Systemic Lupus Erythematosus and Antiphospholipid Syndrome Related Retinal Vasculitis Mimicking Ocular Cysticercosis: a Case Report
Department of Ophthalmology,Department of Rheumatology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing 00730, China
Systemic Lupus Erythematosus and Antiphospholipid Syndrome Related Retinal Vasculitis Mimicking Ocular Cysticercosis: a Case Report
Chan Wu1, Fang-tian Dong1*, You-xin Chen1, Qian Wang2, Rong-ping Dai1, and Hua Zhang1
1Department of Ophthalmology,2Department of Rheumatology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing 100730, China
systemic lupus erythematosus; antiphospholipid syndrome; retinal vasculitis; cysticercosis
Chin Med Sci J 2015; 30(1):59-62
M AKING accurate and timely diagnosis is often challenging when patients with a systemic disease first present with ocular manifestations. The possibility that vasculitis associated with systemic lupus erythematosus (SLE) and antiphospholipid syndrome (APS) can be misdiagnosed as cysticercosis has not been discussed in the literatures.
CASE DESCRIPTION
A 45-year-old woman was referred to the emergency department of our hospital with progressive vision loss bilaterally for 5 days. She also reported dyspnea and palpitation in the past 4 months which were worsening for a week before her presentation. She was suspected with ocular cysticercosis (OCC) in a local hospital because she was diagnosed with neurocysticercosis after a seizure 7 years ago. Cysticercal serum enzyme-linked immunoelectrotransfer blot assay was positive at that time, and intermittent treatment for cysticercosis was administered. She had consequent seizure recurrence several times since then and developed uncontrollable hypertension for 7 years, interstitial lung disease and anemia for 2 years. She suffered from spontaneous abortion 5 times. Her family history was unremarkable.
On examination, the best-corrected visual acuity (BCVA) in the right eye was 20/400, Jr7 and 20/200, Jr5 in the left eye. Intraocular pressure was normal bilaterally. Slit lamp examination of the right eye showed mild pupillary irregularity with mild relative afferent pupillary defect. Both eyes showed clear lens with no anterior chamber or vitreous reaction and no subconjunctival cyst. Dilated fundus examination revealed diffuse vasculitis with widespread intraretinal hemorrhages in both eyes. Additionally, yellow-white lesions of approximately 1.5 prism diopters were noticed across the macular area of both eyes. The optic nerve head showed 0.6 cupping in the right eye and 0.5 in the left eye with no papillary edema (Fig. 1A). Ultrasonography revealed vitreous opacities and round dense echoes corresponding to the macular lesions bilaterally (Fig. 1B). Optical coherence tomography (OCT)showed thickening neuroepithelium with a hyper-reflective portion within it in the macular area (Fig. 1C). Fluorescein angiography (FFA) of both eyes revealed slower filling of vessels and peripheral areas of nonperfusion. It also showed blocked fluorescence in the macular areas. The late phase FFA showed significant dye leakage from the retinal veins and abnormal vessels in nonperfusion areas (Fig. 1D).
The patient's general condition deteriorated 3 days later, and she was found to have severe mitral regurgitation with suspected vegetation. She also began to complain of pain in the right eye. Ophthalmological examination showed the BCVA of the right eye decreased to counting fingers at 1 meter. Intraocular pressure of the right eye was 43 mm Hg, while that of the left eye was normal. Slit lamp examination revealed significant iris neovascularization and corneal edema in the right eye. Dilated fundus examination revealed worsening intraretinal hemorrhages. Retinal vasculitis and neovascular glaucoma were considered. Panretinal photocoagulation and topical anti-glaucoma eye drops were administered immediately.
Her complete blood cell count revealed pancytopenia with normal eosinophil cell count. The urinalysis revealed proteinuria and red blood cells. The erythrocyte sedimentation rate was mildly elevated and the complement (CH50, C3, C4) levels decreased. Antibody measurements showed positive antinuclear antibody (ANA) and anticardiolipin antibody (ACLA), while the anticysticercus antibody was negative.
Magnetic resonance imaging of the brain showed multiple discrete white matter lesions in the right periventricular area and bilateral temporal lobes. The patient was diagnosed as systemic lupus erythematosus and antiphospholipid syndrome with lupus nephritis and neuropsychiatric lupus. Prednisolone in combination with cyclophosphamide was initiated. Intravitreal injection of triamcinolone acetonide and bevacizumab was applied to the right eye, and panretinal photocoagulation was continued in both eyes.
After above treatment for 2 weeks, the patient’s clinical condition was significantly improved. The ophthalmological examination showed improved vision in both eyes. The BCVA of the right eye was 20/1000, and the left eye was 20/50. Intraocular pressure of the right eye reduced to 20 mm Hg. Slit lamp examination revealed partial regression of iris neovascularization in the right eye and the cornea turned clear. The right pupil was larger and relative afferent pupillary defect was remarkable. Fundus examination showed the optic disc was pale in the right eyes with a cup-disk ratio of 0.9. The hemorrhages in both eyes were absorbed, and the macular yellow-white lesions disappeared (Fig. 2A). OCT showed the neuroepithelium of the fovea was thinning and the hyper-reflective area disappeared (Fig. 2B).
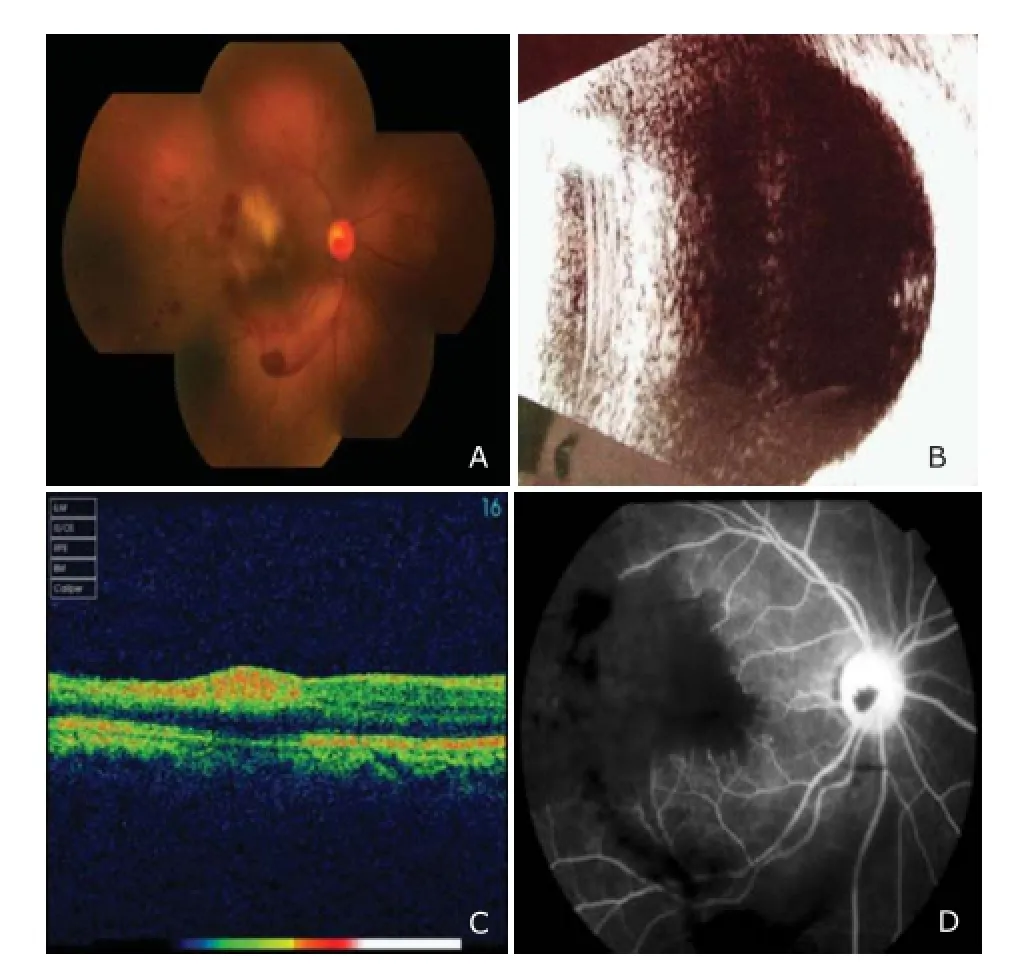
Figure 1.Patient at initial visit.

Figure 2.Patient after treatment.
DISCUSSION
Considering the previous diagnosis of neurocysticercosis and the positive cysticercal antibody, the doctors suspected this case as OCC initially. Cysticercus can settle in nearly all parts of the eye while the most favored sites for OCC are vitreous and subretinal spaces. The parasite is brought via the posterior ciliary arteries to the subretinal space, usually in the region of the posterior pole. The symptoms are determined by the location and size of cysts, host's immune status, and level of inflammatory reaction.1Retinal pigment epithelial disturbances, retinal detachment, retinal edema, intraretinal haemorrhage, and vascular sheathing are known to occur in intraocular cysticercosis.2Clinical outcomes can be devastating as the cysticercus increases in size, leading to blindness in 3 to 5 years, since death of the parasite can cause remarkable release of toxic products, leading to a profound inflammatory reaction such as vitreous inflammation, uveitis, retinal detachment, glaucoma etc. and destruction of the eye.3
Although OCC should be considered in this case, several important clinical clues of systemic autoimmune disease were missed. The sensitivity and specificity of serological testing vary depending on the number of cysts, location, and phase of infection. The test can be positive in patients who had been exposed to the adult parasite without developing cysticercosis.4Although seizure was reported as the primary or sole manifestation in almost 70% of cases,5this patient’s epilepsy showed no improvement after receiving specific treatment for cysticercosis. In addition, repetitive stillbirth and multiple systems involvement including anemia, interstitial lung disease, and thrombosis could hardly be explained by cysticercosis alone. In contrast, an autoimmune disease was strongly indicated in this young woman of childbearing age, especially SLE combined with APS.
Retinopathy is one of the most common vision-threatening complications of SLE, which usually indicates active systemic disease and is strongly correlated with central nervous system involvement.6Retinal vasculitis is a subset of retinal vasculopathy, which tends to be acute onset and have poorer visual outcomes. A large percentage of these patients with retinal vasculitis have concomitant antiphospholipid antibodies including anticardiolipin, lupus anticoagulant and anti-[beta]2-glycoprotein 1. In one study, 77% of patients of SLE with retinal involvement had positive antiphospholipid antibody titers, compared to 29% among SLE patients without retinal disease.7In 1984, Hall et al8first reported a link between severe lupus retinal vasculopathy and presence of antiphospholipid antibodies. While the milder form of retinal vasculopathy is mediated by immunocomplex deposition and inflammation, the more severe vaso-occlusive disease stems from fibrinoid degeneration or necrosis without significant inflammation.9
APS can affect blood vessels in all vascular segments and is characterized by hypercoagulability-related diverse symptoms, including ocular manifestations. The most frequent ocular manifestation is retinal thrombosis especially in young people, while 75% were women, with an approximate mean age of 40 years.10Classically, APS has been associated with central or branch retinal vein/artery occlusion. Retinal findings include venous tortuosity, dilation, and flame haemorrhages. Other findings include choroidal infarction, cilioretinal artery occlusion, microvascular retinopathy with cotton wool spots, peripheral retinal ischemia with neovascularization and hemorrhage, and macular choroidal neovascular membranes. Neuro-ophthalmic findings include nonarteritic or arteritic ischemic optic neuropathy (NAION, AION), optic neuritis, extraocular motility disturbance that may be part of cranial nerve palsies, and infarctions in the central nervous system along the visual pathway.10
This case highlighted the rapid progress of ocular disease in patients with SLE and APS, and the importance of clinical vigilance for this condition. The patient’s ocular manifestations indicated that SLE was highly active, which was also reflected by a SLE disease activity index of 27, and the cardiac, central nervous system, renal involvement. Neovascular glaucoma in the right eye occurred shortly after her admission, and her visual function declines sharply. FFA revealed large nonperfusion area in the peripheral retina, which may be caused by platelet and plasma fibrinogen aggregated in retinal capillary due to APS. Prompt diagnosis and treatment are crucial for optimal outcomes. For this case, after the diagnosis was confirmed, corticosteroids, immunosuppressants and anticoagulants were administered. Pan-retinal photocoagulation was applied in both eyes, combining with intravitreal injection of anti-vascular endothelial growth factor drugs in the right eye. These therapies successfully controlled her underlying diseases, and finally protected the patient’s visual function.
In conclusion, APS should be considered in all cases of retinal arterial and venous thrombosis, as well as in cases of unexplained ocular inflammations, particularly in young women. Improving ophthalmologists’ knowledge of SLE and APS is important to avoid misdiagnosis and mistreatment, which can improve the prognosis by timely diagnosis.
REFERENCES
1. Pushker N, Bajaj MS, Chandra M, et al. Ocular and orbital cysticercosis. Acta Ophthalmol Scand 2001; 79:408-13.
2. Kaliaperumal S, Rao VA, Parija SC. Cysticercosis of the eye in South India—a case series. Indian J Med Microbiol 2005; 23:227-30.
3. Sharma T, Sinha S, Shah N, et al. Intraocular cysticercosis: Clinical characteristics and visual outcome after vitreoretinal surgery. Ophthalmology 2003; 110: 996-1004.
4. Garcia HH, Del Brutto OH, Nash TE, et al. New concepts in the diagnosis and management of neurocysticercosis (Taenia solium). Am J Trop Med Hyg 2005; 72:3-9.
5. Del Brutto OH. Neurocysticercosis: A review. Sci World J 2012; 2012:159821.
6. Ushiyama O, Ushiyama K, Koarada S, et al. Retinal disease in patients with systemic lupus erythematosus. Ann Rheum Dis 2000; 59:705-8.
7. Montehermoso A, Cervera R, Font J, et al. Association of antiphospholipid antibodies with retinal vascular disease in systemic lupus erythematosus. Semin Arthritis Rheum 1999; 28:326-32.
8. Hall S, Buettner H, Luthra HS. Occlusive retinal vascular disease in systemic lupus erythematosus. J Rheumatol 1984; 11:846-50.
9. Au A, O'Day J. Review of severe vaso-occlusive retinopathy in systemic lupus erythematosus and the antiphospholipid syndrome: Associations, visual outcomes, complications and treatment. Clin Experiment Ophthalmol 2004; 32:87-100.
10. Utz VM, Tang J. Ocular manifestations of the antiphospholipid syndrome. Br J Ophthalmol 2011; 95:454-9.
for publication July 25, 2014.
E-mail: d_fangtian@sina.com
 Chinese Medical Sciences Journal2015年1期
Chinese Medical Sciences Journal2015年1期
- Chinese Medical Sciences Journal的其它文章
- INSTRUCTIONS FOR AUTHORS
- Conjunctival Langerhans Cell Histiocytosis: a Case Report
- Calyceal Diverticulum Mimicking Simple Parapelvic Cyst: a Case Report
- Effects of Sunitinib Malate on Growth of Human Bladder Transitional Cell Line T24 In Vitro△
- Association between Two Polymorphisms of Follicle Stimulating Hormone Receptor Gene and Susceptibility to Polycystic Ovary Syndrome: a Meta-analysis
- Total Glycosides of Ranunculus Japonius Prevent Hypertrophy in Cardiomyocytes via Alleviating Chronic Ca2+Overload
