阵发性心房颤动患者左右心房电传导特点的临床研究
林明宽,刘 浩,周 婷
·全科医生知识窗·
阵发性心房颤动患者左右心房电传导特点的临床研究
林明宽,刘 浩,周 婷
目的 探讨阵发性心房颤动患者左右心房电传导的特点。方法 选取2012年4月—2013年5月广西医科大学第一附属医院住院行射频消融术的阵发性心房颤动患者19例为心房颤动组,另选取同时期住院的阵发性室上性心动过速或室性期前收缩患者23例为对照组,应用固定程序SIS,500、400、350、300、280 ms分别起搏高位右心房、低位右心房,分别测量冠状窦近端、远端不应期,高位、低位右心房到冠状窦近端、远端传导时间。结果 对照组与心房颤动组冠状窦近端、远端不应期比较,差异均无统计学意义(P>0.05)。对照组与心房颤动组不同起搏时间高位右心房到冠状窦近端传导时间比较,差异均无统计学意义(P>0.05);对照组与心房颤动组起搏时间500、400、350 ms时高位右心房到冠状窦远端传导时间比较,差异均无统计学意义(P>0.05);心房颤动组起搏时间300、280 ms时高位右心房到冠状窦远端传导时间较对照组延长(P<0.05)。心房颤动组起搏时间500、400 ms时低位右心房到冠状窦近端、远端传导时间较对照组延长(P<0.05);对照组与心房颤动组起搏时间350、300、280 ms时低位右心房到冠状窦近端、远端传导时间比较,差异均无统计学意义(P>0.05)。结论 阵发性心房颤动患者冠状窦组织和冠状窦心房交界处存在传导延缓,可能参与心房颤动的促发及维持。
心房颤动;脉冲射频术;不应期,电生理学
林明宽,刘浩,周婷.阵发性心房颤动患者左右心房电传导特点的临床研究[J].中国全科医学,2015,18(24):2997-3000.[www.chinagp.net]
Lin MK,Liu H,Zhou T.Clinical study of the characteristics of electrical conduction between left and right atriums in patients with paroxysmal atrial fibrillation[J].Chinese General Practice,2015,18(24):2997-3000.
冠状窦是心房间传导通路之一,尤其在心房下部间的传导中占据优势地位。冠状窦肌肉组织连接右心房和左心房,是心房间电传导的部分,也是Bachmann束的一部分[1]。Saremi等[2]研究65例正常窦性心律患者及7例心房颤动患者的冠状动脉CT,发现正常组58例显示有冠状窦-左心房肌性连接存在,心房颤动组患者均显示有冠状窦-左心房肌性连接。陈芳等[3]研究发现,冠状窦内存在1条左右心房间的特殊传导束,可能是一定条件下诱发并维持房性心律失常的心房间传导通路之一。冠状窦肌肉组织也是触发活动和房性心律失常的根源[4-6]。冠状窦肌肉组织传导延缓还与折返倾向和房性心律失常相关[7-9]。本课题组前期研究表明,阵发性心房颤动患者中,冠状窦肌肉组织存在传导延迟[10]。关于阵发性心房颤动患者左右心房电传导特点未见报道。本文探讨阵发性心房颤动患者左右心房电传导的特点,为明确阵发性心房颤动的发生机制提供一定的理论依据。
1 资料与方法

1.2 电生理检查 以1%利多卡因局部麻醉,分别穿刺右侧股静脉及右侧颈内静脉。置入6 F鞘管,放置电生理导管于希氏束和冠状窦。冠状窦电极(圣犹达生物科技有限公司,美国,电极间距2-8-2-8-2-8-8-2 mm)放置良好。记录电生理仪为电生理及导管工作站Combolab 7000(USA G.E)、心脏电生理刺激仪为东方DF-5A型(苏州市东方电子仪器厂)。希氏束电极放置:电极进入右心室后回撤,使导管顶端位于右房室瓣口处,头端指向后上方,可同时记录到大致相等的A波和V波,在A波和V波之间可见H波。冠状窦电极放置:(1)左前斜位透视冠状窦口位于膈肌上2~3 cm,第9胸椎左侧缘。(2)心内电生理图显示右心房为大A波,冠状窦近端及远端为大A波小V波,A波时相在P波终末,V波与QRS波同相。(3)行冠状窦造影证实冠状窦位置,以确认冠状窦近端电极在冠状窦口。高位右心房电极放置:经股静脉送至右心房与上腔静脉交界处,贴近心房外侧壁,导管尾端1~2极与多导记录仪连接,显示大A波,与体表心电图P波起点同相。低位右心房电极放置:电极顶端置于下腔静脉与右心房侧面交界处,既可记录到A波,也可记录到V波。
1.3 刺激方案 消融前,固定程序SIS。500、400、350、300、280 ms分别起搏冠状窦近端(9~10极)、冠状窦远端(1~2极)。电压4~8 V,脉宽0.5 ms,测量时纸速400 mm/s。程控刺激:分别于冠状窦近端、远端行S1S1刺激和S1S2刺激,S1S1刺激:刺激周长为500 ms;S1S2刺激,按8∶1比例释放,联律周期从350 ms开始递减,步长-10 ms,直至局部心肌组织有效不应期。
1.4 高位、低位右心房到冠状窦近端、远端传导时间测量 起搏高位右心房及低位右心房时,分别测量高位右心房A波起始到冠状窦近端A波起始、远端A波起始的传导时间;测量低位右心房A波起始到冠状窦近端A波起始、远端A波起始的传导时间。连续测量3个心动周期取其平均值。

2 结果
2.1 对照组与心房颤动组冠状窦近端、远端不应期比较 对照组与心房颤动组冠状窦近端、远端不应期比较,差异均无统计学意义(P>0.05,见表1)。

Table 1 Comparison of the refractory period in the proximal end and the distal end of coronary sinus between control group and AF group
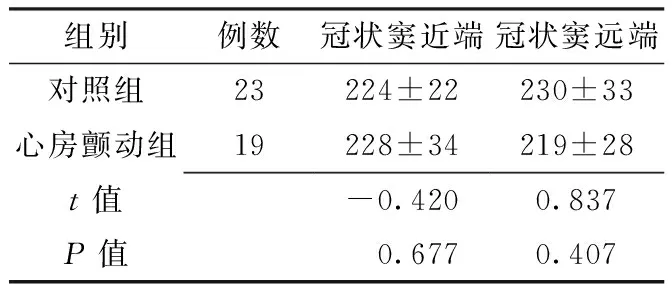
组别例数冠状窦近端冠状窦远端对照组23224±22230±33心房颤动组19228±34219±28t值-0.4200.837P值 0.6770.407
2.2 对照组与心房颤动组不同起搏时间高位右心房到冠状窦近端、远端传导时间比较 对照组与心房颤动组不同起搏时间高位右心房到冠状窦近端传导时间比较,差异均无统计学意义(P>0.05);对照组与心房颤动组起搏时间500、400、350 ms时高位右心房到冠状窦远端传导时间比较,差异均无统计学意义(P>0.05);对照组与心房颤动组起搏时间300、280 ms时高位右心房到冠状窦远端传导时间比较,差异均有统计学意义(P<0.05,见表2)。
2.3 对照组与心房颤动组不同起搏时间低位右心房到冠状窦近端、远端传导时间比较 对照组与心房颤动组起搏时间500、400 ms时低位右心房到冠状窦近端、远端传导时间比较,差异均有统计学意义(P<0.05);对照组与心房颤动组起搏时间350、300、280 ms时低位右心房到冠状窦近端、远端传导时间比较,差异均无统计学意义(P>0.05,见表3)。
3 讨论
冠状窦有助心房颤动的促发和维持通过其传导特性[11]。冠状窦提供右心房和左心房的传导缓慢连接,导致冠状窦和冠状窦左心房交界处激动延迟。冠状窦的慢传导和传导阻滞便于折返性心动过速沿冠状窦和冠状窦心房交界处传导。冠状窦肌肉组织的折返电路可能是心房颤动的机制。

Table 2 Comparison of the conduction time from HRA to the proximal end and the distal end of coronary sinus at different time points of pacemaking between control group and AF group
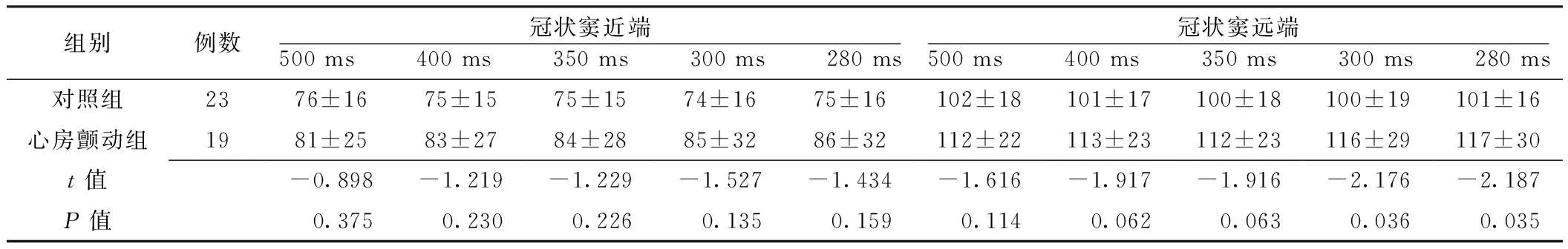
组别例数冠状窦近端500ms 400ms 350ms 300ms 280ms冠状窦远端500ms 400ms 350ms 300ms 280ms对照组2376±1675±1575±1574±1675±16102±18101±17100±18100±19101±16心房颤动组1981±2583±2784±2885±3286±32112±22113±23112±23116±29117±30t值-0.898-1.219-1.229-1.527-1.434-1.616-1.917-1.916-2.176-2.187P值0.3750.2300.2260.1350.1590.1140.0620.0630.0360.035

Table 3 Comparison of the conduction time from LRA to the proximal end and the distal end of coronary sinus at different time points of pacemaking between control group and AF group
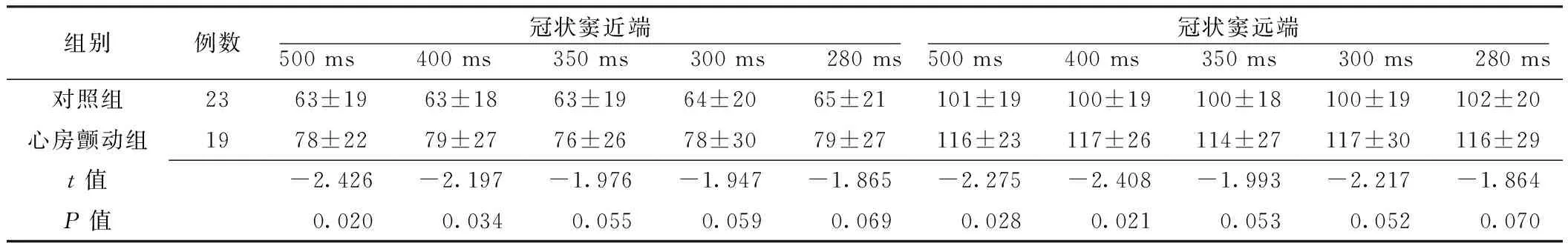
组别例数冠状窦近端500ms 400ms 350ms 300ms 280ms冠状窦远端500ms 400ms 350ms 300ms 280ms对照组2363±1963±1863±1964±2065±21101±19100±19100±18100±19102±20心房颤动组1978±2279±2776±2678±3079±27116±23117±26114±27117±30116±29t值-2.426-2.197-1.976-1.947-1.865-2.275-2.408-1.993-2.217-1.864P值0.0200.0340.0550.0590.0690.0280.0210.0530.0520.070
研究发现,持续性心房颤动患者和阵发性心房颤动患者Bachmann束不应期较对照组长,持续性心房颤动患者冠状窦口有效不应期较对照组长[12]。本研究发现,阵发性心房颤动组和对照组冠状窦近端和远端不应期无差异,和上述研究结果不一致。主要考虑以下原因:样本量小不足以产生统计学差异;与入选的心房颤动类型有关,国外试验入选的是持续性心房颤动患者,而本研究入选的是阵发性心房颤动患者。
本研究发现,对照组和心房颤动组高位右心房到冠状窦远端传导时间有差异,起搏时间300、280 ms时显著;对照组和心房颤动组低位右心房到冠状窦近端、远端传导时间有差异,起搏时间500、400 ms时显著,说明心房颤动患者左右心房间存在传导延缓或阻滞。本研究和国外Platonov等[13]研究发现,对冠状窦远端进行程序刺激,阵发性心房颤动患者右心房到冠状窦近端传导时间比对照组长〔(110±47)ms与(69±16)ms,P<0.05〕相似。递减起搏,持续性心房颤动患者在Bachmann束和冠状窦口的传导时间比阵发性心房颤动或对照组延长[12]。研究发现,89%存在冠状窦远端-左心房传导阻滞的患者,均有心房颤动或非典型房扑发作史[8]。冠状窦组织的传导延缓增加了房性心律失常的倾向[7]。Morita等[14]研究发现,犬冠状窦-心房连接处的电传导变慢。所以,冠状窦与左右心房间发生传导延缓或传导阻滞,易导致折返形成,继而诱发心房颤动。
本研究证实,心房颤动患者冠状窦存在电传导延缓或传导阻滞,但具体机制仍不清楚,可能与心房颤动患者的电重构和解剖重构有关,还有待进一步试验研究证实。
综上所述,冠状窦组织和冠状窦心房交界的电传导延缓或传导阻滞可能是心房颤动促发和维持的潜在机制。在心房颤动患者中,冠状窦局部存在电传导延缓或传导阻滞,通过改变这些电传导特性,可为心房颤动射频消融术提供新的治疗策略。本研究还存在一定局限性:样本量少对结果可能产生一定的误差,今后还需进一步大样本的前瞻性研究。
利益冲突声明:本课题未涉及任何厂家及相关雇主或其他经济组织直接或间接的经济或利益的赞助。无利益冲突。
[1]Ludinghausen VM,Ohmachi N,Boot C.Myocardial coverage of the coronary sinus and related veins[J].Clin Anat,1992,5(1):1-15.
[2]Saremi F,Thonar B,Sarlaty T,et al.Posterior interatrial muscular connection between the coronary sinus and left atrium:anatomic and functional study of the coronary sinus with multidetector CT[J].Radiology,2011,260(3):671-679.
[3]Chen F,Yang SN,Wang T,et al.The role of coronary sinus musculature on electrical conduction between left atrium and right atrium in isolated canine heart[J].Chinese Journal of Cardiology,2008,36(9):834-837.(in Chinese) 陈芳,杨沙宁,王腾,等.犬冠状窦肌组织在左右心房间电传导中的作用[J].中华心血管病杂志,2008,36(9):834-837.
[4]Wit A.Coronary sinus electrophysiology and arrhythmogenesis:historical development//Chen S,Haissaguerre M,Zipes D,et al.Thoracic Vein Arrhythmias:Mechanism and Treatment[M].Malden,Massachusetts:Blackwell,2004:21-29.
[5]Rotter M,Sanders P,Takahashi Y,et al.Images in cardiovascular medicine:coronary sinus tachycardia driving atrial fibrillation[J].Circulation,2004,110(6):e59-60.
[6]Yamada T,Murakami Y,Plumb VJ,et al.Focal atrial fibrillation originating from the coronary sinus musculature[J].Heart Rhythm,2006,3(9):1088-1091.
[7]Katritsis D,Ioannidis JP,Giazitzoglou E,et al.Conduction delay within the coronary sinus in humans:implications for atrial arrhythmias[J].J Cardiovasc Electrophysiol,2002,13(9):859-862.
[8]Kasai A,Anselme F,Saoudi N.Myocardial connections between left atrial myocardium and coronary sinus musculature in man[J].J Cardiovasc Electrophysio,2001,12(9):981-985.
[9]Antz M,Otomo K,Arruda M,et al.Electrical conduction between the right atrium and the left atrium via the musculature of the coronary sinus[J].Circulation,1998,98(17):1790-1795.
[10]周婷,刘浩,曾晓春,等.阵发性心房颤动患者冠状静脉窦电传导改变的研究[J].实用医学杂志,2013,29(19):3197-3199.
[11]Antz M,Otomo K,Arruda M,et al.Electrical conduction between the right atrium and the left atrium via the musculature of the coronary sinus[J].Circulation,1998,98(17):1790-1795.
[12]O′Donnell D,Bourke JP,Fumiss SS.Interatrial transseptalf electrical conduction:comparison of patients with atrial fibrillation and normal controls[J].J Cardiovasc Electrophysiol,2002,13(11):1111-1117.
[13]Platonov PG,Yuan S,Hertervig E,et al.Further evidence of localized posterior interatrial conduction delay in lone paroxysmal atrial fibrillation[J].Europace,2001,3(2):100-107.
[14]Morita H,Zipes DP,Morita ST,et al.The role of coronary sinus musculature in the induction of atrial fibrillation[J].Heart Rhythm,2012,9(4):581-589.
修回日期:2015-06-15)
(本文编辑:陈素芳)
Clinical Study of the Characteristics of Electrical Conduction Between Left and Right Atriums in Patients With Paroxysmal Atrial Fibrillation
LINMing-kuan,LIUHao,ZHOUTing.
Post-GraduateofElectrophysiology,GuangxiMedicalUniversity,Nanning530021,China
Objective To study the characteristics of electrical conduction between left and right heart atriums in patients with paroxysmal atrial fibrillation (PAF).Methods Enrolled 19 PAF patients who received pulsed radiofrequency treatment into the First Affiliated Hospital of Guangxi Medical University from April 2012 to May 2013 as AF group.And another 23 patients with paroxysmal supraventricular tachycardia or ventricular premature contraction were enrolled as control group.A fixed program of SIS was applied.At 500,400,350,300 and 280 ms,pace-making was made in high right atrium (HRA) and low right atrium (LRA),and we measured the refractory period in the proximal end and the distal end of coronary sinus and the conduction time from HRA and LRA to the proximal end and the distal end of coronary sinus.Results Control group and AF group were not significantly different (P>0.05) in the refractory period in the proximal end and distal end of coronary sinus.Control group and AF group were not significantly different (P>0.05) in the conduction time from HRA to the proximal end of coronary sinus at different time points of pace-making;control group and AF group were not significantly different (P>0.05) in the conduction time from HRA to the distal end of coronary sinus at 500,400,350 ms of pace-making;the AF group was higher (P<0.05) than control group in the conduction time from HRA to the distal end of coronary sinus at 300 and 280 ms of pacemaking.AF group was higher (P<0.05) than the control group in the conduction time from LRA to the proximal end and the distal end of coronary sinus at 500 and 400 ms of pacemaking;the control group and the AF group were not significantly different (P>0.05) in the conduction time from LRA to the proximal end and the distal end of coronary sinus.Conclusion Conduction delay exists in the coronary sinus and the junction of coronary sinus and heart atrium,which may be involved in the onset and sustaining of atrial fibrillation.
Atrial fibrillation;Pulsed radiofrequency treatment;Refractory period,electrophysiological
广西医疗卫生重点科研课题资助项目(桂卫重200923)
530021广西南宁市,广西医科大学电生理专业硕士研究生(林明宽);广西医科大学第一附属医院心内科(刘浩),胸外科(周婷)
刘浩,530021广西南宁市,广西医科大学第一附属医院心内科;E-mail:Liuhaomd@163.com
R 541.75
A
10.3969/j.issn.1007-9572.2015.24.026
2014-12-21;