡所致,且免疫学研究也显示,毛细支气管炎与哮喘的发病机制相似,均存在Th1/Th2细胞失调[17-18]。Th1细胞主要分泌IFN-γ,其能促使机体产生白介素12(IL-12),并形成正反馈调节。毛细支气管炎急性期因抑制Th1细胞功能而不能诱导产生IFN-γ,而经药物治疗后IFN-γ水平升高,提示IFN-γ早期就参与毛细支气管炎的炎症免疫过程[19]。毛细支气管炎是由多种炎性细胞、炎性递质和细胞因子参与形成的慢性气道炎症,具有气道高反应性、可逆性气道阻塞和气道变应性炎症等临床特征,其发病过程与Th活化并分泌多种细胞因子密切相关[17-18]。近年有研究显示,Th1与Th2的失衡与哮喘发生关系密切[19]。正常情况下Th1产生IL-2、IFN-γ及肿瘤坏死因子α、β等多种细胞炎性因子,激活巨噬细胞而发生迟发超敏反应;Th2细胞产生IL -4、IL-5、IL-6、IL-10、IL-13等多种细胞炎性因子,诱导嗜酸粒细胞产生和募集及免疫球蛋白亚型转化,从而产生IgE。这两类细胞炎性因子表达的正常调节由Th1/Th2细胞功能的平衡决定。在上述诸多细胞炎性因子中,IL-4与IFN-γ互为拮抗作用,常用来反映Th1/Th2细胞的平衡[20]。Th2细胞主要分泌IL-4,其作用是诱导Th2细胞的生长和分化,并能抑制Th1细胞产生IFN-γ,其在变应性炎症的发生发展中具有重要作用[20]。本研究结果显示,治疗后试验组患儿血清IFN-γ和IL-4水平低于对照组,且Th1细胞分数、Th2细胞分数及Th1/Th2细胞百分比低于对照组,提示小儿肺热咳喘口服液可以降低毛细支气管炎患儿Th1/Th2细胞水平。
综上所述,小儿肺热咳喘口服液治疗小儿毛细支气管炎临床疗效良好,可通过调节Th1/Th2细胞而增加患儿免疫功能,值得临床推广应用。
[1]Openshaw PJ,Tregoning JS.Immune responses and disease enhancement during respiratory syncytial virus infection[J].Clin Microbiol Rev,2005,18(3):541-555.
[2]Legg JP,Hussain IR,Warner JA,et al.Type 1 and type 2 cytokine im-balance in acute respiratory syncytialvirusbronchiolitis[J].Am J Respir Crit Care Med,2003,168(6):633-639.
[3]Takemura M,Niimi A,Matsumoto H,et al.Clinical,physiological and anti-inflammatory effect of montelukast in patients with?cough variant asthma[J].Respiration,2012,83(4):308-315.
[4]Tripp RA,Oshansky C,Alvarez R.Cytokines and Respiratory Syncytial Virus Infection[J].Proc Am Thorac Soc,2005,2 (2):147-149.
[5]Pinto RA,Arredondo SM,Bono MR,et al.Thelper1/Thelper2 cyto -kine imbalance in respiratory syncytial virus infection is associated with increased endogenous plasma cortisol[J].Pediatrics,2006,117(5):e878-e886.
[6]Tamaoki J,Yokohori N,Tagaya E,et al.Comparable effect of a leukotriene receptor antagonist and long-acting beta-adrenergic agonist incough variant asthma[J].Allergy Asthma Proc,2010,31 (5):78-84.
[7]Legg JP,Hussain IR,Warner JA,et al.Type 1 and type 2 cytokine imbalance in acute respiratory syncytial virus bronchiolitis[J].Am J Respir Crit Care Med,2003,168(6):633-639.
[8]CostaML,Stein RT,Bauer ME.Levels of Th1 and Th2 cytokines in children with post-infectious bronchiolitis obliterans[J].Ann Trop Paediatr,2005,25(4):261-266.
[9]Matsuoka H,Niimi A,Matsumoto H,et al.Inflammatory subtypes
in coughvariant asthma:association with maintenance doses of inhaled corticosteroids[J].Chest,2010,138(6):1418-1425.
[10]Brandenburg AH,Kleinjan A,van Het Land B,et al.Type1-like immune response is found in children with respiratory syncy-tial virus infection regardless of clinical severity[J].J Med Virol,2000,62(2):267-277.
[11]Flamant C,Hallalel F,Nolent P,et al.Severe respiratory syncytialvirus bronchiolitis in children:From short mechanical ventilation to extracor-porealmembrane oxygenation[J].EurJPediatr,2005,164(2):93-98.
[12]Bartz H,Turkel O,Hoffjan S,et al.Respiratory syncytial virus decreases the capacity of myeloid dendritic cells to induce inter-feron -gamma in naive T cells[J].Immunology,2003,109(1):49 -57.
[13]Piedimonte G,Renzetti G,Auais A,et al.Leukotriene synthesis during respiratory syncytial virus bronchiolitis:influence of age and atopy[J].Pediatr Pulmonol,2005,40(4):285-291.
[14]Bendelja K,Gagro A,Bace A,et al.Predominant type 2 response in infants with respiratory syncytial virus(RSV)infection demonstrated by cytokine flow cytometry[J].Clin Exp Immunol,2000,121(2):332-338.
[15]Bacharier LB,Boner A,Carlsen KH,et al.Diagnosis and treatment of asthma in childhood:a PRACTALL consensus report[J].Allergy,2008,63(1):5-34.
[16]Smith PK,Wang SZ,Dowling KD,et al.Leucocyte populationsin respiratory syncytial virus-induced bronchiolitis[J].J Paediatr Child Health,2001,37(2):146-151.
[17]Papadopoulos NG,Arakawa H,Carlsen KH,et al.International consensus on(ICON)pediatric asthma[J].Allergy,2012,67 (8):976-997.
[18]Yu I,Yoo Y,Kim DK,et al.Distribution of antibody time to Mycoplasma pneumoniae in Korean children in 2000—2003[J].J Korean Med Sci,2005,20(4):542-547.
[19]Oommen A,Grigg J.Urinary leukotriene E4 in preschool children with acute clinical viral wheeze[J].Eur Respir J,2003,21(1): 149-154.
[20]Bukstein DA,Luskin AT,Bernstein A."Real world"effective daily controller medicine in children with mild persistent asthma[J].Ann Allergy Asthma Immunol,2003,90(5):543-549.
Im pact of Xiaoer-feire-kechuan O ral Solution on Th1/Th2 Cells of Infants w ith Bronchiolitis
LI Jing,DONG Yan,ZHANG Jing-jie,et al.
Integrated Chinese and Western Medicine Hospital of Changping District,Beijing 102208,China
Objective To explore the impact of xiaoer-feire-kechuan oral solution on Th1/Th2 cells of infants with bronchiolitis.M ethods A total of 80 infants with bronchiolitis that hospitalized in Department of Pediatrics,Integrated Chinese and Western Medicine Hospital of Changping District were selected from September 2013 to December 2014,and they were divided into experiment group and control group according to random number table,each of 40 cases.Infants of both groups were given anti-infectious therapy and symptomatic treatment according to clinical medication guides,and infants of control group were given extra intravenous drip of ceftriaxone sodium,while infants of experiment group were given extra xiaoer-feirekechuan oral solution based on the treatment of control group,both groups treated for 7 days.Clinical effect,serum levels of IFN -γ and IL-4,Th1 cell counts,Th2 cell counts and Th1/Th2 cell percentage before and after treatment were compared between the two groups,and incidence of adverse reactions were observed.Results The clinical effect of experiment group was statistically significantly better than that of control group(P<0.05).No statistically significant differences of serum levels of IFN-γ and IL-4,Th1 cell counts,Th2 cell counts or Th1/Th2 cell percentage were found between the two groups before treatment(P>0.05);while serum levels of IFN-γ and IL-4,Th1 cell counts,Th2 cell counts and Th1/Th2 cell percentage of experiment group were lower than those of control group after treatment(P<0.05).Conclusion Xiaoer-feire-kechuan oral solution can has a certainly good clinical effect on bronchiolitis in infants,it may adjust Th1/Th2 cells to improve the immune function.
Bronchiolitis;Feirekechuan oral liquid;Th1-Th2 balance
R 562.21
B
10.3969/j.issn.1008-5971.2015.04.038
2015-02-13;
2015-04-15)
(本文编辑:谢武英)
102208北京市昌平区中西医结合医院

