Memory and behavior-related problems of patients with neurocognitive disorders and the attitudes of their caregivers
Qingyan Wang, Fen Jiang, Sanmei Chen, Siyuan Tang
Memory and behavior-related problems of patients with neurocognitive disorders and the attitudes of their caregivers
Qingyan Wang1, Fen Jiang2, Sanmei Chen1, Siyuan Tang1
Objective:The purpose of this study was to investigate the memory and behavior-related problems of patients with neurocognitive disorders and the attitudes of their caregivers so as to provide an effective basis for nursing interventions against such problems.
Methods:The subjects were selected from patients who were under treatment or short-term hospitalization between April 2011 and March 2012. One hundred fifty-three patients with neurocognitive disorders and their major caregivers were selected from 9 grade 3 Class A hospitals of Hunan Province. The Revised Memory and Behavior Problems Checklist (RMBPC) was used to measure the memory and behavior-related problems of patients with neurocognitive disorders and the influence on their caregivers. The occurrence of different memory and behavior-related problems and the distress on their caregivers was compared.
Results:The RMBPC investigation showed that among 153 patients and their caregivers, 152 (99.3%) had memory-related problems, 137 (89.5%) had depression, and 136 patients (88.9%) had destructive behaviors. The incidence of memory-related problems was higher than depression and destructive behaviors (P<0.01). Caregivers bore more distress when encountering destructive behaviors (1.95±1.13 points) than memory-related problems and depression (0.91±0.76 points and 0.89±0.85 points;P<0.01). Curve fitting was used to analyze the relationship between the number of memory and behavior-related problems and the distress on their caregivers. A curve correlation existed between the two factors (the recorded maximum value of the Cubic equation curve was 0.278, F=229.212,P<0.05).
Conclusion:Among patients with neurocognitive disorders, memory-related problems had the highest incidence, while the caregivers bore the strongest distress when encountering destructive behaviors, thus interventions should be conducted in consideration of patient memory and behavior-related problems, and caregivers’ attitude to further reduce caregiver burden.
Neurocognitive disorders, Memory Disorder, Caregiver, Attitude, Revised Memory and Behavior Problems Checklist
Introduction
Neurocognitive disorders are chronic, progressive, deteriorating mental diseases in old age, generally associated with various memory and behavioral disorders, and affected patients often require long-term care [1]. Currently, the lack of long-term caregiving agencies, the insurance system, and related policies in China cause that traditional family caregiving is still the major form of long-term care for patients with neurocognitive disorders. This undoubtedly brings a huge burden to the caregivers,and seriously influences their physical and mental health [2], and also becomes a key point of community health care. In the 1980s it was shown that memory and behavioral problems of patients with neurocognitive disorders was an important factor regarding the level of burden, depression, stress, and anxiety of the caregivers [3, 4]. The memory and behavioral problems of the patients with neurocognitive disorders are also considerations determining whether or not the senile shall be sent to medical pension institutes [5]. Domestic and foreign research have carried out analyses on the influence of patient behavior on the burden of their caregivers [6–9]; however, no investigation regarding the specific behaviors of patients has been conducted by domestic research. The current research investigated 153 patients with neurocognitive disorders (memory and behavioral problems) and their major caregivers’ attitudes towards each behavior via questionnaire. The memory and behavioral problems of patients with neurocognitive disorders and the maximum intensity of distress amongst the caregivers were determined, and effective evidence-based rationale for nursing interventions against memory and behavioral problems of the patients with neurocognitive disorders and the attitudes of their caregivers was provided.
Subjects and methods
Research subjects
Between April 2011 and March 2012, 153 patients with neurocognitive disorders and their caregivers were selected as research subjects. The patients with neurocognitive disorders were under treatment or short-term hospitalization in nine provincial hospitals in Hunan, including Xiangya Hospital of Central South University, the Second Xiangya Hospital of Central South University, the Third Xiangya Hospital of Central South University, Hunan Provincial People’s Hospital, Hunan Provincial No.4 Hospital, and Brains Hospital of Hunan Province. The subjects were selected according to the following criteria: (1) patients with neurocognitive disorders diagnosed by the neurology consultant room of a Class Three grade A hospital, and conforming to the diagnostic standards of the tenth revision of the international classification of disease (ICD-10) of the World Health Organization and their caregivers; (2) caregivers ≥18 years of age, and caregiving ≥3 months in duration; (3) caregivers shall provide care for the patients for the longest time, undertake most tasks of the caregiving, and have a major role in the patients’ caregiving process, and each patient can only have one caregiver who can be his/her spouse, child, or other relative; and (4) caregivers are lucid and can speak and communicate with the researchers, and are willing to participate in the research study. Caregivers who received remuneration were excluded.
Methods
Research tools:
General data questionnaire.The questionnaire was designed by the researchers. The main content of the questionnaire included 20 items about caregivers, including age, gender, and economic status, and 7 items about the patients with neurocognitive disorders, including age, gender, neurocognitive disorder type, and self-care situation.
Revised Memory and Behavior Problems Checklist (RMBPC) [5].This checklist is formed by revising the original Memory and Behavior Problem Checklist, which has been widely used to measure the memory and behavioral problems of patients with neurocognitive disorders and the influence of the problem towards their caregivers [9–11]. Taiwan scholars have developed a Chinese version with good reliability [12]. In this research, the Cronbach’s α coefficient in the checklist was 0.800. The RMBPC includes two sub-checklists consisting of the memory and behavioral problems of the patients, and their caregivers’ attitudes towards them. There are 24 items in these two checklists, mainly including 3 dimensions of memoryrelated problems, destructive behaviors, and depression. The full score for the sub-checklist of patient’s memory behavioral problem is 24 points; specifically, if a problem occurs on the patient within 1 week, the score is 1; if not, the score is 0. The sub-checklist shall be completed by the caregiver. In the subchecklist of the caregivers’ attitudes, each item can be divided from 0 to 4 according to the intensity of caregiver distress, as follows: 0=not troubled; 1=slightly troubled; 2=moderately troubled; 3=very troubled; 4=extremely troubled; and the full score is 96. The higher the scores are in the sub-checklists, the more significant the memory and behavior-related problems of the patients, and the stronger the intensity of the caregiver distress.
generally, the following two indices are used to reflect the attitude of the caregivers: (1) average attitude score=full score of this dimension or the sub-checklist/total number of items in this dimension or this sub-checklist, including the number of patients’ memory and behavior occurring or not occurring; and (2) distress intensity=full score of this dimension or this sub-checklist/total item number of this dimension or this subchecklist [13]. This paper took the intensity of the caregiver distress as the index to measure the caregivers’ attitudes.
Data collection methods
This research used a questionnaire for investigation of the caregivers. Regarding the elderly caregivers with poor eyesight and a low level of education, they shall answer the questionnaire orally described by the researcher in the form of neutralization and non-suggestion, then the researcher fills in the questionnaire according to the answers of the caregivers. After completing the questionnaire, the researcher shall collect the questionnaire. This research distributed 170 pieces of questionnaires, 160 of which were recovered; excluding 7 non-effective questionnaires, there were 153 effective questionnaires, thus the rate of effective questionnaires was 90.0%.
Statistical methods
SPSS 17.0 statistical software package was used to perform statistical processing of the data. Measuring data shall be indicated by x±s and analyzed by means of analysis of variance. Pair comparisons of different groups used the SNK method. Comparisons of counting data was tested by x2. Curve fitting was used to analyze the correlation between caregiver distress and the frequency of the diseases. Testing criterion was set at an α=0.05.
Results
Basic data of patients with neurocognitive disorders and their caregivers Basic data of patients with neurocognitive disorders:Among 153 patients with neurocognitive disorders, 93 were males (60.8%) and 60 were females (39.2%). The average age of the patients was 77.7±12.8 years. There were 103 patients (67.3%) with Alzheimer’s disease, 43 patients (28.1%) with vascular neurocognitive disorders, and 7 patients (4.6%) with mixed neurocognitive disorders. Patients’ self-care arrangements were as follows: 16 patients (10.5%) could provide basic self-care; 82 patients (53.6%) had partial self-care ability; and 55 patients (35.9%) had no self-care ability.
Basic data of the caregivers:Among 153 caregivers of patients with neurocognitive disorders, 50 were males (32.7%) and 103 were females (67.3%). The average age was 58.5±12.8 years. One hundred forty-two caregivers (92.8%) were married. Thirteen caregivers (8.5%) had a primary school education or less, 46 (30.1%) had a junior high school education, 48 (31.4%) had a high school or secondary technical school education, 25 (16.3%) had a college education, and 21 (13.7%) had a bachelor’s degree or higher. One hundred thirteen caregivers (73.9%) were unemployed, while 40 caregivers (26.1%) were employed. Ninety-five caregivers (62.1%) were living with their patients. eighty-six caregivers (56.2%) were spouses of the patients, 55 caregivers (35.9%) were the children of the patients, and 12 caregivers (7.9%) were the patients’ daughters or sons-in-law. Among the 153 caregivers, 13 (8.5%) had very poor health, 43 (28.1%) had poor health, 71 (46.4%) were generally healthy, 22 (14.4%) were in good health, and 4 caregivers (2.6%) were in very good health, according to self-report.
Occurrence of memory and behavioral problems and the caregivers’ attitudes
Based on the three dimensions of the RMBPC, 152 patients (99.3%) had memory-related problems; the average number of cases under each item was 120 (78.4%). One hundred thirtysix patients (88.9%) had destructive behaviors; the average number of cases under each item were 62 (40.8%). One hundred thirty-seven patients (89.5%) had depression; the average number of cases under each item was 50 (32.5%). According to a comparison of the incidence among the memory-related problems, destructive behaviors, and depression in patients with neurocognitive disorders, the differences were statistically significant (x2=15.311,P<0.01). The incidence of memory-related problem was higher than the destructive behaviors and depression (P<0.01).
Table 1 shows the specific patient number for each problem and the caregivers’ attitudes. Among the patients’ memory and behavioral problems, the following three problems occurredmost frequently: “hard to remember the recent events;” “forget today’s date;” and “repeat questions asked.” In contrast, the following three problems occurred least often: “threaten to harm themselves;” “threaten to harm others;” “sense frustration and no obvious achievements for themselves.” With respect to the caregivers’ attitudes, the following three problems were the most troublesome: “do something potential dangerous to themselves and others;” “destroy property;” and“wake you or others up at night.” In contrast, the following three items were the least troublesome: “forget today’s date;”“seem sadness or sorrow;” and “sense frustration and no obvious achievements for themselves.”

Table 1. Occurrence of memory and behavioral problems of 153 patients with neurocognitive disorders and the attitudes of their caregivers
Comparison of the corresponding caregivers’ attitudes towards different memory and behavioral problems of the patients
A difference was shown to exist between the level of caregiver distress when encountering memory and behavioral problemsof the patients (P<0.05). Indeed, the caregiver distress arising from the patients’ destructive behaviors was higher than memory-related problems or depression (P<0.01, Table 2).

Table 2. Caregivers’ attitudes towards different memory and behavioral problems of 153 patients with neurocognitive disorders
Analysis of the number of patients with problems and caregiver distress
To further explain the relationship between the caregivers’burden and the memory and behavior-related problems of the patients. Curve fitting was used to analyze the relationship between caregiver burden and the memory and behaviorrelated problems of the patients. TheR2value in the Cubic equation curve had a maximum of 0.278 (F=229.212,P<0.05). Additionally, although the linear regression relationship was statistically significant, (R2=0.185), it was a non-optimal fitting curve (Fig. 1).
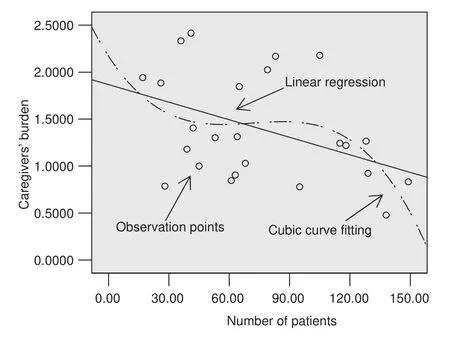
Fig. 1. Fitting diagram of relationship between the intensity of caregiver distress and the case number of patients.
Discussio n
The most common memory and behavior-related problems among the patients with neurocognitive disorders and the most troublesome problems for the caregivers
The RMBPC applied in this research covers three common memory and behavior-related problems for patients with neurocognitive disorders (memory-related problems, destructive behaviors, and depression). This finding is consistent with the research results of Cheng et al. [9]; the top five of the frequently occurring memory and behavior-related problems are all memory-related problems. Among the destructive behaviors for patients with neurocognitive disorders, the most common behavior is that they might “wake you or others up at night.” The most common depression-related problem is that they would “seem like sadness or sorrow.” The five rarest problems were related to destructive behaviors and depression. The rarest problem were related to memory; specifically, patients found it “hard to remember important events.” The problem that troubles the caregivers most is the patients’ destructive behaviors; indeed, the patients would “do something potentially dangerous to themselves or others,” “destroy property,”and “wake up you or others at night.” Additionally, the depression problems that troubles the caregivers most is that they would “threaten to harm themselves,” while with respect to the memory-related problems, what troubles the caregivers most is the patients would always “lose or misplace things.” The five least-troublesome items for the caregivers were memory- and depression-related problems. The least-troublesome destructive behaviors for the caregivers was that the patients would“speak loudly and rapidly.”
The most frequently-observed two of five problems include the following, which are the least-troublesome problems to the caregivers: patients would find it “difficult to remember recent events;” and “forget today’s date.” In contrast, the most-troublesome problems for the caregivers were as follows, which rank sixth and fourth, respectively, from the bottom among the memory and behavior-related problems of the patients: they would “do something potentially dangerous to themselves or others;” and “destroy property.” generally speaking, the higher the incidence of a problem, the more attention it required. The memory and behavior-related problems that cause distress and challenge the caregivers have a high incidence, but are least troublesome to caregivers. This research result is consistent with the findings of Teri [5] and Roth [13]. Those memory and behavior-related problems with a low incidence cause the greatest distress and challenge to caregivers.
Comparison of caregivers’ attitudes towards different memory and behavior-related problems of the patients
Currently, the indices representing the average value of caregivers’ attitudes on the RMBPC include the average value of the attitude and intensity of distress. Based on the formula, the burden could better reflect the actual attitude of the caregivers to each memory and behavior-related problem, while the average value of the attitude would underestimate the burden to the caregivers from each memory and behavior-related problem. In the current study, the burden to the caregivers was used as an index to measure the attitudes of the caregivers. The incidence of memory-related problems of patients with neurocognitive disorders was higher than the destructive behavior and depression, while the destructive behavior created a greater burden for the caregivers than the memoryrelated problems and depression. Regarding problems that already occurred, the memory-related problems and depression occur more frequently, but the effect was small and limited. Such behaviors only affect the patients themselves and their major caregivers. Compared with the preceding behaviors, the incidence of destructive behaviors was low, but would be more harmful and with a wider impact range, even if the threatening act did not cause an injury and may also greatly influence the psychology of the caregivers. Due to the wide influencing range of the destructive behavior, patients’roommates, nursing personnel, and visiting relatives may be affected because patients would “do something embarrassing or awkward,” “something potentially dangerous to themselves or others,” or “wake up you or others at night.”In such cases, caregivers face not only a mental burden, but also external stress.
Analysis of the number of problems and the burden on caregivers with curve fitting was used to explain the relationship between the preceding two factors;R2in the Cubic equation curve was the largest (0.278, F=229.212, P<0.05). There is a possibility that the two factors have a curve relationship, but the relevance was not high, so further research and discussion is needed. Additionally, based on the curve, among the most common and rare patient problems, the burden of the caregivers and the number of problems have a negative correlation. Therefore, for patients with the two aforementioned problems, their caregivers need more attention to relieve their burden by reducing the memory-related problems of the patients or offering short-term alternative care.
Prospect
It has been verified by some research that the caregiving burden may influence the caregivers’ health and cause a higher mortality than the normal population. Moreover, the memory and behavioral problems of the patients were the major source of the caregivers’ burden [9–14]. Thus, community workers can effectively help those people by identifying the memory and behavior-related problems of the patients, and which problem(s) cause maximum trouble for the caregivers [13]. Currently, although China has carried out investigations and interventions [15, 16] with respect to the memory and behavior-related problems of patients, the focus has been limited to the patients’ problems and the caregivers’ attitudes have been neglected. As a result, the intervention measures to reduce the caregivers’ burden are weakened and the problems cannot be solved as a result.
There are many tools that can be used to evaluate patients’mental and behavioral problems, as well as caregivers’ attitudes at the same time; the most widely used tools include the Neuropsychiatric Inventory-Questionnaire (NPI-Q) [17, 18] and the RMBPC [5, 12]. The latter tool was developedby our research institute, and the RMBPC has been recognized by the medical and psychological industry. The tools have been thoroughly used in psychological and sociological investigations. The NPI-Q is mainly used to investigate the caregivers’ general reaction to each patients’ problems. The NPI-Q focuses on the mental and behavioral problems of the patients. Compared with the NPI-Q, RMBPC can more effectively evaluate the caregivers’ attitudes and burden regarding each memory and behaviour-related problem. The level of burden varies with different memory and behavior-related problems of the patients [13]. Further analysis and discussion are needed to determine if RMBPC is more suitable than NPI-Q.
It is believed by the authors that a curve relationship exists between the universality of patients’ memory and behaviorrelated problems and the burden imposed on caregivers. The common behaviors of patients occur more frequently, so more attention should focus on such behaviors, and caregivers are familiar with the behaviors, thus the behaviors are less troublesome to caregivers and vice versa. The influence of destructive behaviors on caregivers cannot be excluded. Thus, the preceding phenomena need further discussion and verification.
In the response process theory, the caregivers’ evaluation of stress was classified into primary and secondary evaluations. The caregivers’ attitude refers to the first reaction when the patients take some actions. The caregivers’ attitude is the result of primary evaluation in the response process theory. The factors that influence the caregivers’ attitude include whether or not there is a caregiver and how the caregiver feels about patients, while other economic factors are the results of the secondary evaluation. The caregivers’evaluation of stress may influence their burden [19]. Future research involving community medical care should focus on finding out which factors influence the primary evaluation to provide a basis for caregivers to reduce their burden and help understand the process underlying the burden imposed on the caregivers.
Confict of interest
The authors declare no conflict of interest.
1. Larson e, Langa K. The rising tide of dementia worldwide. Lancet 2008;372:430–2.
2. Liu Q, Shang S, Yue P. Basing on Lazarus stress – experience and research of the caring of mode home neurocognitive disorders patients’ spouses. Chin gen Pract 2012;15:498–500.
3. Teri L, Borson S, Kiyak HA, Yamagishi M. Behavioral disturbance, cognitive dysfunction, and functional skill. Prevalence and relationship in Alzheimer’s disease. J Am geriatr Soc 1989;37:109–16.
4. Drinka TJ, Smith JC, Drinka PJ. Correlates of depression and burden for informal caregivers of patients in a geriatrics referral clinic. J Am geriatr Soc 1987;35:522–5.
5. Teri L, Truax P, Logsdon R, Uomoto J, Zarit S, Vitaliano PP. Assessment of behavioral problems in dementia: the revised memory and behavior problems checklist. Psychol Aging 1992;7:622–31.
6. Hu F. Investigation and analysis of caregiver burden and influencing factors of the hospitalized patients with Alzheimer’s disease. Chin J Pract Nurs 2012;28:23–4.
7. Yue P, Shang S, Liu Q, Wang ZW, Liu Y, Fu X, et al. Multivariate analysis of the caregivers burden and influencing factors of the home patients with neurocognitive disorders. Chin J Behav Med Sci 2007;16:462–3.
8. Bai J, Ding J, Wang Z. Qualitative research of kinship caregivers experience for patients with neurocognitive disorders. Chin Nurs J 2006;41:1065–9.
9. Cheng ST, Lam LC, Kwok T. Neuropsychiatric symptom clusters of Alzheimer disease in Hong Kong Chinese: correlates with caregiver burden and depression. Am J geriatr Psychiatry 2012;21:1029–37.
10. Assogna F, Palmer K, Pontieri Fe, Pierantozzi M, Stefani A, gianni W, et al. Alexithymia is a non-motor symptom of Parkinson disease. Am J geriatr Psychiatry 2012;20:133–41.
11. Castellanos Pinedo F, Hernández Pérez JM, Zurdo M, Rodríguez Fúnez B, garcía Fernández C, Cueli Rincón B, et al. Psychopathological disorders and quality of life in patients with brain infarction. Neurologia 2012;27:76–82.
12. Fuh JL, Liu CY, Wang SJ, Wang HC, Liu HC. Revised memory and behavior problems checklist in Taiwanese patients with Alzheimer’s disease. Int Psychogeriatr 1999;11:181–9.
13. Roth DL, Burgio LD, gitlin LN, gallagher-Thompson D, Coon DW, Belle SH, et al. Psychometric analysis of the Revised Memory and Behavior Problems Checklist: factor structure of occurrence and reaction ratings. Psychol Aging 2003;18:906–15.
14. Merritt MM, Mccallum TJ, Fritsch T. How much striving is too much? John Henryism active coping predicts worse daily cortisolresponses for African American but not white female dementia family caregivers. Am J geriatr Psychiatry 2011;19:451–60.
15. Li Q, Luo Y, Cai Z, Ai DH, Zhang CJ, Jing XH, et al. Influence of different sports towards the intelligence and behavior of the patients with neurocognitive disorders. Chin J gerontol 2012;32:455–6.
16. Yang Z, Wang H, Yao Z. Quantitative analysis of behavioral and psychological symptoms of the patients with Alzheimer’s disease. Chin J gerontol 2011;31:408–10.
17. Cummings JL. The neuropsychiatric inventory: assessing psychopathology in dementia patients. Neurology 1997;48(5, Suppl 6):S10–6.
18. Cummings JL, Mega M, gray K, Rosenberg-Thompson S, Carusi DA, gornbein J. The neuropsychiatric inventory: comprehensive assessment of psychopathology in dementia. Neurology 1994;44:2308–14.
19. Lazarus FS. Stress, appraisal, and coping. New York: Springer Publishing Company; 1984. pp. 117–8.
1. School of Nursing, Central South University, Hunan 410013, China
2. The Medical College of Hunan Normal University, Hunan 410006, China
Siyuan Tang
School of Nursing, Central South University, Hunan 410013, China e-mail: tangsyuan@126.com
7 October 2013;
Accepted 30 November 2013
 Family Medicine and Community Health2013年4期
Family Medicine and Community Health2013年4期
- Family Medicine and Community Health的其它文章
- The ‘physical-mental’ treatment of cardiovascular disease co-morbid with mental disorders
- Economic burden of inpatients with viral hepatitis B-related diseases and the infuencing factors
- Health-related behaviors in children of ethnic minorities and Han nationality in China
- Epidemiologic survey and analysis of mild cognitive impairment amongst community senior citizens of Changsha City
- Development of community health service-oriented computerassisted information system for diagnosis and treatment of respiratory diseases
- Family Medicine and Community Health
