Advances in prognostic factors in acute pancreatitis: a mini-review
Theodoros E Pavlidis, Efstathios T Pavlidis and Athanasios K Sakantamis
Thessaloniki, Greece
Advances in prognostic factors in acute pancreatitis: a mini-review
Theodoros E Pavlidis, Efstathios T Pavlidis and Athanasios K Sakantamis
Thessaloniki, Greece
BACKGROUND:Early assessment of the severity of acute pancreatitis is essential to the proper management of the disease. It is dependent on the criteria of the Atlanta classification system.
DATA SOURCES:PubMed search of recent relevant articles was performed to identify information about the severity and prognosis of acute pancreatitis.
RESULTS:The scoring systems included the Ranson's or Glasgow's criteria≥3, the APACHE II classification system≥8, and the Balthazar's criteria≥4 according to the computed tomography enhanced scanning findings. The single factors on admission included age >65 years, obesity, hemoconcentration (>44%), abnormal chest X-ray, creatinine >2 mg/dl, C-reactive protein>150 mg/dl, procalcitonin >1.8 ng/ml, albumin <2.5 mg/dl, calcium <8.5 mg/dl, early hyperglycemia, increased intra-abdominal pressure, macrophage migration inhibitory factor, or a combination of IL-10 >50 pg/ml with calcium <6.6 mg/dl.
CONCLUSION:The prediction of the severity of acute pancreatitis is largely based on well defined multiple factor scoring systems as well as several single risk factors.
(Hepatobiliary Pancreat Dis Int 2010; 9: 482-486)
acute pancreatitis; severity prediction; risk factor; prognostic sign; scoring system; infected necrosis
Introduction
A variety of prognostic factors and scoring systems have been proposed for accurate assessment of the severity of acute pancreatitis and reliable prediction of high risk and potentially fatal cases. However, most of them are based on small populations, usually from single specialist centres. So far, acute physiology and chronic health evaluation (APACHE) II, although complicated, ensures the highest positive predictive value up to 69%. This is quite important since the most prognostic variables are related to high but low negative predictive values. Except for the APACHE II, the other prognostic scoring systems are not adequately sensitive, specific in prediction.[1]
The severity of acute pancreatitis is determined to predict the prognosis of the disease and differentiate the less severe from severe patients who need monitoring in ICU. The currently used the classification system of Atlanta is based on the consensus of an international symposium held in 1992 in which severe acute pancreatitis is defined to be associated with specific clinical manifestations, Ranson's prognostic criteria ≥3 points or APACHE II ≥8, multiple organ dysfunction (MOD) in the course of systemic inflammatory response syndrome (SIRS), and pancreatic necrosis.[2-5]
The pancreatic necrosis is characterized by either pathologically confirmed necrosis of the parenchyma or fat in the interstitial space. There was no up-taking shown by the parenchyma contrast medium sized >3 cm or more than 30% of the gland on dynamic CT (Balthazar's criteria).
The clinical manifestations of acute pancreatitis included abdominal tenderness, guarding, flatulence, hypotension, respiratory distress, palpable mass, or bruising (Grey-Turner's sign periumbilically or Cullen's sign in the loin region, observed in only 1%-3% of cases after 48 hours).
Prognostic scoring systems
The Ranson's prognostic criteria (1974) include 11factors (age, white cell count, LDH, SGPT, glucose, fall in hematocrit, urea, calcium, PO2, base deficit, fluid replacement) (Table 1).[6]The Glasgow's prognostic criteria modified by Imrie (1978) includes 8 factors (white cell count, glucose, urea, PO2, calcium, LDH, transaminases, albumin) (Table 2).[7]
Formerly the criteria of APACHE system acute physiology and chronic health evaluation included 34 factors (1981), which are difficult to use. This promptedus to modify APACHE II (1985), which includes 12 factors widely used today (Table 3). These factors include age and other coexisting diseases. APACHE III (1991) includes 18 factors whereas APACHE-O (obesity-1996) includes the added one, obesity.[8-11]
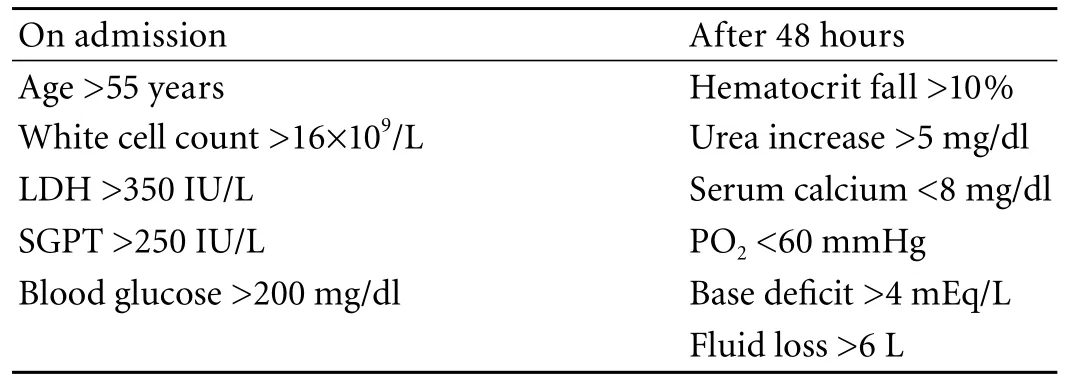
Table 1. Prognostic criteria of Ranson
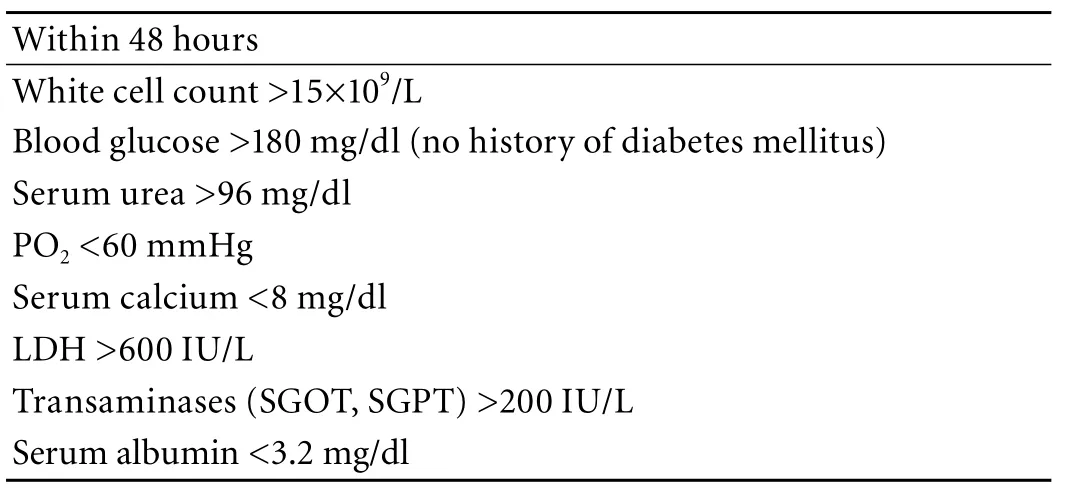
Table 2. Prognostic criteria of Glasgow
The prognostic criteria of Balthazar (1985) are based on the findings of CT and classified into 5 grades (A: normal findings, B: focal or diffuse swelling of the pancreas, C: inflammation of the pancreas and peripancreatic fat, D: one peripancreatic fluid collection, and E: two or more collections or endo/peri-pancreatic air presence). They are scored from 0-4 points, respectively.[12]The same author later in 1990, based on the findings of dynamic CT with intravenous contrast medium, added one more criterion (F: degree of necrosis 30%, 50% or more), giving 2, 4 or 6 extra points, respectively.[13]
Also, dynamic CT is useful in predicting local complications in patients with pancreatic necrosis by assessing some well-defined factors for infected pancreatic necrosis development, i.e. the extent of pancreatic necrosis and the presence of peripancreatic necrosis. The finding of transparenchymal necrosis with up-stream viable (enhancing), pancreatic and no peripancreatic necrosis, is yet another factor for pseudocyst formation.[14]
Single prognostic factors
As individual predictors of severe acute pancreatitis are now considered, obesity with body mass index (BMI): 25-30 kg/m2(+), >30 kg/m2(++), pleural effusion or pulmonary infiltration within the first 24 hours is associated withincreased mortality, increased serum creatinine level (>2 mg/dl).[15-17]Also, the composition of peritoneal fluid (amount, color) after 8 hours is considered as a prognostic criterion in equal value with the Ranson's and Glasgow's criteria.[2]The hemoconcentration, reflected by an increase in hematocrit on admission, is associated with the development of severe necrotizing pancreatitis. Thus it is considered as a simple, useful and early prognostic marker. The patients with no hemoconcentration have minimal risk to develop organ failure or death.[18-21]
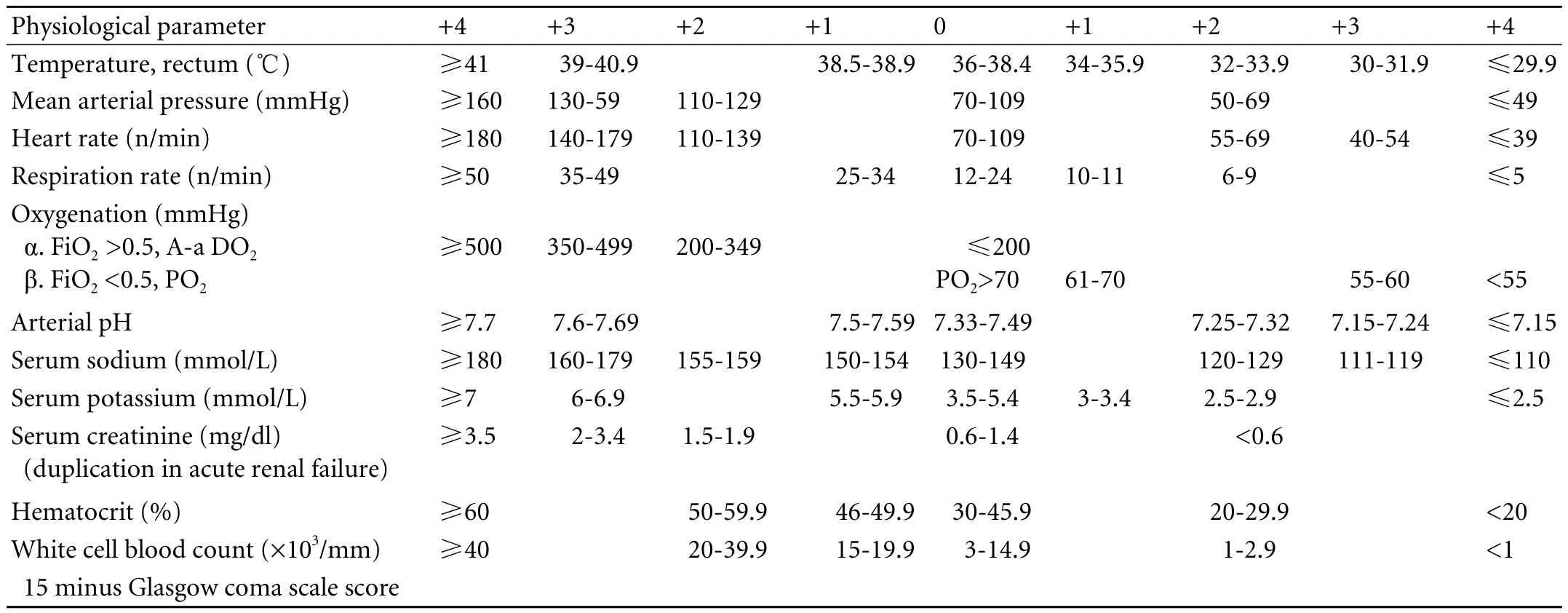
Table 3. APACHE II scoring system
Much effort, nowadays, has been concentrated on simple prognostic scoring systems. In a recent study[22]independent prognostic factors associated with poor prognosis have been determined, i.e. age above 65 years, leukocyte count above 13 000/mm3, serum albumin level below 2.5 mg/dl, serum calcium below 8.5 mg/dl and C-reactive protein (CRD) above 150 mg/dl.
Apart from these some prognostic factors in serum are used separately to determine the severity of acute pancreatitis. The main factors include those that determine the inflammatory response and consist of acute phase proteins CRP (150 mg/dl is currently the limit of discrimination of the severe from mild one) and amyloid A, polymorphonuclear elastase, cytokines (IL-6, IL-8, IL-10), phospholipase A2, thrypsin, antithrypsin, thrypsinogen activation peptide, carboxypeptidase activation peptide, beta2 macroglobulin and procalcitonin (1.8 ng/ml is the threshold to distinguish between infected and non-infected pancreatic necrosis).[2]Between acutephase proteins (such as serum amyloid A, CRP) and procalcitonin as prognostic factors in acute pancreatitis, the latter gained the best prognostic value with a cutoff level at 0.5 ng/ml; also, some single parameters such as total calcium concentration, lactic acid activity and glucose concentration share equal prognostic value.[23]
However, the CRP has the best practical value and is widely used as a predictor of severe acute pancreatitis; but it should be increased at least 48 hours after elapse from the onset of the episode. Its value is comparable to that of system APACHE II.[15,16]Instead of this, the procalcitonin could be used as a predictor of severe acute pancreatitis in the first 24 hours; even the monitoring of changes reflects the course of the disease.[24,25]
The markers that determine the extent of pancreatic lesion via the activation of pancreatic enzymes are mainly used in research and have not yielded yet relevant clinical application.
The anti-inflammatory cytokines (IL-10, receptor antagonist of IL-1 and soluble receptors of TNF), which reflect the degree of immune response, are increased early and now gain an intense research interest. The combination of anti-inflammatory cytokine interleukin 10 (IL-10 >50 pg/ml) and serum calcium (Ca <6.6 mg/dl) within 12 hours after the onset is considered currently as the best predictor of impending multiple organ failure with high diagnostic accuracy.[26]
Recent interesting aspects
It has been postulated that the degree of inflammation and pancreatic necrosis in severe acute pancreatitis may be associated with the risk of disease recurrence.[27]Also, in patients with severe acute pancreatitis, as independent prognostic factors for arterial injury (pseudo-aneurysm) and gastrointestinal complications (duodenal perforations) the persistent elevation of CRP and the high Balthazar's CT severity score are determined.[28]
The above mentioned parameters including hematocrit, urea, creatinine, matrix metalloproteinase-9 (MMP-9) and amyloid A have been used nowadays, as early predictors of severity of acute pancreatitis within the first 24 hours.[29]Early hyperglycemia in acute pancreatitis is a prognostic indicator of severe episode. Although, obesity is not an independent risk factor for organ failure, it correlates with early hyperglycemia, which may predispose to organ failure development increasing the mortality.[30,31]
Infected pancreatic necrosis is associated with high mortality and surgery is the cornerstone in its management. Some independent predictors of survival have been defined in such surgery. Thus, pancreatic necrosectomy has been found to be related to higher mortality in patients with increased APACHE II score (mean score 14) on admission, presence of early persistent SIRS (within the first 48 hours) and MOD within two weeks after admission.[32]
APACHE II score >8, LDH >667 U/L, base excess>5, CT severity index >3, and CRP>142 mg/L reported to be of prognostic value.[33]Six factors have been used recently to develop another prognostic scoring system, i.e. arterial pH, age, serum urea, mean arterial pressure, PaO2/FiO2 ratio, AND total serum calcium.[34]
As acute pancreatitis is one of the main causes of increased intra-abdominal pressure and compartment syndrome, this pressure has been used as a reliable marker of disease severity.[35]
Another simple scoring system has been proposed according to the three prognostic factors i.e. serum urea nitrogen (≥25 mg/dl), serum LDH (≥900 IU/l), and pancreatic necrosis in contrast-enhanced CT.[36]
Recently, serum macrophage migration inhibitory factor as a potentiator of cytokine response has been proposed as an early (within 24 hours) marker ofpancreatic necrosis; but most importantly, it promises the development of novel therapeutic agents to ameliorate SIRS in acute pancreatitis.[37]
Conclusions
The risk of severe acute pancreatitis is increased at Glasgow's or Ranson's score ≥3 in 48 hours, APACHE II on admission ≥8, BMI ≥30, abdominal wall bruising, abnormal chest radiograph and serum creatinine >2 mg/dl on admission, Balthazar's score ≥4, CRP >150 mg/dl at 48 hours, and hematocrit >44%. Likewise, the risk of dying is increased at Glasgow's or Ranson's score ≥3 in 48 hours, APACHE II ≥15, abnormal chest radiograph and serum creatinine >2 mg/dl on admission, and Balthazar's score ≥7. In our opinion, the better single factor useful in daily practice is CRP >150 mg/dl or procalcitonin >0.5 ng/ml for determination of severe acute pancreatitis; also, procalcitonin >1.8 ng/ml can indicate infected pancreatic necrosis.
Funding:None.
Ethical approval:Not needed.
Contributors:PTE wrote the main body of the article with the help of PET under the supervision of SAK. PET provided advice on literature data and their interpretation, while SAK provided advice on medical aspects. PTE is the guarantor.
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Gravante G, Garcea G, Ong SL, Metcalfe MS, Berry DP, Lloyd DM, et al. Prediction of mortality in acute pancreatitis: a systematic review of the published evidence. Pancreatology 2009;9:601-614.
2 Triester SL, Kowdley KV. Prognostic factors in acute pancreatitis. J Clin Gastroenterol 2002;34:167-176.
3 Gerlach H. Risk management in patients with severe acute pancreatitis. Crit Care 2004;8:430-432.
4 Bank S, Singh P, Pooran N, Stark B. Evaluation of factors that have reduced mortality from acute pancreatitis over the past 20 years. J Clin Gastroenterol 2002;35:50-60.
5 Tenner S. Initial management of acute pancreatitis: critical issues during the first 72 hours. Am J Gastroenterol 2004;99: 2489-2494.
6 Ranson JH, Rifkind KM, Roses DF, Fink SD, Eng K, Spencer FC. Prognostic signs and the role of operative management in acute pancreatitis. Surg Gynecol Obstet 1974;139:69-81.
7 Imrie CW, Benjamin IS, Ferguson JC, McKay AJ, Mackenzie I, O'Neill J, et al. A single-centre double-blind trial of Trasylol therapy in primary acute pancreatitis. Br J Surg 1978;65:337-341.
8 Wilson C, Heath DI, Imrie CW. Prediction of outcome in acute pancreatitis: a comparative study of APACHE II, clinical assessment and multiple factor scoring systems. Br J Surg 1990;77:1260-1264.
9 Jones HJ, de Cossart L. Risk scoring in surgical patients. Br J Surg 1999;86:149-157.
10 Connor S, Ghaneh P, Raraty M, Rosso E, Hartley MN, Garvey C, et al. Increasing age and APACHE II scores are the main determinants of outcome from pancreatic necrosectomy. Br J Surg 2003;90:1542-1548.
11 Toh SKC, Walters J, Johnson CD. APACHE-O: a new predictor of severity in acute pancreatitis. Gut 1996;38:A35.
12 Balthazar EJ, Ranson JH, Naidich DP, Megibow AJ, Caccavale R, Cooper MM. Acute pancreatitis: prognostic value of CT. Radiology 1985;156:767-772.
13 Balthazar EJ, Robinson DL, Megibow AJ, Ranson JH. Acute pancreatitis: value of CT in establishing prognosis. Radiology 1990;174:331-336.
14 Ocampo C, Zandalazini H, Kohan G, Silva W, Szelagowsky C, Oría A. Computed tomographic prognostic factors for predicting local complications in patients with pancreatic necrosis. Pancreas 2009;38:137-142.
15 Mayerle J, Hlouschek V, Lerch MM. Current management of acute pancreatitis. Nat Clin Pract Gastroenterol Hepatol 2005;2:473-483.
16 Pitchumoni CS, Patel NM, Shah P. Factors influencing mortality in acute pancreatitis: can we alter them? J Clin Gastroenterol 2005;39:798-814.
17 Martínez J, Sánchez-Payá J, Palazón JM, Suazo-Barahona J, Robles-Díaz G, Pérez-Mateo M. Is obesity a risk factor in acute pancreatitis? A meta-analysis. Pancreatology 2004;4:42-48.
18 Brown A, Orav J, Banks PA. Hemoconcentration is an early marker for organ failure and necrotizing pancreatitis. Pancreas 2000;20:367-372.
19 Lankisch PG, Mahlke R, Blum T, Bruns A, Bruns D, Maisonneuve P, et al. Hemoconcentration: an early marker of severe and/or necrotizing pancreatitis? A critical appraisal. Am J Gastroenterol 2001;96:2081-2085.
20 Baron TH. Predicting the severity of acute pancreatitis: is it time to concentrate on the hematocrit? Am J Gastroenterol 2001;96:1960-1961.
21 Gan SI, Romagnuolo J. Admission hematocrit: a simple, useful and early predictor of severe pancreatitis. Dig Dis Sci 2004;49:1946-1952.
22 Gonzálvez-Gasch A, de Casasola GG, Martín RB, Herreros B, Guijarro C. A simple prognostic score for risk assessment in patients with acute pancreatitis. Eur J Intern Med 2009;20: e43-48.
23 Gurda-Duda A, Kusnierz-Cabala B, Nowak W, Naskalski JW, Kulig J. Assessment of the prognostic value of certain acutephase proteins and procalcitonin in the prognosis of acute pancreatitis. Pancreas 2008;37:449-453.
24 Ammori BJ, Becker KL, Kite P, Snider RH, Nylén ES, White JC, et al. Calcitonin precursors in the prediction of severity of acute pancreatitis on the day of admission. Br J Surg 2003;90:197-204.
25 Modrau IS, Floyd AK, Thorlacius-Ussing O. The clinical value of procalcitonin in early assessment of acute pancreatitis. Am J Gastroenterol 2005;100:1593-1597.
26 Mentula P, Kylänpää ML, Kemppainen E, Jansson SE, Sarna S, Puolakkainen P, et al. Early prediction of organ failure bycombined markers in patients with acute pancreatitis. Br J Surg 2005;92:68-75.
27 Yasuda T, Ueda T, Takeyama Y, Shinzeki M, Sawa H, Nakajima T, et al. Long-term outcome of severe acute pancreatitis. J Hepatobiliary Pancreat Surg 2008;15:397-402.
28 Hagiwara A, Miyauchi H, Shimazaki S. Predictors of vascular and gastrointestinal complications in severe acute pancreatitis. Pancreatology 2008;8:211-218.
29 Al Mofleh IA. Severe acute pancreatitis: pathogenetic aspects and prognostic factors. World J Gastroenterol 2008;14:675-684.
30 Mentula P, Kylanpaa ML, Kemppainen E, Puolakkainen P. Obesity correlates with early hyperglycemia in patients with acute pancreatitis who developed organ failure. Pancreas 2008;36:e21-25.
31 Martínez J, Johnson CD, Sánchez-Payá J, de Madaria E, Robles-Díaz G, Pérez-Mateo M. Obesity is a definitive risk factor of severity and mortality in acute pancreatitis: an updated meta-analysis. Pancreatology 2006;6:206-209.
32 Mofidi R, Lee AC, Madhavan KK, Garden OJ, Parks RW. Prognostic factors in patients undergoing surgery for severe necrotizing pancreatitis. World J Surg 2007;31:2002-2007.
33 Kaya E, Dervisoglu A, Polat C. Evaluation of diagnostic findings and scoring systems in outcome prediction in acute pancreatitis. World J Gastroenterol 2007;13:3090-3094.
34 Harrison DA, D'Amico G, Singer M. The Pancreatitis Outcome Prediction (POP) Score: a new prognostic index for patients with severe acute pancreatitis. Crit Care Med 2007; 35:1703-1708.
35 Rosas JM, Soto SN, Aracil JS, Cladera PR, Borlan RH, Sanchez AV, et al. Intra-abdominal pressure as a marker of severity in acute pancreatitis. Surgery 2007;141:173-178.
36 Ueda T, Takeyama Y, Yasuda T, Matsumura N, Sawa H, Nakajima T, et al. Simple scoring system for the prediction of the prognosis of severe acute pancreatitis. Surgery 2007;141: 51-58.
37 Rahman SH, Menon KV, Holmfield JH, McMahon MJ, Guillou JP. Serum macrophage migration inhibitory factor is an early marker of pancreatic necrosis in acute pancreatitis. Ann Surg 2007;245:282-289.
June 28, 2010
Accepted after revision September 2, 2010
Author Affiliations: Surgical Propedeutical Department, Medical School, Aristotle University of Thessaloniki, Hippocration Hospital, Konstantinoupoleos 49, 54642 Thessaloniki, Greece (Pavlidis TE, Pavlidis ET and Sakantamis AK)
Theodoros E Pavlidis, MD, PhD, Associate Professor of Surgery, A Samothraki 23, 54248 Thessaloniki, Greece (Tel: +302310-992861; Fax: +302310-992932; Email: pavlidth@otenet.gr; pavlidth@med.auth.gr; pavlidth@auth.gr)
© 2010, Hepatobiliary Pancreat Dis Int. All rights reserved.
 Hepatobiliary & Pancreatic Diseases International2010年5期
Hepatobiliary & Pancreatic Diseases International2010年5期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- News
- Resection of hepatic caudate lobe hemangioma: experience with 11 patients
- Hepatocellular carcinoma metastatic to the kidney mimicking renal oncocytoma
- Simultaneous breast and ovarian metastasis from gallbladder carcinoma
- An eight-year journey of Hepatobiliary & Pancreatic Diseases International
- Interferon and lamivudine combination therapy versus lamivudine monotherapy for hepatitis B e antigen-negative hepatitis B treatment: a meta-analysis of randomized controlled trials
