Applied anatomical study of the vascularized ulnar nerve and its blood supply for cubital tunnel syndrome at the elbow region
Mei-xiu-li Li, Qiong He, Zhong-lin Hu, Sheng-hua Chen, Yun-cheng Lv, Zheng-hai Liu, Yong Wen, Tian-hong Peng,
1 Laboratory of Clinical Anatomy, University of South China, Hengyang, Hunan Province, China
2 Department of Radiology, Chen-xi Hospital, Huaihua, Hunan Province, China
Applied anatomical study of the vascularized ulnar nerve and its blood supply for cubital tunnel syndrome at the elbow region
Mei-xiu-li Li1, Qiong He1, Zhong-lin Hu2, Sheng-hua Chen1, Yun-cheng Lv1, Zheng-hai Liu1, Yong Wen1, Tian-hong Peng1,*
1 Laboratory of Clinical Anatomy, University of South China, Hengyang, Hunan Province, China
2 Department of Radiology, Chen-xi Hospital, Huaihua, Hunan Province, China
Cubital tunnel syndrome is often accompanied by paresthesia in ulnar nerve sites and hand muscle atrophy. When muscle weakness occurs, or after failure of more conservative treatments, anterior transposition is used. In the present study, the ulnar nerve and its blood vessels were examined in the elbows of 18 adult cadavers, and the external diameter of the nutrient vessels of the ulnar nerve at the point of origin, the distances between the origin of the vessels and the medial epicondyle of the humerus, and the length of the vessels accompanying the ulnar nerve in the superior ulnar collateral artery, the inferior ulnar collateral artery, and the posterior ulnar recurrent artery were measured. Anterior transposition of the vascularized ulnar nerve was performed to treat cubital tunnel syndrome. The most appropriate distance that the vascularized ulnar nerve can be moved to the subcutaneous tissue under tension-free conditions was 1.8 ± 0.6 cm (1.1-2.5 cm), which can be used as a reference value during the treatment of cubital tunnel syndrome with anterior transposition of the vascularized ulnar nerve.
nerve regeneration; ulnar nerve; blood supply; compressive neuropathy; cubital tunnel syndrome; superior ulnar collateral artery; inferior ulnar collateral artery; posterior ulnar recurrent artery; anterior transposition; neural regeneration
Funding:This study was supported by the Hunan Provincial Science and Technology Research Project Foundation for Colleges and Universities in China, No. 12A119; Construct Program of the Key Discipline in Hunan Province, China.
Li MXL, He Q, Hu ZL, Chen SH, Lv YC, Liu ZH, Wen Y, Peng TH (2015) Applied anatomical study of the vascularized ulnar nerve and its blood supply for cubital tunnel syndrome at the elbow region. Neural Regen Res 10(1):141-145.
Introduction
Ulnar nerve compression at the elbow, known as cubital tunnel syndrome, is the second most frequently seen compression neuropathy, after carpal tunnel syndrome (Contreras et al., 1998; Mitsionis et al., 2010). Regardless of what causes the volume of the cubital tunnel to shrink or the pressure on the ulnar nerve to increase, such effects can decrease the blood supply to the ulnar nerve directly or indirectly, causing peripheral nerve entrapment syndrome. Patients with cubital tunnel syndrome often also display other symptoms such as paresthesia in the ulnar nerve distribution and weakness or atrophy of the intrinsic musculature of the hand (Palmer and Hughes, 2010). Unfortunately, there is no gold standard for diagnosing cubital tunnel syndrome. Surgical treatment for cubital tunnel syndrome is indicated with motor weakness or when conservative measures have failed (Sugawara, 1988). The common surgical treatments include in situ decompression, subcutaneous transposition, intramuscular transposition, medial epicondylectomy, and anterior transposition (Palmer and Hughes, 2010). Among these treatments, decompression and anterior transposition of the ulnar nerve are the most commonly used surgical procedures (Bartels et al., 1998; Ochi et al., 2013). However, protection of the blood supply of the ulnar nerve and controlling the appropriate distance that the ulnar nerve is transposed anteriorly are critical when performing anterior transposition of the vascularized ulnar nerve (Zhou et al., 2005). There is currently no consensus among many published studies in the literature on how to best protect the blood supply of the ulnar nerve and what distance the nerve should be anteriorly transposed. Therefore, the aim of the present study was to observe and measure the ulnar nerve and its blood vessels at the elbow, and to simulate anterior transposition of the vascularized ulnar nerve in order to determine the most appropriate distance that the vascularized ulnar nerve at the cubital tunnel can be moved during the treatment of cubital syndrome.
Materials and Methods
Materials
This study used 18 cadaver specimens that had been prepared for educational use by the medical students in theDepartment of Anatomy, University of South China, China. The anatomy of the ulnar nerve and the blood vessels that supplied it in thirty upper extremities were examined after the injection of red-colored latex (Yunnan Natural Rubber Industrial Co., Ltd., Kunming, Yunnan Province, China). Six additional fresh adult upper limbs that were injected with a modifed gelatin-lead oxide mixture were also examined. The gelatin-lead oxide mixture was prepared as follows. First, 5 g of gelatin (Shijiazhuang JinDa Gelatin Co., Ltd., Hebei Province, China) was diluted in 100 mL of tap water at 40°C and 100 g of water-soluble red lead oxide (Tianjin Kermel Chemical Reagents Co., Ltd., Tianjin, China) was added. The average age of the cadavers at death was 68 years (range: 41 to 87 years). The examined regions had no history of surgical procedures, trauma, or vascular disease.
Observation of the ulnar nerve and its blood vessels in the elbow region
First, the ulnar nerve and its blood supply in the elbow region were observed from thirty adult upper extremities that had been injected with red-colored latex. A vernier caliper (Xin-lai Instrument, Guangzhou, Guangdong Province, China) was used to measure the external diameter of the nutrient vessels of the ulnar nerve at the point of origin. A straightedge (Jia-jia stationery, Shenzhen, Guangdong Province, China) was used to measure the distances between the origin of the vessels and the medial epicondyle of the humerus, and the length of the vessels accompanying the ulnar nerve was measured using a vernier caliper. Next, an imaginary line was drawn between the medial epicondyle of the humerus and the high point of the olecranon of the ulnar in order to measure the diameter of the cubital tunnel. The ulnar nerve at the elbow on one cadaver’s upper limb had been dissected and modifed such that the spatial relationship between the ulnar nerve and its blood supply could be observed clearly.
Blood vessels nurturing the ulnar nerve were observed by X-ray examination
X-rays (Philips, Amsterdam, Netherlands) were taken that recorded the anastomosis of the blood vessels that nurture the ulnar nerve in six upper limbs of fresh adult cadavers that had been injected with modifed gelatin-lead oxide 24 hours prior to the examination.
Measurement of the range of anterior transposition of ulnar nerve under tension-free conditions
A simulation of the clinical surgical procedure was performed in thirty upper limbs of adult cadavers that were injected with red-colored latex. The straightedge was used to measure the range of anterior transposition of the ulnar nerve while maintaining tension-free conditions.
Statistical analysis
All data were analyzed with SPSS 18.0 software (SPSS, Chicago, IL, USA) and were expressed as the mean ± SD with ranges showing the minimal to maximal values (min-max).
Results
Trunk and branches of the ulnar nerve at the cubital tunnel
The ulnar nerve proceeded through the cubital tunnel and was surrounded by the fexor carpi ulnaris, arcuate ligaments (among the fbrous fascia tissue at the olecranon), and the groove of the ulnar nerve of the humerus in all specimens. The ulnar nerve then entered the forepart of the forearm among the heads of the fexor carpi ulnaris. The diameter of the ulnar nerve at the cubital tunnel was 4.9 ± 1.3 mm (range: 3.6-5.8 mm), and the diameter of the cubital tunnel was 6.0 ± 1.9 mm (range: 4.9-8.2 mm). The ulnar nerve was observed to release 1-2 joint branches that were distributed to the posterior internal elbow joint and 2-3 muscle branches to the fexor carpi ulnaris (Figure 1).
Blood supply of the ulnar nerve at the elbow
Three major arteries were found that supply blood to the ulnar nerve at the elbow: the superior ulnar collateral artery, the inferior ulnar collateral artery, and the posterior ulnar recurrent artery. The external diameter of the ulnar nerve nutrient vessels at its point of origin, the distance between the origin of the arteries and the medial epicondyle of the humerus, and the length of the vessels accompanying the ulnar nerve are shown inTable 1.
Among the thirty limb specimens, the superior ulnar collateral artery originated from the brachial artery (in 28 limbs, 93%) or the deep brachial artery (in 2 limbs, 7%) in the upper third of the arm. Then, it proceeded down with the ulnar nerve and issued 3-6 branches that were distributed vertically into the ulnar nerve. These branches were divided into ascending and descending branches under the adventitia of the ulnar nerve. The descending branches fnally anastomosed with the branches coming from the inferior ulnar collateral artery or posterior ulnar recurrent artery at the elbow. The posterior ulnar recurrent artery split off of the ulnar artery and gave off a volaris branch and a dorsal branch 1 cm from the origin point. The dorsal branch travelled from bottom to top and gave off 2-4 branches into the deep surface of the flexor carpi ulnaris before entering the nerve at the distal elbow. The trunk of the posterior ulnar recurrent artery ran upwards, and its terminals anastomosed with the superior ulnar collateral artery or inferior ulnar collateral artery. The inferior ulnar collateral artery originated from the brachial artery (in 27 limbs, 90%) or the ulnar recurrent artery (in 3 limgs, 10%). The trunk of the inferior ulnar collateral artery ran into the forepart of the medial humerus and then split into the volaris branch and the dorsal branch. The dorsal branch pierced the medial intermuscular septum and its terminals anastomosed with the superior ulnar collateral artery and inferior ulnar collateral artery after issuing 1-2 branches to supply the ulnar nerve and its projections. All the terminal branches of the superior ulnar collateral artery anastomosed with the dorsal branches of the posterior ulnar recurrent artery in all thirty upper limbs, and some dorsal branches of the inferior ulnar collateral artery (in 4 limbs, 13.3%) were affliated and anastomosedwith them. The rami anastomoticus, which was located in the deep fascia of the elbow anteriomedialis, proceeded towards the ulnar along an arc. The spatial relationship between the ulnar nerve and blood vessels was clearly observed in the upper limbs after removing the muscle and fascia. The superior ulnar collateral artery and posterior ulnar recurrent artery, which accompanied the ulnar nerve, were longer than the inferior ulnar collateral artery. The trunks of the superior ulnar collateral artery, posterior ulnar recurrent artery, and inferior ulnar collateral artery, as well as their branches, penetrated the ulnar nerve posterolaterally, and the terminal branches anastomosed with each other at the surface of the ulnar nerve, forming the epineurium vessels of the ulnar nerve. The characteristics of the superior ulnar collateral artery, posterior ulnar recurrent artery, inferior ulnar collateral artery, and the vascular anastomosis network formed from their terminals were observed using radiography on the specimens injected with modifed gelatin-lead oxide (Figure 2).

Table 1 Dimensions of the vasculature supplying the ulnar nerve
Simulation of anterior transposition of the ulnar nerve
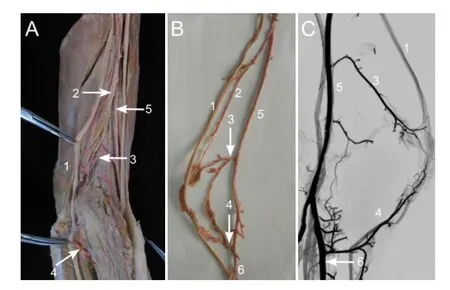
Figure 2 Arrangement of the blood supply to the ulnar nerve at the elbow.
An approximately 15-cm longitudinal incision was made around the medial epicondyle, and then the skin, superficial fascia, and deep fascia were dissected to clearly expose the cubital tunnel and the ulnar nerve. The superior ulnar collateral artery, inferior ulnar collateral artery, posterior ulnar recurrent artery, and the anastomosis of their branches with the accompanying vessels were identifed and displayed along the ulnar nerve. The branches of the superior ulnar collateral artery were distributed in the triceps brachii muscle. In addition, the trunk of the superior ulnar collateral artery ran parallel to the ulnar nerve and produced many branches that supplied the ulnar nerve. One of the branches of the inferior ulnar collateral artery crossed the trunk of the ulnar nerve, producing additional minor branches that fed into it (Figure 2A). Thus, ligating the muscular branches of the superior ulnar collateral artery, while preserving the integrity of the deep fascia around the vessels and nerves during the operation, is safe and does not injure the nervous branches of the superior ulnar collateral artery. As another main artery originating from the ulnar artery, the branches of the posterior ulnar recurrent artery provide nutrition deep into the ulnar nerve by reaching to the deep face of the fexor carpi ulnaris at the distal end of the cubital tunnel. Before the ulnar nerve and its nutrient vessels can be safely separated and transposed to the subcutaneous tissue anterior to the medial epicondyle, great care and consideration must be taken to ensure that the blood vessels and deep fascia around the nerve are left intact. From the surgical simulations, we concluded that the appropriate distance that one can transpose the vascularized ulnar nerve is 1.8 ± 0.6 cm (1.1-2.5 cm) anteriorly without putting it under tension.
Discussion
Characteristics of the ulnar nerve and its blood supply at the elbow
A detailed knowledge of the anatomy of the ulnar nerve is critical for diagnosing and treating cubital tunnel syndrome. The ulnar nerve is derived from the C8and T1nerve roots.Although the ulnar nerve may be compressed at any position along its length, the most common place is at the elbow, especially in the cubital tunnel (Kroonen, 2012). In physiological conditions, the cubital tunnel volume and pressure change with flexion and extension of the elbow; when the elbow is in fexion, the cubital tunnel pressure becomes signifcantly higher (Jones and Gauntt, 1979; Macnicol, 1982; Wilgis and Murphy, 1986). In particular, repetitive fexion of the elbow can lead to infammation and edema surrounding the ulnar nerve, which inhibits the normal gliding action of the nerve and increases the strain (Ochi et al., 2013). Therefore, the basic anatomical biomechanics of the cubital tunnel syndrome includes the ulnar nerve being pulled, rubbed, and injured in the cubital tunnel when the elbow joint undergoes fexion and extension (Jones and Gauntt, 1979). The results presented here show that the diameter of the ulnar nerve is similar to that of the cubital tunnel, which suggests that changes in the anatomy of the cubital tunnel or ulnar nerve can lead to cubital tunnel syndrome. The blood supply to the peripheral nerve is provided in segments by the accompanying vessels, for example the epineurial blood vessels, the endoneurium vasoganglion, and the micro-vasoganglion within the nerve bundle. Three major arteries supply the ulnar nerve at the cubital tunnel: the superior ulnar collateral artery, inferior ulnar collateral artery, and posterior ulnar recurrent artery. Breidenbach and Terzis (1986) reported that the superior ulnar collateral artery is the main blood vessel at the elbow, but they did not differentiate between the superior ulnar collateral artery and the posterior ulnar recurrent artery. In the present study based on a series of anatomical observations, we found that the superior ulnar collateral artery is the main nutrient vessel of the ulnar nerve in the upper arm, but that the posterior ulnar recurrent artery is the main nutrient vessel in the cubital tunnel. Consequently, the inferior ulnar collateral artery acts as a bridge, anastomosing the superior ulnar collateral artery and the posterior ulnar recurrent artery near the junction of the cubital tunnel with the ulnar nerve tunica external vessels. Prevel et al. (1993) dissected and observed eighteen elbow joints, but found the segmental vessels originating from the inferior ulnar collateral artery in only fve specimens. In contrast, among the thirty specimens examined here, we found twenty-two joints with segmental vessels originating from the inferior ulnar collateral artery. If one of the nutrient vessels becomes damaged, the segmental arteries and vasoganglion of the ulnar nerve may be able to compensate. The ulnar nerve divides into 2-3 muscular branches and 1-2 joint branches at the elbow (Taylor and Palmer, 1987). Taylor and Palmer’s standard for characterizing the nerve blood supply suggests that the elbow ulnar nerve blood supply is type E: the branches of the nerve are complicated and receive blood supply from different sources. Therefore, it is not suitable for use as donor tissue for free vascularized nerve grafts. However, the blood of the ulnar nerve at the elbow is segmentally supplied by three segments distributed at the superior ulnar collateral artery, inferior ulnar collateral artery, and posterior ulnar recurrent artery, i.e., the vasoganglion within the fasciculus, the vasoganglion vessel in the epineurium, and the vessel between the fasciculi. Lundborg (1979) divided the peripheral nerve vessels into internal and external vessels. The superior ulnar collateral artery, inferior ulnar collateral artery, and posterior ulnar recurrent artery, as well as their respective segmental arteries, are external ulnar vessels at the elbow, which should be carefully protected when the ulnar nerve is moved during anterior transposition. The lengths of these three vessels that accompany the ulnar nerve are longer than that from the origin of the arteries to the medial epicondyle, which allows excessive traction of the ulnar nerve to be avoided during the anterior transposition of the ulnar nerve. Therefore, anterior transposition of the vascularized ulnar nerve is feasible as a way to treat cubital tunnel syndrome, while still maintaining the blood supply to the ulnar nerve.
Clinical signifcance of protecting the blood supply to the ulnar nerve
The etiological factors that contribute to cubital tunnel syndrome include mechanical pressure, chronic ischemic injury, and their interactions in the elbow (Bartels, 2001; Kroonen, 2012). In a healthy person, the pressure in the cubital tunnel at the elbow during flexion is far stronger than that at the elbow during extension. With repeated elbow flexion, the pressure in the cubital tunnel increases, decreasing the blood supply to the ulnar nerve in the cubital tunnel. Peripheral nerves such as the ulnar nerve can easily become dysfunctional if the normal oxygen tension within the nerve tissue is disturbed (Prevel et al., 1993). In fact, anything that decreases the oxygen supply to the ulnar nerve causes temporary, or sometimes permanent, damage to the ulnar nerve. Thus, it is important to ensure that the blood supply to the ulnar nerve is not interrupted, especially during anterior transposition. The results of the present study show that the superior ulnar collateral artery is the main nutrient vessel in the upper arm and the posterior ulnar recurrent artery is the main blood vessel in the elbow. Therefore, in order to protect the integrity of the posterior ulnar recurrent artery and its branches during the operation, the muscular branches of the inferior ulnar collateral artery and the articular branches of the ulnar nerve are frst ligated so that the fascia around them can be preserved. The results reported by Sugawara et al. (1988) after investigating the blood supply of the ulnar nerve in dogs indicated that at least 80% of the blood supply could be preserved if the accompanying vessels were kept intact during the anterior transposition. On the contrary, if the accompanying vessels are ligated, only 45% of the blood supply could be preserved. Ogata et al. (1991) showed that the signal that stimulates the nerve conduction velocity was signifcantly reduced when the ulnar nerve was in segmental ischemia. Therefore, protecting the blood supply to the ulnar nerve is particularly important. Anterior transposition can fundamentally reduce the risk factors for cubital tunnel syndrome by maintaining the blood supply to the ulnar nerve while avoiding ulnar nerve compression, traction, and mechanical friction at the cubital tunnel. During anterior transposition, the ulnar nerve is relocated into the subcutaneousareolar tissue, where it can move easily, which is beneficial for the repair of nerve lesions and to achieve better results. Nevertheless, this relocation can affect the function of ulnar nerve and its blood supply if it is excessively released, dissociated, or injured during the anterior transposition operation. Therefore, how to best relieve nerve compression, while maintaining the blood supply to the ulnar nerve, is a problem of clinical signifcance.
Findings regarding anterior transposition with the blood supply of the ulnar nerve
The data reported here suggest several important findings regarding anterior transposition with the blood supply of the ulnar nerve. First, the length of the incision should be at least 10 cm. In the present study, we used longitudinal incisions of about 15 cm to allow total decompression of the ulnar nerve. To prevent the ulnar nerve from leaving its groove after the operation, the position of the incision should be such that it lies in the anterior groove of the ulnar nerve of the medial epicondyle of the humerus. In that position, the anterior transposition of the ulnar nerve can then be covered by the large and loose skin folds available at the elbow. Second, the ulnar nerve that lies in the superior-medial elbow should be dissected first, and then the ulnar nerve that is located in the cubital tunnel. In this step, the ulnar nerve in the cubital tunnel can be clearly seen during the operation, making it easier to separate and avoid injuring the accompanying vessels. Finally, in order to form a new tunnel at the elbow after subcutaneous anterior transposition of the ulnar nerve, the surgeon should suture the subcutaneous and deep fascia to prevent the ulnar nerve from sliding back into the original ulnar nerve groove.
Compared with conventional experiments that only use gross anatomy, radiology was used in the present study to show the ulnar nerve and its blood supply, which was also combined with a simulation of anterior transposition of the ulnar nerve to make our results more convincing. In future work, we would like to assess this technique in a clinical trial. We hypothesized that the ulnar nerve can be visualized directly under X-rays, and the release of the ulnar nerve under endoscope monitoring is a major developing trend. In fact, the results presented here provide anatomical data to help guide anterior transposition of the vascularized ulnar nerve for treating cubital tunnel syndrome.
In summary, anterior transposition of the vascularized ulnar nerve for treating cubital tunnel syndrome is feasible. The appropriate distance that the vascularized ulnar nerve can be moved into the subcutaneous tissue under tension-free conditions is 1.8 ± 0.6 cm (1.1-2.5 cm).
Author contributions:All authors participated in study design, experimental supervision, data acquisition, data analysis paper drafting and approved the final version of the paper.
Conficts of interest:None declared.
Bartels RH (2001) History of the surgical treatment of ulnar nerve compression at the elbow. Neurosurgery 49:391-400.
Bartels RH, Menovsky T, Van Overbeeke JJ, Verhagen WI (1998) Surgical management of ulnar nerve compression at the elbow: an analysis of the literature. J Neurosurg 89:722-727.
Breidenbach WC, Terzis JK (1986) The blood supply of vascularized nerve grafts. J Reconstr Microsurg 3:43-58.
Contreras MG, Warner MA, Charboneau WJ, Cahill DR (1998) Anatomy of the ulnar nerve at the elbow: potential relationship of acute ulnar neuropathy to gender differences. Clin Anat 11:372-378.
Jones RE, Gauntt C (1979) Medial epicondylectomy for ulnar nerve compression syndrome at the elbow. Clin Orthop Relat Res 174-178.
Kroonen LT (2012) Cubital tunnel syndrome. Orthop Clin N Am 43:475-486.
Lundborg G (1979) The intrinsic vascularization of human peripheral nerves: structural and functional aspects. J Hand Surg Am 4:34-41.
Macnicol MF (1982) Extraneural pressures affecting the ulnar nerve at the elbow. Hand 14:5-11.
Mitsionis GI, Manoudis GN, Paschos NK, Korompilias AV, Beris AE (2010) Comparative study of surgical treatment of ulnar nerve compression at the elbow. J Shoulder Elbow Surg 19:513-519.
Ochi K, Horiuchi Y, Nakamura T, Sato K, Arino H, Koyanagi T (2013) Ulnar nerve strain at the elbow in patients with cubital tunnel syndrome: effect of simple decompression. J Hand Surg Eur Vol 38:474-480.
Ogata K, Shimon S, Owen J, Manske PR (1991) Effects of compression and devascularisation on ulnar nerve function. A quantitative study of regional blood flow and nerve conduction in monkeys. J Hand Surg Br 16:104-108.
Palmer BA, Hughes TB (2010) Cubital tunnel syndrome. J Hand Surg Am 35:153-163.
Prevel CD, Matloub HS, Ye Z, Sanger JR, Yousif NJ (1993) The extrinsic blood supply of the ulnar nerve at the elbow: an anatomic study. J Hand Surg Am 18:433-438.
Sugawara M (1988) Experimental and clinical studies of the vascularized anterior transposition of the ulnar nerve for cubital tunnel syndrome. Nihon Seikeigeka Gakkai Zasshi 62:755-766.
Svernlöv B, Larsson M, Rehn K, Adolfsson L (2009) Conservative treatment of the cubital tunnel syndrome. J Hand Surg Eur Vol 34:201-207.
Taylor GI, Palmer JH (1987) The vascular territories (angiosomes) of the body: experimental study and clinical applications. Br J Plast Surg 40:113-141.
Wilgis EF, Murphy R (1986) The signifcance of longitudinal excursion in peripheral nerves. Hand Clin 2:761-766.
Zhou JL, Du RX, Wang QY, Liu QH, Meng XL, Wang ZW (2005) Anatomic and clinical study of anterior transposition of the vascularized ulnar nerve for cubital tunnel syndrome. Zhongguo Linchuang Jiepou Xue Zazhi 23:484-486.
Copyedited by McCarty W, Norman C, Yu J, Qiu Y, Li CH, Song LP, Zhao M
*Correspondence to: Tian-hong Peng, thpeng67@163.com.
10.4103/1673-5374.150723
http://www.nrronline.org/
Accepted: 2014-09-04
- 中国神经再生研究(英文版)的其它文章
- Letter from the Editors-in-Chief
- Fat cell-secreted adiponectin mediates physical exercise-induced hippocampal neurogenesis: an alternative anti-depressive treatment?
- Induced pluripotent stem cell-derived neural stem cell therapies for spinal cord injury
- “Bad regenerators” die after spinal cord injury: insights from lampreys
- Can cinnamon bring aroma in Parkinson’s disease treatment?
- Acupuncture: a potent therapeutic tool for inducing adult neurogenesis