Depressive symptoms among the visually disabled in Wuhan:an epidemiological survey
Wenxue LI, Baoliang ZHONG*, Xiujun LIU, Xian’e HUANG, Xiaoyan DAI, Qiongfang HU, Huishi ZHANG,Hanming XU
•Original article•
Depressive symptoms among the visually disabled in Wuhan:an epidemiological survey
Wenxue LI, Baoliang ZHONG*, Xiujun LIU, Xian’e HUANG, Xiaoyan DAI, Qiongfang HU, Huishi ZHANG,Hanming XU
1. Introduction
Visual disability is defined as either a significant loss of vision in both eyes that cannot be corrected or a visual field defect so extensive that it impairs an individual’s daily life and social function.[1]In 2008, 1.29% of the Chinese population was visually disabled.[2]Among those 50 years of age or older, 10.8% were classified as‘visually impaired’ and 2.3% were classified as ‘blind’.[3]The public health importance of visual disabilities is widely recognized by community members and by government agencies in China, but there is little appreciation of the mental health effects of this severe disability. Negative societal attitudes about the disabled often magnify the limitations imposed by serious sensory and physical disabilities, undermining the self-confidence and psychological wellbeing of disabled individuals.[4,5]Studies from other countries report that the prevalence of depressive symptoms is two- to five-fold higher among individuals with visual disabilities than in the general population.[6,7]Previous studies in China, including two studies of students in special schools for the blind[8,9]and one study in blind community members,[10]also found that people with visual disabilities report lower self-esteem and higher levels of depressive symptoms compared to the general population. But these studies were conducted in small,unrepresentative samples and they did not consider the demographic and personality factors associated with depression in visually disabled individuals. The current study assessed the prevalence of depressive symptoms and the factors associated with depressive symptoms in a representative sample of all visually disabled individuals registered with the Disabled Persons’Federation in Wuhan, a municipality of ten million residents[11]in China’s central Hubei Province.
2. Methods
2.1 Pilot study
A pilot study was conducted with 50 visually disabled participants to assess the feasibility of the intended survey procedures and to make a crude assessment of the prevalence of ‘severe depressive symptoms’ (i.e.a score of 27 or higher on the Chinese version of the Center for Epidemiological Studies Depression Scale[CES-D][12-14]) which would subsequently be used to estimate the required sample size in the main study.
2.2 Sampling
PASS software 2005 (LLC, Kaysville, UT, USA) was used to estimate the sample size needed for the main study. The formula for finite population sampling was used with the following parameters: (a) based on the pilot survey,the estimated possibility of detecting severe depressive symptoms in this population was set as 0.1; (b) precision was set as 0.02; (c) typeierror (alpha) was set as 0.05;(d) the registered visually disabled population in Wuhan was 22,184; (e) respondent rate was set as 0.8; (f) the design effect was set as 1.1. This generated a required sample size of 1142.
The identification of participants in this survey is shown in Figure 1. Based on the national prevalence of visual disabilities of 1.29%[2]and Wuhan’s population of 10 million individuals,[11]there are an estimated 129,000 visually disabled residents in the municipality. In China most individuals with serious disabilities who require government financial assistance or other types of services are registered with the local Disabled Persons’Federation, a semi-governmental agency with offices throughout the country that coordinate governmental and non-governmental services for disabled citizens and their families. The sampling frame for the study was all 22,184 persons with visual disabilities listed in the registry maintained by the Wuhan Disabled Persons’Federation (WDPF) as of 1 July 2011. (This registry includes approximately 17% of all persons with visualdisabilities living in Wuhan.) After excluding individuals with multiple disabilities and those under 18 years of age, multi-stage cluster random sampling was used to identify the sample. Given that 66% of the population and 60% of all registered persons with visual disabilities live in the central districts of the municipality, we randomly selected three of the seven central districts(Jiangan, Jianghan and Qiaokou) and one of the six suburban districts (Xinzhou). In the second stage of sampling, the urban neighborhoods and rural villages in each district were listed by population size and then every fourth neighborhood of the 468 urban neighborhoods was selected and every sixth village of the 579 rural villages was selected. This resulted in 157 urban neighborhoods and 115 rural villages, but 12 of the urban neighborhoods and 11 of the rural villages selected had no registered individuals with a visual disability. All 1200 registered individuals 18 years of age or older with visual disabilities (and no other disability)in the remaining 144 urban neighborhoods and 104 rural villages were potential subjects for the study.Among these identified subjects, 1003 (83.6%) were located and successfully completed the survey.
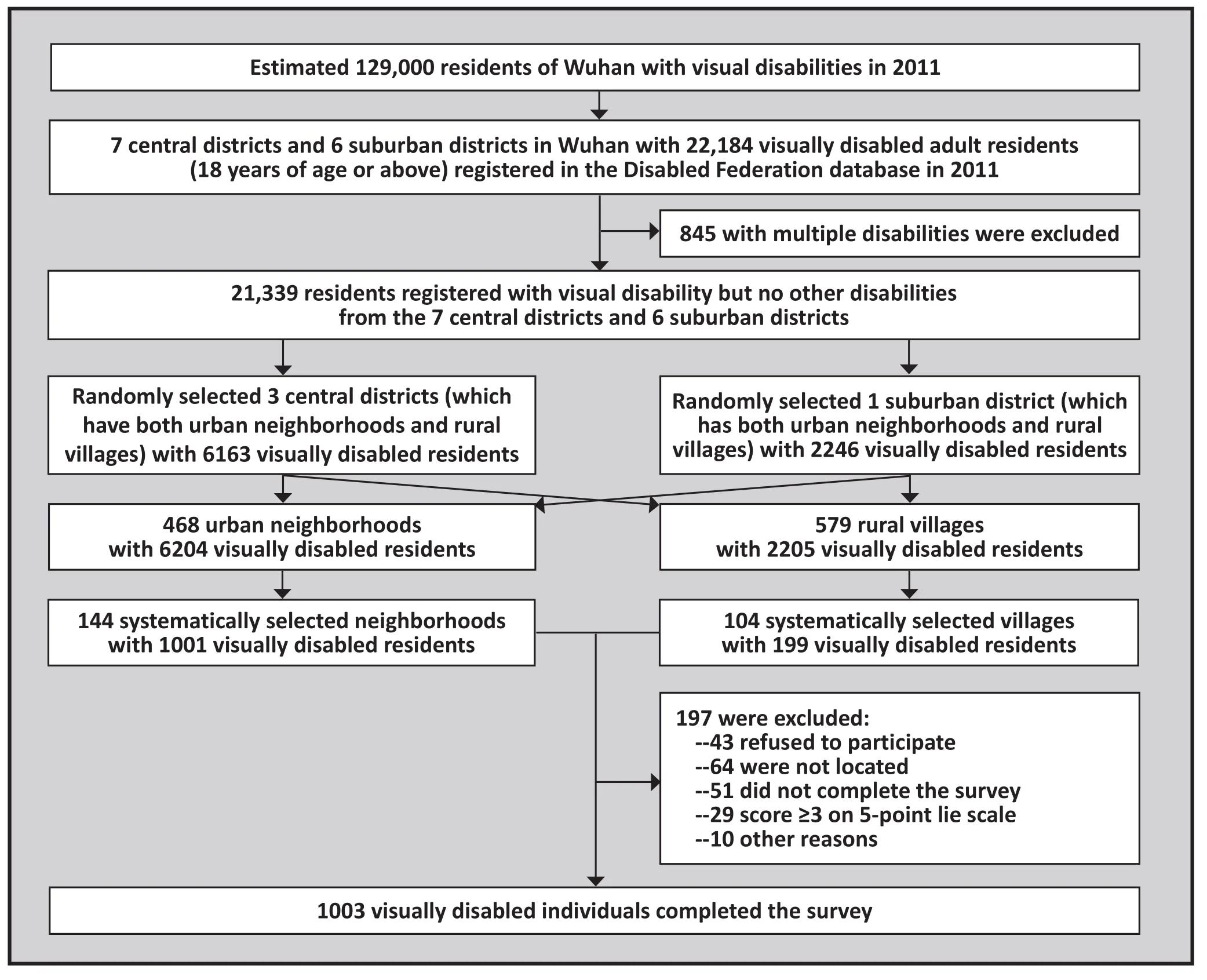
Figure 1. Identification of the survey participants
2.3 Assessments
The survey instrument employed in the current study consists of three parts: a questionnaire developed for the study that collects basic demographic information(age, gender, education, marital status, urban v. rural residence, registered degree of disability, family income,and self-reported presence of religious beliefs); the Chinese version of the Center for Epidemiological Studies Depression Scale (CES-D);[12-14]and the Revised Eysenck Personality Questionnaire-Short Scale for Chinese (EPQ-RSC).[15]
The CES-D is a 20-item scale used to assess the frequency of depressive symptoms during the past week.Each items is rated on a 4-point Likert scale (0=‘rarely or none of the time [less than 1 day]’; 1=‘some or a little of the time [1-2 days]’; 2=‘occasionally or a moderate amount of the time [3-4 days]’; and 3=‘most or all of the time [5-7 days]’). The total score ranges from 0 to 60 with higher scores representing more frequent depressive symptoms. The total score is classified as ‘no significant depressive symptoms’ (total score=0-15), ‘mild depressive symptoms’ (total score=16-19), ‘moderate depressive symptoms’ (total score=20-26), and ‘severe depressive symptoms’ (total score>26). The Chinese version of CES-D has good reliability and validity, with a reported Cronbach α of 0.88.[14]
The EPQ-RSC is a 48-item scale with dichotomous(‘yes’ or ‘no’) response sets. There are four subscales:an extraversion/introversion scale (lower scores indicate more introversion), a neuroticism/stability scale(higher scores indicate greater emotional instability),a psychoticism/socialization scale (higher scores indicate being more reclusive, indifferent to others,and intransigent), and a lie scale. Only the first three personality traits were included in this analysis. The lie scale, which was used to assess the acceptability of respondents’ answers, included three questions from the original EPQ-RSC and two new items that we previously developed for use with heroin users:[16]the original items were (a) ‘Are all of your habits good and desirable ones?’, (b) ‘Have you ever blamed someone else for doing something you knew was really your own fault?’, and (c) ‘Have you ever taken anything (even a pin or button) that belonged to someone else?’; the two added items were (d) ‘I’m worried becauseihave too much money to spend it all,’ and (e) ‘ I’m not afraid of anything’. Responding ‘yes’ to items (a), (d), and (e) and responding ‘no’ to items (b) and (c) were considered untruthful; the survey results of individuals who had three or more untruthful responses were excluded.
2.4 Survey methods
The three survey instruments were administered in face-to-face interviews conducted in respondents’homes from 1 July to 28 December 2011. Before starting the survey interviewers explained the aims and the confidentiality principles of the study and obtained written informed consent from the participant. The interviewers read all the items to the participants and recorded their answers. When the respondent had difficulty understanding an item, interviewers provided a brief explanation.
Interviewers were 63 staff members (40 men and 23 women) from the local community service office in each neighborhood. They had all been recommended and trained through the WDPF. Ten volunteers with visual disabilities were recruited to participate in the training sessions for the interviewers. During the training sessions the inter-rater reliability of the interviewers of the overall CES-D score (intraclass correlation coefficient[ICC]=0.95) and of the three EPQ-RSC subscale scores(ICC=0.955-0.963) were excellent. During the main study, the interviewers in each selected neighborhood or village were supervised by an official from the WDPF who cross-checked all of the questionnaires and randomly phoned some of respondents to inquire about their impressions of the interview. Interviewers who failed to follow the survey protocol were identified and closely supervised.
The study was approved by the institutional review board of the Wuhan Mental Health Center.
2.5 Statistical methods
SPSS software version 19.0 was used to analyze the data.Most of the continuous variables were dichotomized at the median value, including years of schooling, duration of disability and scores of the three subscales of EPQRSC. Age was divided into three ranges in the analysis.The four levels of visual disability recognized by the WDPF were categorized as ‘blind’ (level 1 and level 2) or‘visually impaired’ (level 3 and level 4). The prevalence of depressive symptoms in different population cohorts was calculated and an overall adjusted rate was computed by adjusting the crude rate for differences between the gender ratio in the sample compared to that in all 22,000 visually disabled persons registered with the WDPF. Ordinal multivariate logistic regression models with a backward stepwise entry of variables were used to estimate the association between the severity of depressive symptoms, the level of visual disability and personality variables. All tests employed were two-tailed and the significance level used was p<0.05.
3. Results
3.1 Characteristics of survey participants
The demographic and other characteristics of the respondents are shown in Table 1. Among the 1003 respondents, 592 (59.0%) were male and 411 (41.0%)were female. The mean (sd) age was 46.7 (12.7) years,ranging from 18 to 99. Among these respondents,218 (21.7%) had a level-1 visual disability (the most severe form), 181 (18.0%) had a level-2 visual disability,188 (18.7%) had a level-3 visual disability, and 416(41.5%) had a level-4 visual disability (the least severelydisabled). Thus 399 (39.8%) were classified as ‘blind’(i.e., levels 1 and 2) and 604 (60.2%) were classified as‘visually impaired’ (i.e., levels 3 and 4). Distributions of other demographic variables and of the three EPQ-RSC subscale scores are shown in Table 1. All 22,184 visually disabled individuals registered with the WDPF included 49.3% males and their average age was 47.3 years;the proportion of males in our sample was higher(χ2=36.2, p<0.001), but the mean age was similar (t=1.5,p=0.135).

Table 1. Univariate ordinal logistic regression of the severity of depressive symptoms by different characteristics in 1003 visually disabled respondents in Wuhan in 2011
3.2 Prevalence and adjusted prevalence of depressive symptoms
Based on the CES-D scores, 594 respondents (59.2%, 95%confidence interval [CI]=56.2-62.3%) had no significant depressive symptoms, 90 (9.0%, CI=5.9-12.0%) had mild depressive symptoms, 160 (16.3%, CI=13.0-18.8%)had moderate depressive symptoms and 159 (15.9%,CI=13.6-18.1%) had severe depressive symptoms. The gender-standardized prevalences of these four categories of depressive symptoms (standardized to the gender distribution of all visually disabled individuals registered in Wuhan) were 59.6% (CI=56.4-62.7%), 8.8% (CI=5.7-11.8%), 15.6% (CI=12.8-18.5%) and 16.0% (CI=13.7-18.3%), respectively. The proportions of participants with various characteristics stratified according to the four severity levels of depressive symptoms (i.e., none, mild,moderate, and severe) are shown in Table 1.
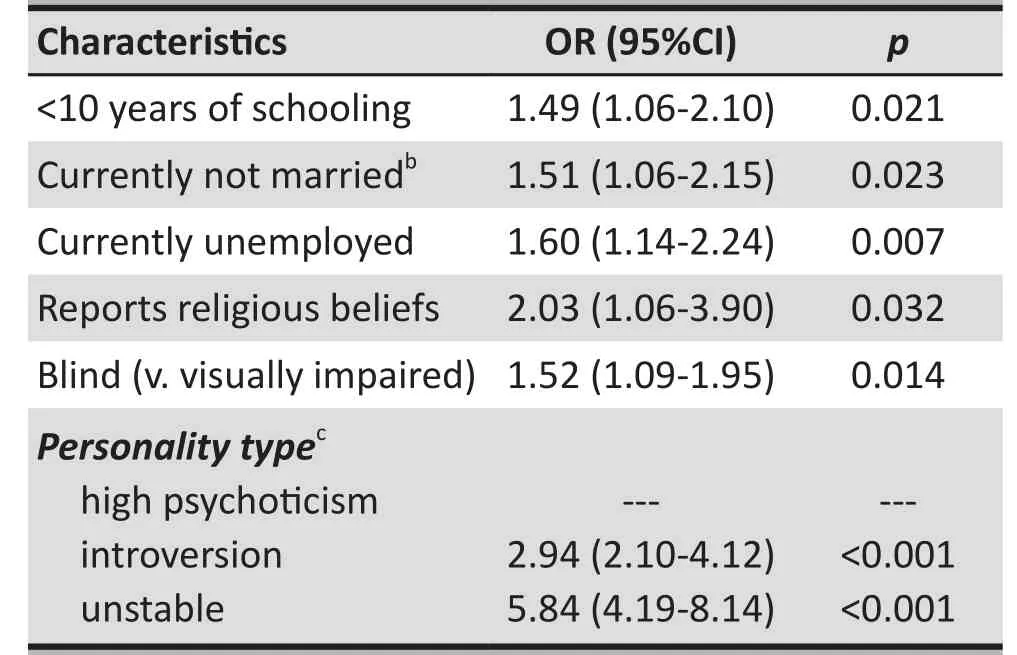
Table 2. Multivariate ordinal logistic regression results of factors significantly associated with the severity of depressive symptoms in 1003 visually disabled respondents in Wuhan in 2011a
3.3 Factors associated with the severity of depressive symptoms among people with visual disability
The results of the univariate ordinal logistic regression analysis are also shown in Table 1. Several variables were significantly associated with the severity of depressive symptoms in these visually disabled individuals:advanced age, lower education, being unmarried or unemployed, having religious beliefs, being classified as blind (i.e., the most severe form of visual disability),living in rural areas, reporting low family income, and having high scores for psychoticism, introversion or neuroticism on the EPQ-RSC.
Results of the stepwise multivariate ordinal logistic regression are shown in Table 2. After entering all statistically significant variables from the univariate analysis (Table 1), factors that were independently associated with the severity of depressive symptoms were identified using backward selection. The factors that remained in the final model included: low education, being currently unmarried or unemployed,reporting religious beliefs, being classified as blind, and having high scores on the introversion or neuroticism dimensions of the EPQ-RSC. Taken together, these factors accounted for 29.3% of the variance in the severity of depression among these subjects.
4. Discussion
4.1 Main findings
In this study, the estimated prevalence of having any depressive symptom (CES-D >16) was 40.8% among people with visual disabilities. This prevalence is much higher than that reported in other cohorts in China,including the 19.9% prevalence reported in the general urban population,[17]the 23.7% prevalence reported among rural-to-urban migrants,[18]the 24.8% prevalence reported in perimenopausal women,[19]and the 33.8% prevalence reported in outpatients with heroin dependence.[20]The prevalence we found in persons with visual disabilities is similar to that reported among older individuals with Parkinson’s Disease (38.8%)[21]and among elderly patients in general hospitals (39.0%).[22]Compared to 1467 individuals with physical disabilities in Wuhan, persons with visual disabilities were more likely (at a trend level only) to have mild, moderate or severe depressive symptoms (9.0% v. 7.7%, 16.3% v.15.2%, 15.9% v. 14.0%, respectively, Mann-Whitney Z=1.89, p=0.059).[23]However, the severity of depressive symptoms in individuals with visual disabilities was not significantly different from that reported among 485 individuals in Wuhan with hearing disabilities[24](Z=0.90,p=0.370).
The high prevalence of depressive symptoms in persons with visual disabilities found in this study is concordant with findings reported in other studies. In other countries, a high prevalence of depression has been reported among blind adolescents[25]and among elders with visual impairments.[26]In China, a small community based study[10]and two school-based studies[8,27]also found an elevated prevalence of depression among visually disabled individuals.
Regression analysis found that the severity of depressive symptoms among visually disabled individuals is related to education level, marital status, employment status, religious beliefs, degree of visual disability and personality. On the whole, these findings are similar to those reported in previous studies about depression in the general population, which identify female gender,[28,29]low educational level,[30,31]unhappy marriage[29,31]and unemployment[28,29,31]as the primary risk factors for depression. There are, however, some differences.The vast majority of research in other cohorts reports substantially higher rates of depressive symptoms in women than in men, but we found no significant difference in the self-reported severity of depressive symptoms between males and females with visual disabilities.
Having a religious belief is generally viewed as a protective factor against depression in the general population.[32]But in this study the relatively small proportion of respondents who reported having religious beliefs had more severe depressive symptoms than respondents who reported having no religious beliefs. This finding – which suggests that holding religious beliefs is a risk factor for depression – is consistent with some other studies in China among outpatients in internal medicine departments[33]and among individuals with physical disabilities.[34]One possible explanation for this difference with studies from the West is that the majority of mainland Chinese are atheists; individuals who subsequently become religious (typically after becoming an adult) may do so because they are seeking more existential meaning to their life or because they are emotionally troubled.However, the questions used in our survey to identify those with religious beliefs did not assess the degree the individual participated in religious activities so it was only a crude measure of ‘religiousness’. Further studies are needed to clarify the reasons for this apparent cross-cultural difference in the psychological valence of religious beliefs and religious participation.
It is not surprising that the severity of depressive symptoms was more pronounced among individuals classified as ‘blind’ than among those classified as‘visually impaired’, which is a less severe form of visual disability.[34]This relationship between the degree of disability and a higher prevalence of depressive symptoms is also seen in the physically disabled[24]and in the hearing disabled.[25]Some previous studies have reported that blind individuals are more likely to have low self-esteem and to be introverted, emotionally unstable, and unassertive.[10,35]Our study confirmed these findings: there was a clear, independent relationship between the severity of depressive symptoms and high introversion and high neuroticism (i.e., emotional instability). This association has also been reported in the general population; in the general population the EPQ neuroticism score is positively related to depression[36]and the EPQ extraversion score is negatively related to depression.[37]
4.2 Limitations
The main limitation of this study is that the sampling was based on the registration system of the WDPF, a system that only captures an estimated 17% of all visually disabled persons in the community. Persons registered in the government-run WDPF database tend to have lower family incomes and higher degrees of disability, so our reported prevalence of depressive symptoms in the visually disabled may be an overestimate of the rates that exist among all visually disabled individuals in the community. However, individuals registered with the Disabled Persons’ Federation are those whose disability is severe enough to require government assistance so they are an important target group for any subsequent interventions. A second limitation is that this is a crosssectional study so the factors we found associated with depressive symptoms are not, strictly speaking,risk factors. Whether or not the identified factors cause depressive symptoms need to be determined by prospective longitudinal studies. A third limitation is that the current study only measured depressive symptoms,not depression; so it is not known how many of these individuals were sufficiently impaired to justify a clinical diagnosis and medical treatment. A final limitation is that some other risk factors of depression (negative life events, lack of social support, poor coping style,etc.) were not assessed in the study so it is uncertain whether or not these factors would also be associated with increased rates of depressive symptoms in visually disabled individuals.
4.3 Implications
This is the first study in China to provide a reliable estimate of the prevalence of depressive symptoms in visually disabled individuals who are registered with the national Disabled Persons’ Federation. The extremely high reported rates of depressive symptoms – which were similar in males and females – indicate that individuals with visual disabilities have psychological needs that are not being met. Many of the risk factors for depression in the general population are also associated with depressive symptoms in the visually disabled but the negative psychological effect of these factors may be magnified by the visual disability,particularly in individuals who are more severely disabled. Services for the visually disabled (and for individuals with other types of severe disabilities)need to include periodic evaluation of depressive symptoms, expanded social supports that specifically focus on improving psychological wellbeing, and, when necessary, psychiatric assessment and treatment.
Conflict of interest
The authors declare no conflict of interest.
Funding
The study was supported by the Wuhan Bureau of Health (No. WG11D03).
Acknowledgements
The authors thank the Wuhan Disabled Persons’Federation and the Disabled Persons’ Federations of the Jiangan, Jianghan, Qiaokou, and Xinzhou districts of Wuhan for their support of the survey.
1. Leading group of the Second China National Sample Survey on Disability, National Bureau of Statistics of the People’s Republic of China. Data Manual of the Second China National Sample Survey on Disability. Beijing: Huaxia Publishing; 2007. (in Chinese)
2. Zheng XY, Zhang L, Chen G, Pei LJ, Song XM. Prevalence of visual, hearing, speech, physical, intellectual and mental disabilities in China. Chinese Journal of Epidemiology 2008;29(7): 634-638. (in Chinese)
3. Zhao J, Ellwein LB, Cui H, Ge J, Guan H, Lv J, et al. Prevalence of vision impairment in older adults in rural China: the China Nine-Province Survey. Ophthalmology 2010; 117(3): 409-416.
4. Sharma S. Emotional stability of visually disabled in relation to their study habits. J Indian Acad Appl Psychol 2006; 32(1):30-32.
5. Nadeem NA, Pujuand JA, Zahoor N. Study of mental health of visually impaired and hearing impaired rural and urban adolescent students. Stand J Edu Res Essay 2013; 1(1): 21-24.
6. Margrain TH, Nollett C, Shearn J, Stanford M, Edwards RT,Ryan B, et al. The depression in visual impairment trial(DEPVIT): trial design and protocol. BMC Psychiatry 2012;12(1): 57-64.
7. Noran NH, Izzuna MG, Bulgiba AM, Mimiwati Z, Ayu SM.Severity of visual impairment and depression among elderly Malaysians. Asia Pac J Public Health 2009; 21(1): 43-50.
8. Li X, Zhao J, Lin YY. Comparative study of the psychological health of blind school students and general middle school students.. Journal of Jining University 2012; 33(4): 121-124.(in Chinese)
9. Liao SS, Ye GJ. A psychological health survey among 237 students from special blind schools. Chinese Mental Health Journal 1989; 3(6): 245-247. (in Chinese)
10. Li CL, Zhao ZQ. Psychological characteristics of blind persons in Yinchuan, Ningxia. Ningxia Medical Journal 2010; 32(5):474-475. (in Chinese)
11. Wuhan Bureau of Statistics. Wuhan Statistical Yearbook 2012. Beijing: National Statistics Press of China. 2012.
12. Zhang J, Wu ZY, Fang G, Li J, Han BX, Chen ZY. Development of the Chinese age norms of the Center for Epidemiological Studies Depression Scale (CES-D) in urban area. Chinese Mental Health Journal 2010; 24(2): 139-143. (in Chinese)
13. Han M, Jia CX. Reliability and validity of the Center for Epidemiological Studies Depression Scale (CES-D) in different rural populations. Chinese Journal of Public Health 2012;28(10): 1265-1267. (in Chinese)
14. Zhang ZJ. Handbook of Behavioral Medical Scales. Beijing:Chinese Medical Multimedia Press; 2005. p. 224-225. (in Chinese)
15. Qian MY, Wu GC, Zhu RC, Zhang S. Development of the Revised Eysenck Personality Questionnaire Short Scale for Chinese (EPQ-RSC). Acta Psychologica Sinica 2000; 32(3):317-323. (in Chinese)
16. Liu XJ, Zhong BL, Zhu JH. Tobacco use behavior and depression, anxiety, and sleep quality among smokers of methadone maintenance treatment outpatients. Chin J Drug Depend 2013; 22(1): 17-22.
17. Xiao L, Ji JL, Zhang SB, Wang WL, Wu Y, Cheng MY, et al.A pilot survey of depressive symptoms and depression in a community of Shanghai. Chinese Journal of Behavioral Medical Science 2000; 9(3): 200-201. (in Chinese)
18. Qiu PY, Yang Y, Chen Q, Yuan P, Zhou HY, et al. Depression and its impact factors among migrant workers in Chengdu.Modern Preventive Medicine 2010; 37(22): 4263-4266. (in Chinese)
19. Gu L, Du L, Shi H, Qian XM, Tan J, Qin M, et al. Investigation on the effect factors of depression symptoms among perimenopausal women. Chinese Journal of Maternal and Child Health Care 2011; 26(25): 3962-3966. (in Chinese)
20. Zhong BL, Li HJ, Zhu JH, Chen HH. Depression, anxiety,and insomnia among methadone maintenance treatment outpatients: detection rates, comorbidity and correlates.Chinese Journal of Drug Dependence 2010; 19(5): 371-375.(in Chinese)
21. Ma JH, Zou HQ, Sun F, An J, Chen B. Impact of depression on quality of life of Parkinson’s disease and its associated factors. Journal of capital Medical University 2011; 32(6):776-780. (in Chinese)
22. Lu Z, Wu WY, Cai J, Li YS, Li CB, Liu ML, et al. Depression of elderly patients in general hospitals. Chinese Mental Health Journal 2002; 16(7): 468-470. (in Chinese)
23. Li WX, Zhong BL, Liu XJ, Huang XE, Zhang HS. Depressive symptoms in physically disabled persons in Wuhan: A crosssectional study. Chinese Mental Health Journal 2012; 26(12):943-948. (in Chinese)
24. Liu XJ, Zhong BL, Li WX, Xu HM, Huang XE, Zhang HS, et al.Prevalence and influencing factors of depressive symptoms in persons with hearing disability in Wuhan. Chinese Journal of Public Health 2013; 29(5): 1-4. (in Chinese)
25. Koenes SG, Karshmer JF. Depression: a comparison study between blind and sighted adolescents. Issues Ment Health Nurs 2000; 21(3): 269-279.
26. Hayman KJ, Kerse NM, La Grow SJ, Wouldes T, Robertson MC, Campbell AJ. Depression in older people: visual impairment and subjective ratings of health. Optom Vis Sci 2007; 84(11): 1024-1030.
27. Huang BF. An investigation on students’ mental status of Zhejiang school for the blind. Chinese Journal of Special Education 2004; 45(3): 39-42. (in Chinese)
28. Cui LJ, Li KQ, Jiang QP, Cui Z, Gao LH, Zhang Y, et al. The prevalence of major depression disorders in Hebei Province from 2004 to 2005. Chinese Journal of Psychiatry 2007;40(3): 140-143. (in Chinese)
29. Wilhelm K, Mitchell P, Slade T, Brownhill S, Andrews G.Prevalence and correlates of DSM-IV major depression in an Australian national survey. J Affect Disord 2003; 75(2): 155-162.
30. Ma X, Xiang YT, Cai ZJ, Li SR, Xiang YQ, Guo HL, et al.Prevalence and socio-demographic correlates of major depressive episode in rural and urban areas of Beijing, China.J Affect Disord 2009; 115(3): 323-330.
31. Lu J, Ruan Y, Huang Y, Yao J, Dang W, Gao C. Major depression in Kunming: prevalence, correlates and co-morbidity in a south-western city of China. J Affect Disord 2008; 111(2-3):221-226.
32. Peng F, Zhang XY. Review on the relationship between religion and mental health. Medicine and Philosophy(Humanistic and Social Medicine Edition) 2010; 31(10): 53-55. (in Chinese)
33. Qin X, Wang W, Jin Q, Ai L, Li Y, Dong G, et al. Prevalence and rates of recognition of depressive disorders in internal medicine outpatient departments of 23 general hospitals in Shenyang, China. J Affect Disord 2008; 110(1-2): 46-54.
34. Brown RL, Barrett AE. Visual impairment and quality of life among older adults: an examination of explanations for the relationship. J Gerontol B Psychol Sci Soc Sci 2011; 66(3):364-373.
35. Chen TY, Liu YH. Investigation on psychological guidance in Beijing school for the blind. Chinese Journal of Special Education 1998; 19(3): 10-13. (in Chinese)
36. Wu JX, Lv QQ. Relationship among anxiety, depression,personality and self-efficacy of freshmen in medical colleges.China Journal of Health Psychology 2009; 17(12): 1498-1501.(in Chinese)
37. Wang J, Zhang HB, Wang LN, Hu HL, Zhu JL, Wu HH, et al.Correlation between depression and personality, and family environment among college students in Anhui Province.Chinese Journal of School Health 2009; 30(1): 32-33. (in Chinese)
武汉地区视力残疾人群的抑郁症状:一项流行病学调查
李文学,钟宝亮*,刘修军,黄先娥,戴晓燕,胡琼芳,张惠实,徐汉明
华中科技大学同济医学院附属精神卫生中心 湖北武汉
背景:在中国目前还缺乏针对残疾人的心理健康状况的代表性研究。目的在中国武汉具有代表性的严重视觉障碍的人群中,评估抑郁症状的发生率及其相关因素。方法采用多阶段分层整群抽样方法,从武汉市残疾人联合会注册的22000名严重视力残疾的人群中抽取1200例。训练有素的调查员使用流行病学研究中心抑郁量表(CES-D)及修订版艾森克人格问卷简式量表(EPQ-RSC)中文版对样本人群进行评估。结果成功完成调查的1003个人中轻度,中度和重度抑郁症状的校正患病率分别为8.8% (95%CI =5.7-11.8%),15.6% (95%CI=12.8-18.5%)和16.0% (95%CI=13.7-18.3%)。多因素逻辑回归分析显示,与严重抑郁症状显著相关的因素有(按重要性顺序)情绪不稳定(OR= 5.84,CI=4.19-8.14),内向性格(OR=2.94,CI=2.10-4.12),有宗教信仰(OR= 2.03,CI=1.06-3.90),失明(相对于那些仅有视力受损) (OR=1.52,CI=1.09-1.95),未婚(OR= 1.51,CI=1.06-2.15) ,以及文化程度低(OR= 1.49,CI=1.06-2.10)。结论武汉残联注册的所有视碍人员有超过三分之一存在显著临床意义的抑郁症状。这些人几乎没有接受治疗。针对有严重视觉障碍患者的服务,也包括对其他严重的身体或感官残疾患者的服务,应包括开展改善心理健康的活动,定期筛查心理问题,以及必要时对精神障碍进行专业的治疗。
Background:There are no representative studies on the mental health status of persons with disabilities in China.Aim:Estimate the prevalence of depressive symptoms and identify the factors associated with depressive symptoms in a representative sample of individuals with serious visually disabilities in Wuhan, China.Methods:A multi-stage stratified cluster sampling method was used to identify 1200 visually disabled individuals from among the 22,000 persons with serious visual disabilities who were registered with the Wuhan Disabled Persons’ Federation. Identified individuals were administered the Center for Epidemiological Studies Depression Scale (CES-D) and the Revised Eysenck Personality Questionnaire-Short Scale for Chinese (EPQ-RSC)by trained interviewers.Results:The adjusted prevalence of mild, moderate and severe depressive symptoms among the 1003 individuals who successfully completed the survey were 8.8% (95% confidence interval [CI]=5.7-11.8%), 15.6%(CI=12.8-18.5%) and 16.0% (CI=13.7-18.3%), respectively. Factors significantly associated with more severe depressive symptoms in the multivariate logistic regression analysis (in order of importance) were emotional instability (OR=5.84, CI=4.19-8.14), introverted personality (OR=2.94, CI=2.10-4.12), having religious beliefs(OR=2.03, CI=1.06-3.90), being blind (versus those who were only visually impaired) (OR=1.52, CI=1.09-1.95),being unmarried (OR=1.51, CI=1.06-2.15), and having less than 10 years of formal education (OR=1.49, CI=1.06-2.10).Conclusions:Over one-third of all individuals with visual disabilities registered with the Disabled Persons’Federation in Wuhan have clinically significant depressive symptoms. Therefore, services for persons with serious visual disabilities – and for individuals with other types of serious physical or sensory disabilities –should include activities aimed at improving psychological wellbeing, periodic screening for psychological problems and, when needed, professional treatment for mental disorders.
10.3969/j.issn.1002-0829.2013.05.006
Affiliated Mental Health Center, Tongji Medical College of Huazhong University of Science & Technology, Wuhan, China
*correspondence: zbl_201@163.com
(received: 2013-05-17; accepted:2013-07-30)

Wenxue Li obtained his associate degree in clinical medicine (1982) from the Hubei School of Medicine in Huanggang, Hubei Province. He has been working in the Mental Health Center of Tongji Medical College at the Huazhong University of Science and Technology since May 1985. He is currently a senior psychiatrist and the vice- director of the Public Health Department of the Mental Health Center. His research interests are community prevention and management of mental disorders and mental health in special communities.
*通讯作者:zbl_201@163.com
——勉冲·罗布斯达
- 上海精神医学的其它文章
- From pilot studies to confirmatory studies
- Case report of adjunctive use of olanzapine with an antidepressant to treat sleep paralysis
- rTMS in the management of auditory hallucinations in patients with schizophrenia
- The multifaceted question of the prescription of antidepressants during pregnancy
- Use of antidepressants during pregnancy: a better choice for some
- Using the Montreal Cognitive Assessment Scale to screen for dementia in Chinese patients with Parkinson’s disease