Differences in the levels of suPeroxide dismutase and brain-derived neurotroPhic factor in first-ePisode schizoPhrenia,chronic schizoPhrenia and normal control subiects
Dachun CHEN,Kebing YANG,Ning WANG,Ying NIE,Meihong XIU,Yanli LI,Qingtao BIAN,Xiangyang ZHANG,Zhanjiang LI
Differences in the levels of suPeroxide dismutase and brain-derived neurotroPhic factor in first-ePisode schizoPhrenia,chronic schizoPhrenia and normal control subiects
Dachun CHEN1,2,Kebing YANG2,Ning WANG2,Ying NIE2,Meihong XIU2,Yanli LI2,Qingtao BIAN2,Xiangyang ZHANG2,Zhanjiang LI1*
Background:Reports about the decreased concentration of brain derived neurotrophic factors(BDNF)and abnormal activity of superoxide dismutase(SOD)in patients with schizophrenia are inconclusive,possibly because of differences in the characteristics of the subjects included in previous studies.
Obiective:Compare in vivo concentrations of SOD and BDNF between patients with first-episode schizophrenia,patients with chronic schizophrenia and normal control subjects;and,in the two patient groups,assess the relationship of SOD and BDNF to the clinical features of the illness.
Methods:Blood concentrations of SOD and BDNF were determined in 78 patients in their first episode of schizophrenia(based on DSM-IV criteria),67 patients with chronic schizophrenia,and 51 normal control subjects.The two patient groups were also administered the Positive and Negative Syndrome Scale(PANSS).
Results:The concentration of both the total superoxide dismutase(T-SOD)and cuprozinc-superoxide dismutase (Cu-ZnSOD)was highest in patients with chronic schizophrenia,intermediate in patients with first-episode schizophrenia and lowest in the normal control group.Conversely,the blood concentration of BDNF was lowest in the chronic schizophrenia group,intermediate in the first-episode schizophrenia group and highest in the normal control group.(All these differences with statistically significant.)BDNF and Cu-ZnSOD were negatively correlated (r=-0.24,P=0.038)in first-episode patients but not in normal controls or chronic patients;BDNF was not significantly correlated to T-SOD in any of the three groups.In drug naïve,first-episode patients there is a significant negative correlation between symptom severity and serum levels of Cu-ZnSOD and a significant positive correlation between symptom severity(primarily positive psychotic symptoms)and BDNF levels but these relationships are absent in chronic patients who are currently medicated.
Conclusion:Compared to patients with first-episode schizophrenia,those with chronic schizophrenia have increased serum activity of SOD and decreased blood concentrations of BDNF.In first-episode patients SOD activity and blood concentrations of BDNF are associated with the symptomatic severity of the illness but this relationship fades in later stages of the illness.
Schizophrenia;Brain-derived neurotrophic factor;Free radicals;Superoxide dismutase;Case-control study
1 Introduction
Previous studies have shown that dopamine can produce free radicals by autologous oxidation or monoamine oxidase metabolism,so enhanced catecholamine metabolism and dopamine hyperactivity—one of the main etiological hypothesis for schizophrenia—may lead to increases in free radicals.Superoxide dismutase(SOD)is the major enzyme organisms employ to prevent oxidative damages from free radicals so increased free radicals secondary to dopamine hyperactivity should induce increased SOD activity[1,2].Several studies have demonstrated that SOD activity is abnormal in patients with schizophrenia,but the results have been contradictory with some authors[3-6]reporting higher SOD activity and others[2,7-9]reporting lower SOD activity.These contradictory results may be due to different characteristics of the samples,suchas duration of illness,severity of symptoms and medication usage.
Blood concentrations of brain derived neurotrophic factors(BDNF)—which plays a key role in neuron growth,differentiation,synaptic linkage,and repair[10]—are lower in patients with schizophrenia than in normal controls[11]and have been correlated with the symptomatic severity of the disorder[12].Increased anti-oxidase activity may lead to degenerative lesions in neurons and associated decreases in protective neurotrophic factors such as BDNF.If this were true,one would expect a negative correlation between serum concentrations of SOD and BDNF in patients with schizophrenia(and,possibly,other mental disorders).We can find no reports in the literature that assess the relationship between these two factors in patients with schizophrenia.
The current study aims to help clarify the relationship of BDNF and SOD in schizophrenia by comparing serum concentrations of these compounds between first-episode patients,chronic patients and normal controls and by identifying the clinical characteristics that are most closely correlated with serum BDNF and SOD concentrations in the two patient groups.
2 Subiects and methods
2.1 Subiects
Subject enrollment is shown in Figure 1.
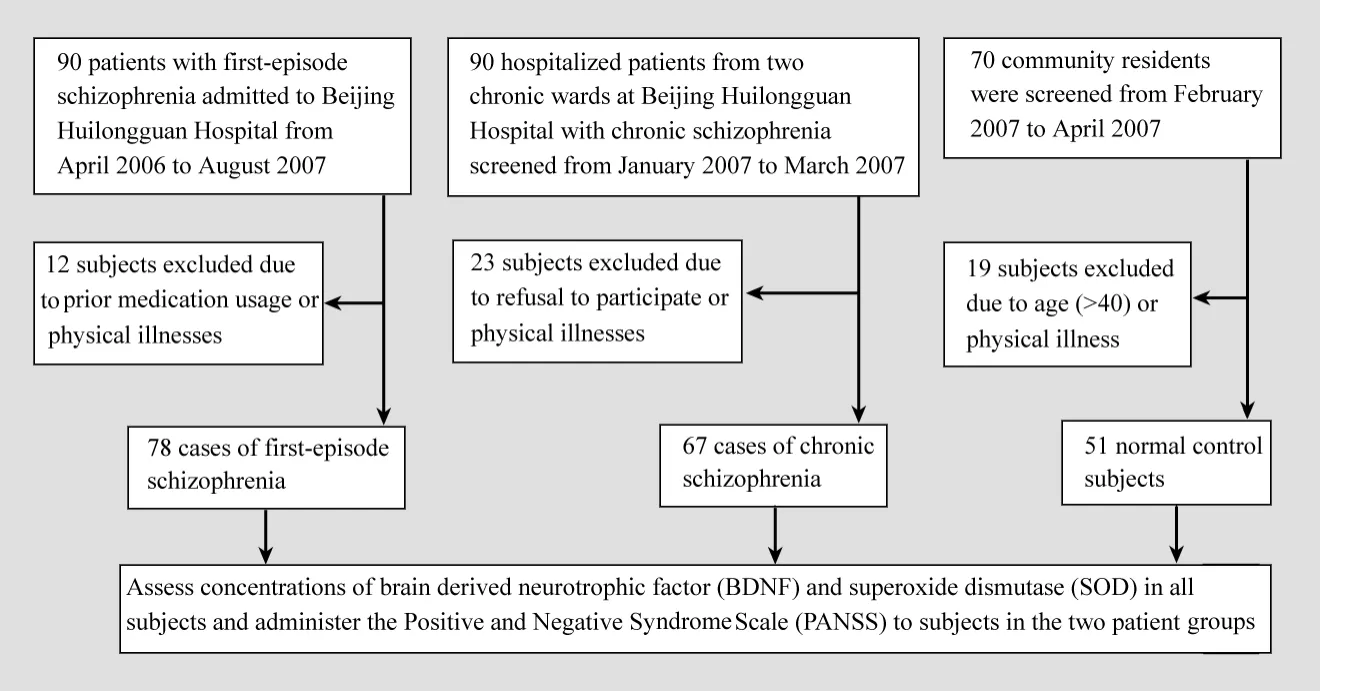
Figure 1.Flowchart of the study
Patients with first-episode schizophrenia(as defined by Lieberman and colleagues[13])admitted to the Beijing Huilongguan Hospital from April 2006 to August 2007 who met the following criteria were enrolled:1)meet DSM-IV criteria for schizophrenia[14];2)18-40 years of age;3)duration of illness of less than 60 months;4)never used antipsychotic medication or used medication for a total of less than 14 days;5)total PANSS score>60;and 6)no serious physical or neurological diseases and no history of substance abuse.Seventy-eight patients met these criteria:40 were male and 38 were female,their mean(SD)age was 32.4(7.2) years,their mean years of formal schooling was 11.6(4.1)years,and their mean duration of illness was 24.6(18.7)months.
Enrolled patients with chronic schizophrenia were inpatients on two long-stay wards at Beijing Huilongguan Hospital identified from January to March 2007 who met the same criteria as the firstepisode patients(above)except that their duration of illness was>60 months and they had a prior history of medication usage.The 67 patients with chronic schizophrenia enrolled included 35 males and 32 females,their mean(SD)age was 33.4(4.2) years,their mean years of schooling was 10.1 (1.8)years,and their mean duration of illness was 400(53)months.These patients had been on a stable dosage of antipsychotic medication for at least one month prior to enrolment:19 were taking risperidone,27 clozapine,4 quetiapine and 17 were taking first generation antipsychotics.The mean chlorpromazine-equivalent dose was 479 (256)mg/d.
Normal control subjects were volunteers recruited from the Wenhua community in the Huilongguan District of Beijing,a typical urban neighborhood in Beijing.Individuals who were outside the age range of the patient groups(i.e.,18-40),had serious physical or neurological diseases,had a history of substance abuse,or had a family history of mental illness were excluded.The 51control subjects enrolled included 26 males and 25 females,their mean(SD)age was 32.3(5.7) years and their mean years of schooling was 12.2 (3.2)years.
There were no significant differences in age,gender or education level between the three groups.All subjects or their guardians provided written consent to participate in the study.The study was approved by the Ethics Committee of the Beijing Huilongguan Hospital.
2.2 Methods
2.2.1 Measurement of laboratory indices
Five milliliters of venous blood was collected at 6:30-7:00 in the morning from subjects(who had fasted for 10-12 hour),refrigerated at 4℃for four hours and centrifuged at 3000 g for 10 minutes.Then the serum was refrigerated at-70℃.A STEKOL1300 spectrophotometer was used to determine the absorbance for total superoxide dismutase (T-SOD)and cuprozinc-superoxide dismutase (Cu-ZnSOD)using kits provided by the Nanjing Jiancheng Engineering Institute.(Extracellular SOD can be divided into Cu-ZnSOD and MnSOD,and the sum of these two kinds of SOD is labelled TSOD.)The results were converted into activity units based on standard formulas.BDNF levels were assessed by a single technician using a standardized method with enzyme-linked immunosorbent assay(ELISA)kits that were produced in the USA and provided by the Beijing Central Plains Leading Science Company.The mean result from two assessments of each sample is reported.The intraclass and interclass differences for the BDNF measure were 5%and 7%.
2.2.2 Scale assessment
Background data obtained from all enrolled subjects included basic demographic information,psychiatric history,and family history.The two patient groups were also administered the Positive and Negative Syndrome Scale(PANSS)[15]at the time of enrollment by two attending-level psychiatrists who were not aware of the results of the blood tests and who had good interrater reliability(intraclass correlation coefficient for the total PANSS score for six patients simultaneously evaluated by the two clinicians was 0.80).
2.3 Statistical analysis
Analyses were conducted using SPSS(version 11.5)software.Comparisons between the three groups of subjects used F-tests(with Dunnett T3 or C tests for subsequent pairwise comparisons)and Chi-square tests.In the two patient groups the relationship of T-SOD,Cu-ZnSOD and BDNF levels to age,duration of illness,number of hospitalizations and PANSS results were assessed using Pearson and Spearman correlation coefficients.Factors independently associated with the levels of these three compounds in the patient groups were identified using stepwise regression analyses.All statistical tests were two-tailed and used P<0.05 as the level of statistical significance.
3 Results
As shown in the Table 1 the mean activity levels of T-SOD and Cu-ZnSOD were significantly higher in the chronic schizophrenia group than in the first-episode schizophrenia group and the mean activity levels in both patient groups were higher than in the control group.Conversely,the mean blood level of BDNF was significantly lower in the chronic schizophrenia group than in the first-episode group and the mean levels in both patient groups were significantly lower than in the control group.
In the control group there was no statistically significant correlation between BDNF blood levels and T-SOD activity level(r=0.07,P=0.621)or Cu-ZnSOD activity level(r=0.03,P=0.804).In the first-episode patient group BDNF blood level was not significantly correlated with the T-SOD activity level(r=-0.13,P=0.283)but it was significantly correlated with the Cu-ZnSOD activity level(r=-0.24,P=0.038).In the chronic patient group the correlationship of BDNF blood levels with the T-SOD activity level(r=-0.11,P=0.145)and with the Cu-ZnSOD activity level(r=0.06,P= 0.722)were not statistically significant.

Table 1.Mean(SD)SOD and BDNF levels among the subiects in the three grouPs
Table 2 shows the relationship between BDNF,T-SOD and Cu-ZnSOD levels and various clinical characteristics of first-episode and chronic patients. In first-episode patients age is unrelated to any of the three parameters but duration of illness is negatively correlated with Cu-ZnSOD activity and positively correlated with BDNF levels.But in chronic patients both age and duration are positively correlated with T-SOD activity and negatively correlated with BDNF.The number of hospitalizations was not significantly correlated with any of the indicies in either of the patient groups.Measures of the severity of different types of symptoms(i.e.,the total score and subscale scores of the PANSS)were not significantly associated with any of the indicies in chronic patients but in first-episode patients they were were negatively correlated with Cu-ZnSOD activity levels and positively correlated with BDNF levels.
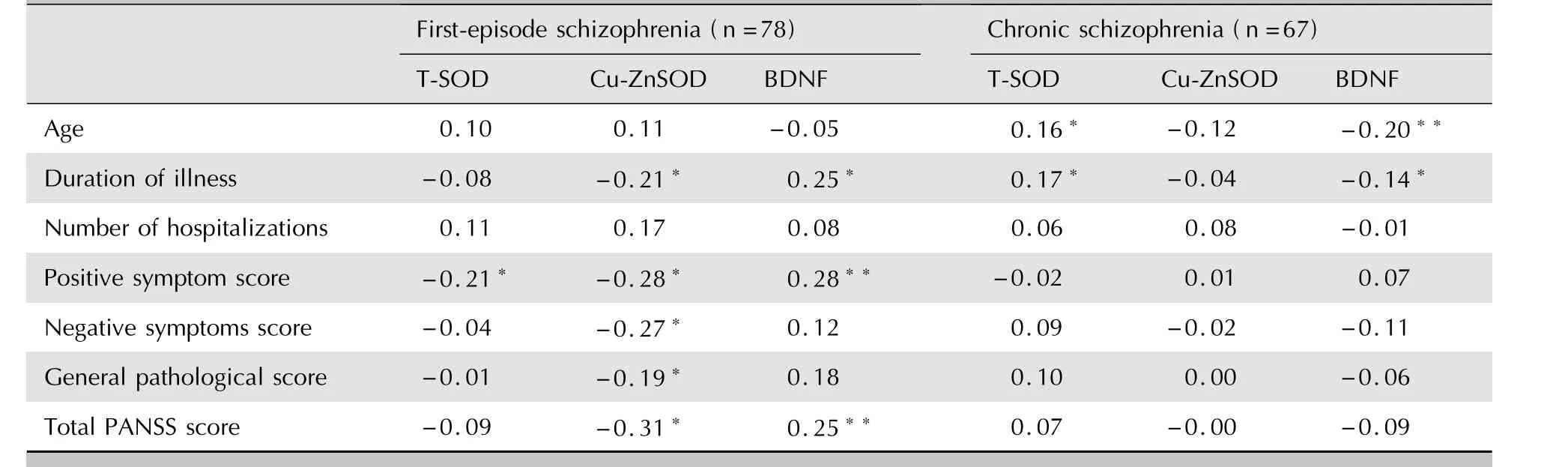
Table 2.Correlation of characteristics of Patients with first-ePisode schizoPhrenia and chronic schizoPhrenia with SOD and BDNF#
4 Discussion
4.1 Main findings
The main results from the present study were as follows.1)The activity of T-SOD and Cu-ZnSOD in the serum of patients with schizophrenia are significantly higher than in normal control subjects,but the BDNF level is significantly lower in patients with schizophrenia than in normal controls.2)TSOD and Cu-ZnSOD activity in patients with chronic schizophrenia are significantly higher than in patients in their first episode of schizophrenia but the BDNF concentration is significantly lower in chronic patients.3)SOD activity and BDNF levels are associated with symptom severity in drugnaïve,first episode schizophrenia but not in chronic schizophrenia.4)The relationship of age and duration of illness to SOD activity and BDNF levels in first-episode schizophrenia is quite different from that seen in patients with chronic schizophrenia. 5)There is little support for the hypothesized inverse relationship between SOD and BDNF in schizophrenia.
These findings are similar to the majority of studies in this area[3-6]but different from some of the previous studies.For example two papers from China[8,9]reported lower SOD activity in drugnaïve,first episode patients.In those two studies SOD activity in erythrocytes(not serum)was assessed and the duration of illness(all subjects had less than 6 months of illness)was much shorter than the mean duration of illness in the current study of 24 months.It is possible that the build-up of free radicals with hyperactive dopamine leads to an initial depletion of SOD enzymes which is only subsequently reversed as the production of the enzyme ramps up due to chronic stimulation.
This is the first study that we know of that directly compares SOD activity in drug naïve,firstepisode patients with SOD activity in chronic medicated patients.One important issue is the extent to which medication use could potentially explain the greater SOD activity in chronic versus first-episode patients.We are unable to directly address this in the current cross-sectional study but several other studies have looked at this issue.One study from China found no differences in SOD activity between chronic patients who were and were notcurrently taking medication[16].Another found no changes in SOD activity in chronic patients after 8 weeks of treatment with olanzapine[17].And two studies in chronic patients that re-introduced atypical antipsychotic medications after a drug holiday found significantly decreased SOD activity compared to the level prior to the drug holiday[2,18]. These findings support—but do not prove—the thesis that higher SOD levels in chronic schizophrenia are more likely related to the ongoing neurological processes than to the direct effect of medication. This hypothesis is supported by our finding of a positive correlation between T-SOD activity levels and duration of illness in chronic patients.
Our results for BDNF are consistent with previous reports that find significantly reduced levels of BDNF in first-episode patients[11]and in chronic patients[19]that are not substantially altered by treatment with typical or atypical antipsychotics[19-23].Our finding of lower BDNF in chronic versus first-episode patients suggests that the protective effects of BDNF may decreased with the progression of the disease.
The differences between first-episode and chronic patients in the relationship of symptom severity to SOD activity and BDNF levels was surprising.It is not clear why SOD and BDNF would be related to current symptom severity in first-episode schizophrenia but not in chronic schizophrenia.In the early phases of illness pronounced psychotic symptoms,particularly positive symptoms,may be associated with more intense dopamine activity,higher levels of free radicals and damage to the cell membranes that manufacture the SOD and,thus,reduced SOD activity.It’s possible that over time the magnitude of the dopamine hyperactivity related to symptoms decreases or a down-regulation in the response to elevated dopamine decouples symptom severity from SOD activity.The significant positive relationship of BDNF levels and symptoms in first-episode but not chronic schizophrenia is equally difficult to explain[24]and is,moreover,contradicted by another study[25]that reported a negative correlation between symptoms severity and BDNF levels in first-episode patients.
Our hypothesis about the potential negative correlationship between BDNF and SOD activity was not confirmed.The significant relationship between Cu-ZnSOD activity and BDNF level identified in first-episode patients was relatively weak (r=-0.24,P=0.038)and was one of four potential correlationships assessed(BDNF with T-SOD and BDNF with Cu-ZnSOD in both first-episode and chronic patients)so this may be a chance finding;it needs to be replicated before it can be considered definitive.
4.2 Limitations
This is a cross-sectional study so we were unable to assess the dynamic nature of the variables being considered.Long-term follow-up studies with substantially larger samples that would make it possible to control the many potential confounders are needed to confirm or disprove the hypothesized relationships between SOD activity,BDNF blood levels,course of illness,severity of symptoms and medication usage.
Several of the associations identified for T-SOD in the study were quite different from those identified for Cu-ZnSOD,which is one of the components of T-SOD.Presumably these differences were due to differences in the component of T-SOD in serum(MnSOD).These differences suggest differential effects or relationships for Cu-Zn-SOD and MnSOD;future studies should try to distinguish the different roles of these two types of SOD.
4.3 ImPlications
We confirm previous research that proposes a key role for free radicals,SOD activity and BDNF as markers in the causal pathway or developmental course of schizophrenia.But the study only provides weak evidence for the hypothesized relationship between BDNF and SOD activity.Substantial differences between drug naïve,first episode patients and chronic medicated patients in both the magnitude of the change in the activity of SOD and BDNF and in the direction of the relationships of SOD activity and BDNF with clinical and demographic parameters highlights the complexity of these associations.The interactions between these many factors are the likely cause for the varying results from different studies on SOD activity and BDNF in schizophrenia.
Conflict of interest
None of the authors had any conflict of interest related to this paper.
Funding
This study was supported by a grant from the Stanley Foundation(project number:03T-459,5T-726).
1. Mahadi SP,Evans.Is schizophrenia a metabolic brain disorder?Membrane phospholipid dysfunction and its therapeutic implications.Psychiatr Clin North Am,2003,26(1):85-102.
2. Chen DC,Zhou DF,Cao LY,Tan YL,Li YL,Wang N,et al.The interaction between superoxide dismutase and prolactin is involved in response to haloperidol and risperidone treatment in schizophrenia:a double-blind and randomized study.Chin J Psychiatry,2007,40(1):5-8.(in Chinese)
3. Dakhale G,Khanzode S,Khanzode S,Saoji A,Khobragade L,Turankar A.Oxidative damage and schizophrenia:the potential benefit by atypical antipsychotics.Neuropsychobiology,2004,49(4):205-209.
4. Othmen LB,Anwar M,Chiraz F,Bost M,Chazot G,Gaha L,etal.Altered antioxidant defense system in clinically stable patients with schizophrenia and their unaffected siblings.Prog Neuro psychopharmacol Biol Psychiatry,2008,32(1):155-159.
5. Dakhale G,Khanzode S,Khanzode S,Saoji A,Khobragade L,Turankar A.Oxidative damage and schizophrenia:the potential benefit by atypical antipsychotics.Neuropsychobiology,2004,49(4):205-209.
6. Sarandol A,Kirli S,Akkaya C,Altin A,Demirci M,Sarandol E. Oxidative-antioxidative systems and their relation with serum S100 B levels in patients with schizophrenia:Effects of short term antipsychotic treatment.Prog Neuro psychopharmacol Biol Psychiatry,2007,31(6):1164-1169.
7. Zhang XY,Tan YL,Cao LY,Wu GY,Xu Q,Shen Y,et al.Antioxidant enzymes and lipid peroxidation in different forms of schizophrenia treated with typical and atypical antipsychotics. Schizophr Res,2006,81(2-3):291-300.
8. Li J,Kong LL,Liu D.Study on the levels of lipid peroxide and antioxidant enzymes in first-episode schizophrenia.China Modern Medicine,2010,17(17):7-8.(in Chinese)
9. Yan XX,Niu AJ.The analysis of SOD and GSH-Px in patients with schizophrenia.Journal of Psychiatry,2007,20(4):202-203.(in Chinese)
10. Lewin GR,Barde YA.Physiology of the neuortorphins.Annu Rev Neurosc,1996,19:289-317.
11. Rizos EN,Rontos I,Laskos E,Arsenis G,Michalopoulou PG,Vasilopoulos D,et al.Investigation of serum BDNF levels in drug-naive patients with schizophrenia.Prog Neuro psychopharmacol Biol Psychiatry,2008,32(5):1308-1311.
12. Wang ZR,Zhou DF,Cao LY,Tan YL,Zhang XY,Li J,et al. Brain-derived neurotrophic factor polymorphisms and smoking in schizophrenia.Schizophrenia Res,2007,97(3):299-301.
13. Lieberman JA,Phillips M,Gu HB,Stroup S,Zhang P,Kong L,et al.Atypical and conventional antipsychotic drugs in treatment-naive first-episode schizophrenia:A 52-week randomized trial of clozapine vs chlorpromazine.Neuropsychopharmacology,2003,28(5):995-1003.
14. American Psychiatric Association.Diagnostic and statistical manual of mental disorders.4th ed.Washington,DC:American Psychiatric Press,1994:1-15.
15. He YL,Zhang MY.The Chinese norm and factor analysis of PANSS.Chinese Journal Clinical Psychology,2000,8(2):65-69.(in Chinese)
16. Zhang ZJ,Peet M,Shah S,Ramchand CN.The involvement of free radical in schizophrenia and relationship with clinical symptoms and antipsychotic treatment.Journal of Clinical Psychiatry,2000,10:129-131.(in Chinese)
17. Atmacu M,Tezcan E,Kuloglu M,Ustundag B,Kirtas O.The effect of extract of ginkgo biloba addition to olanzapine on therapeutic effect and antioxidant enzyme levels in patients with schizophrenia.Psychiatry Clini Neurosci,2005,59(6):652-656.
18. Dakhale G,Khanzode S,Khanzode S.Oxidative damage and schizophrenia:The potential benefit by atypical antipsychotics.Neuropsychobiology,2004,49(4):205-209.
19. Xiu MH,Hui L,Dong YF,Hou TD,Zhang CX,Zheng YL,et al.Decreased serum BDNF levels in chronic institutionalized schizophrenia on long-term treatment with typical and antipsychotic.Prog Neuro psychopharmacol Biol Psychiatry,2009,33(8):1508-1512.
20. Valvassori SS,Stertz L,Andreazza AC,Rosa MI,Kapczinski F,Streck EL,et al.Lack of effect of antipsychotics on BNDF and NGF levels in hippocampus of Wistar rats.Metab Brain Dis,2008,23(23):213-219.
21. Chen DC,Li YL,Xiu MH,Wang N,Yang KB,Nie Y,et al. Effect of risperidone treatment on serum levels of BDNF and the correlation of between serum BDNF levels and clinical efficiency and cognition improvement in first-episode schizophrenic patients.Chin J Nerv Ment Dis,2010,36(9):529-532.(in Chinese)
22. Yoshimura R,Hori H,Sugita A,Ueda N,Kakihara S,Umene W,et al.Treatment with risperidone for 4 weeks increased plasma 3-methoxy-4-hydroxypnenylglycol(MHPG)levels,but did not alter plasma brain-derived neurotrophic factor (BDNF)levels in schizophrenic patients.Prog Neuro psychopharmacol Biol Psychiatry,2007,31(5):1072-1077.
23. Bai O,Chlan-Fourney J,Bowen R,Keegan D,Li XM.Expression of brain-derived neurotrophic factor mRNA in rat hippocampus after treatment with antipsychotic drugs.J Neurosci Res,2003,71(1):127-131.
24. Buckley PF,Pillai A,Evans D,Stirewalt E,Mahadik S.Brain derived neurotropic factor in first-episode psychosis.Schizophr Res,2007,91(1-3):1-5.
25. Narita M,Aoki K,Takagi M,Yajima Y,Suzuki T.Implication of brain-derived neurotrophic factor in the release of dopamine and dopamine-related behaviors induced by methamphetamine.Neuroscience,2003,119(3):767-775. (received date:2011-04-08;accepted date:2011-09-07)
首发和慢性精神分裂症患者、正常对照者超氧化物歧化酶及脑源性神经营养因子水平的差异
陈大春1杨可冰1王 宁1聂 鹰1修梅红1李艳丽1卞清涛1张向阳1李占江2
1北京回龙观医院,100096;2首都医科大学附属北京安定医院10008。
张向阳,电子信箱zhangxy9@gmail.com
背景有研究认为精神分裂症患者脑源性神经营养因子(brain derived neurotrophic factors,BDNF)含量降低,超氧化物歧化酶(superoxide dismutase,SOD)活性异常,但结果并不完全一致,可能与研究对象不同有关。
目的探讨25例首发精神分裂症、慢性精神分裂症患者与正常人体内SOD活性、BDNF含量差异。评估病人组SOD、BDNF与临床特征的关系。
方法收集符合美国精神障碍诊断与统计手册第4版诊断标准的首发精神分裂症住院患者78例,慢性精神分裂症住院患者67例,正常对照51名。以阳性和阴性综合征量表(Positive and Negative Syndrome Scale,PANSS)评定精神症状,同时检测3组对象血SOD活性及BDNF含量。
结果慢性精神分裂症患者组总超氧化物歧化酶(total superoxide dismutase,T-SOD)与铜锌超氧化物歧化酶(cuprozinc-superoxide dismutase,Cu-ZnSOD)活性最高,首发精神分裂症患者组次之,正常对照组最低。与之相反,慢性精神分裂症患者组血BDNF含量最低,首发精神分裂症患者组次之,正常对照组最高(所有差异均有统计学意义)。首发精神分裂症患者组的BDNF与Cu-ZnSOD呈负相关(r=-0.24,P=0.038),但在正常对照组与慢性精神分裂症患者组无此负相关;3组的BDNF与T-SOD均不相关。在未服药的首发精神分裂症患者中,精神症状的严重程度与血清Cu-ZnSOD水平存在显著负相关,(主要是阳性症状)与BDNF水平存在显著正相关,但在服药的慢性患者中无上述相关。
结论与首发精神分裂症患者相比,慢性精神分裂症患者的血清SOD活性增加,血BDNF含量下降。首发精神分裂症患者的SOD活性与血BDNF含量与疾病严重程度相关,但此关联随着疾病进展而逐渐弱化。
精神分裂症 脑源性神经营养因子 自由基 超氧化物歧化酶 病例对照研究
10.3969/j.issn.1002-0829.2011.05.005
1Beijing Huilongguan Hospital,Beijing,China,100096;
2Beijing Anding Hospital,Capital Medical University,Beijing,100088 China*Correspondence:zhangxy9@gmail.com
- 上海精神医学的其它文章
- 精神分裂症的全基因组关联分析研究
- ComParison of the neuroPsychological characteristics of two subtyPes of mild cognitive imPairment
- Randomized controlled trial comParing quetiaPine with lithium and clozaPine with lithium in the treatment of female Patients with mania
- Changes in the level of micro RNA-206 gene exPression in Patients with tyPe I biPolar disorder before and after treatment and comParison with a control PoPulation
- Case-control study of changes in bone mineral density in drug-naïve Patients in the first-ePisode of schizoPhrenia during the first year of treatment with risPeridone
- Binary outcome variables and logistic regression models

