维生素D与复发性流产的相关性及其对妊娠结局的预测价值
史桂源,朱宝菊


摘要:目的 研究維生素D与复发性流产(RSA)的关系,并探讨维生素D对RSA患者再次妊娠结局的预测价值。方法 选取2020年6月-2021年6月于郑州大学第二附属医院定期围保的120例RSA患者作为RSA组,选取50名正常孕妇作为对照组。比较两组血清维生素D水平,以及RSA组不同妊娠结局、流产次数者维生素D水平,另采用Logistic回归分析维生素D水平与RSA发生的风险关系,ROC曲线分析维生素D对复发性流产妊娠结局的预测价值。结果 RSA组和对照组25(OH)D水平分别为(14.92±7.01)ng/ml、(20.81±9.69)ng/ml,组间比较,差异有统计学意义(P<0.05)。RSA组维生素D充足及不足占比低于对照组,缺乏及严重缺乏占比高于对照组,差异有统计学意义(P<0.05)。RSA组中继续妊娠者和流产者25(OH)D水平分别(15.93±7.05)ng/ml、(12.48±6.38)ng/ml,组间比较,差异有统计学意义(P<0.05)。不同流产次数25(OH)D水平比较,差异有统计学意义(P<0.05);Logistic回归分析显示,维生素D缺乏是RSA发生的独立危险因素;ROC曲线分析显示,维生素D预测RSA患者再次发生流产具有一定的价值,曲线下面积为0.678,截断值、灵敏度和特异度分别为11.86 ng/ml、70.60%、60.00%。结论 妊娠期女性的维生素D水平普遍缺乏,与正常孕妇比较,RSA患者孕早期血清维生素D水平较低;孕早期维生素D<11.86 ng/ml时,RSA患者再次发生流产的风险较高。
关键词:复发性流产;维生素D;妊娠结局
中图分类号:R714.2 文献标识码:A DOI:10.3969/j.issn.1006-1959.2024.08.023
文章编号:1006-1959(2024)08-0118-04
Correlation Between Vitamin D and Recurrent Spontaneous Abortion and its Predictive Value for Pregnancy Outcome
SHI Gui-yuan,ZHU Bao-ju
(Department of Obstetrics and Gynecology,the Second Affiliated Hospital of Zhengzhou University,Zhengzhou 450014,Henan,China)
Abstract:Objective To study the relationship between vitamin D and recurrent spontaneous abortion (RSA), and to explore the predictive value of vitamin D on the pregnancy outcome of RSA patients.Methods From June 2020 to June 2021, 120 patients with RSA who were regularly surrounded in the Second Affiliated Hospital of Zhengzhou University were selected as the RSA group, and 50 normal pregnant women were selected as the control group. Serum vitamin D levels were compared between the two groups, as well as vitamin D levels in RSA group with different pregnancy outcomes and abortion times. Logistic regression was used to analyze the risk relationship between vitamin D level and RSA. ROC curve was used to analyze the predictive value of vitamin D on pregnancy outcome of recurrent spontaneous abortion.Results The levels of 25 (OH) D in the RSA group and the control group were (14.92±7.01)ng/ml and (20.81±9.69)ng/ml, respectively, the difference between the two groups was statistically significant (P<0.05). The proportion of vitamin D sufficiency and insufficiency in the RSA group was lower than that in the control group, and the proportion of deficiency and severe deficiency was higher than that in the control group, with statistically significant differences (P<0.05). The levels of 25 (OH) D in continuing pregnancy and abortion in RSA group were (15.93±7.05) ng/ml and (12.48±6.38)ng/ml, respectively, and the difference between the two groups was statistically significant (P<0.05). There was significant difference in 25 (OH) D level among different abortion times (P<0.05). Logistic regression analysis showed that vitamin D deficiency was an independent risk factor for RSA. ROC curve analysis showed that vitamin D had a certain value in predicting recurrent abortion in RSA patients, the area under the curve was 0.678, and the cut-off value, sensitivity and specificity were 11.86 ng/ml, 70.60% and 60.00%, respectively.Conclusion The vitamin D level of pregnant women is generally deficient. Compared with normal pregnant women, the serum vitamin D level of RSA patients in early pregnancy is lower. When vitamin D<11.86 ng/ml in early pregnancy, RSA patients have a higher risk of recurrent abortion.
Key words:Recurrent spontaneous abortio;Vitamin D;Pregnancy outcome
复发性流产(recurrent spontaneous abortion, RSA)是现代妇产科研究的热点问题之一,是指与同一个性伴侣的连续发生至少2次及以上自然流产(包括生化妊娠),多为孕早期流产,病因复杂[1,2]。多次的流产史给再次妊娠的妇女造成了极大的心理负担,因此应该引起足够的重视。研究表明[3-5],维生素D(vitamin D)在人体免疫、胚胎着床、胎盘的血管形成中具有一定的影响,因此维生素D缺乏(vitamin D deficiency, VDD)对胎盘的发育、胚胎着床有着不利的影响[6]。据报道[7,8],近一半的复发性流产女性合并VDD。在人体内,维生素D发挥主要作用的成分是25-羟维生素D[25-hydroxyvitamin D, 25(OH)D],故25(OH)D是用来评估血清维生素D含量的最好检测指标。本研究主要目的在于研究孕早期维生素D水平和RSA的相关性,以及孕早期维生素D水平对RSA妊娠结局的预测价值,以期为RSA早期诊断及治疗提供临床依据,现报道如下。
1资料与方法
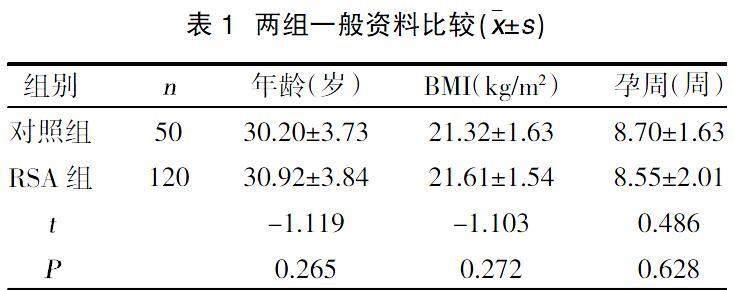
1.1一般资料 选取2020年6月-2021年6月于郑州大学第二附属医院定期围保的120例RSA患者作为RSA组。纳入标准:①符合复发性流产诊断标准;②本次妊娠孕龄为5~13+6周;③宫内单胎妊娠;④孕期规律产检并于本院分娩;⑤依从性好。排除标准:①既往合并内分泌疾病者;②合并生殖道感染者;③近3个月使用维生素D、免疫相关调节剂和干扰内分泌的药物者;④男方精液检验结果提示异常者;⑤夫妻双方染色体核型检查结果异常者;⑥彩超检查结果提示合并生殖道相关器质性病变者;⑦妊娠合并肿瘤、肝炎等疾病者;⑧接受辅助生殖技术者。同期另选取50名女性作为对照组,均未合并任何不良孕产史。两组年龄、BMI、孕周比较,差异无统计学意义(P>0.05),见表1,具有可比性。本研究由郑州大学第二附属医院的临床伦理委员会知晓并批准(批件号:2022327),患者知情同意并签署知情同意书。
1.2方法 两组受试者均在空腹时抽取静脉血3 ml,避光保存,离心分离血清,保存于-20 ℃下待检。应用酶联免疫吸附(ELISA)法检测血清25(OH)D。诊断标准[9]如下:充足为25(OH)D>30 ng/ml(75 nmol/L),不足为20~30 ng/ml(50~75 nmol/L),缺乏为<20 ng/ml(50 nmol/L),严重缺乏为<10 ng/ml(25 nmol/L)。
1.3观察指标 ①比较RSA组与对照组血清维生素D水平;②根据流产次数分组,比较不同分组间维生素D水平及差异;③妊娠结局:随访所有研究对象至孕28周,记录妊娠结局,包括继续妊娠和流产。
1.4统计学方法 本研究数据应用SPSS 23.0统计学软件进行分析,计量资料以(x±s)表示,采用t检验或Kruskal-Wallis H检验;计数资料以[n(%)]表示,采用?字2检验。维生素D水平与RSA发生的风险关系采用Logistic回归分析。维生素D对复发性流产妊娠结局的预测价值使用ROC曲线分析,以P<0.05表示差异有统计学意义。
2结果
2.1两组维生素D水平比较 RSA组和对照组25(OH)D水平分别为(14.92±7.01)ng/ml、(20.81±9.69)ng/ml,组间比较,差异有统计学意义(P<0.05)。RSA组维生素D充足及不足占比低于对照组,缺乏及严重缺乏占比高于对照组,差异有统计学意义(?字2=13.583,P=0.004),见表2。
2.2 RSA组不同妊娠结局维生素D水平比较 RSA组中继续妊娠患者85例,流产患者35例,其25(OH)D水平分别(15.93±7.05)ng/ml、(12.48±6.38)ng/ml,组间比较,差异有统计学意义(P<0.05)。
2.3 RSA组不同流产次数维生素D比较 流产次数为2、3、4次者25(OH)D水平分别为(17.20±7.95)ng/ml、(13.80±5.65)ng/ml、(11.59±4.34)ng/ml,组间比较,差异有统计学意义(H=12.964,P=0.002),即随着流产次数增加,维生素D水平越低。
2.4维生素D与RSA发生的风险关系分析 维生素D水平降低是RSA发生的危险因素[β=-0.086,SE=0.022,Wald值=14.678,OR(95%CI)=0.918(0.878,0.959),P<0.05]。
2.5孕早期維生素D对RSA妊娠结局的预测价值 ROC曲线分析显示,孕早期维生素D水平对预测RSA妊娠结局具有一定价值,其曲线下面积为0.678。当截断值为11.86 ng/ml时,其灵敏度为70.60%,特异度为60.00%,阳性预测值为45.65%,阴性预测值为81.08%,见图1。
3讨论
维生素D作为一种脂溶性类固醇激素,在阳光照射的作用下,可由皮肤内的7-脱氢胆固醇转化生成,少量也可由食物摄取的方式获得[10]。维生素D在肝脏内通过羟基化作用转化为25(OH)D。25(OH)D在血液中浓度最高、水平最稳定,是反映体内维生素D营养状况的最佳指标。目前维生素D缺乏在世界范围内极为普遍,占总人口的50%~80%,成为威胁全球人类健康的公共卫生问题[11]。不同国家及地区的孕妇维生素D缺乏率差异较大。研究表明[12],美洲有42%~72%的孕妇存在维生素D缺乏,而欧洲有18%~90%。本研究纳入了170名孕妇,其中有129名孕妇存在维生素D缺乏(包括严重缺乏),缺乏率约为75.88%。而孕期缺乏维生素D的主要原因可能是妊娠期妇女户外活动及接触阳光的时间减少[13]。孕妇体内维生素D缺乏,将严重威胁母胎健康。
维生素D缺乏可能会导致妊娠胚胎丢失、胚胎反复移植失败、妊娠期高血压等疾病。Li N等[14]研究了RSA女性的维生素D水平和蜕膜组织中维生素D受体的表达情况,发现维生素D缺乏与妊娠失败有关。Andersen LB等[15]研究结果表明,低水平的25(OH)D与孕早期流产风险增加相关。齐雅杰[16]研究也充分说明,RSA与维生素D缺乏有关,并表明RSA患者在妊娠期补充维生素D是有意义的。本研究结果显示,与对照组相比,RSA组血清25(OH)D水平降低,并且RSA组25(OH)D缺乏率及严重缺乏率高于对照组,差异有统计学意义(P<0.05);且流产次数越多,25(OH)D水平越低。经过多因素Logistic分析得出,25(OH)D水平降低是RSA发生的独立危险因素。维生素D缺乏使RSA发生风险升高的机制可能有:①体内免疫调节细胞、免疫细胞因子和自身免疫抗体水平发生异常,进而对胚胎或胎兒产生潜在毒性,影响妊娠的维持,最终导致流产的发生[17,18];②胎盘催乳素、人绒毛膜促性腺激素等女性激素的生成异常,从而导致黄体功能不足和子宫内膜容受性降低[19];③诱发病理性高凝状态,导致子宫螺旋动脉或绒毛血管血栓形成、胎盘微循环发生障碍,影响母体与胎儿的物质交换[20]。
另外本研究通过ROC曲线分析维生素D水平与RSA患者妊娠结局的关系,发现当孕早期25(OH)D<11.86 ng/ml时,预测RSA患者再次发生流产的灵敏度为70.60%,特异度为60.00%,说明维生素D<11.86 ng/ml时,再次发生流产的几率较高,提示RSA患者孕早期应进行维生素D检查,及时补充维生素D,避免因营养元素缺乏导致再次流产的发生,减少再次流产给患者及家庭带来的伤害。
综上所述,妊娠期妇女维生素D普遍缺乏,维生素D缺乏可增加RSA发生的风险,孕早期维生素D水平可作为RSA妊娠结局的预测指标之一。建议在临床工作中,强调RSA患者常规筛查维生素D的重要性,对于维生素D缺乏的患者及时给予治疗,降低再次流产的发生率。
参考文献:
[1]中华医学会妇产科学分会产科学组,复发性流产诊治专家共识编写组.复发性流产诊治专家共识(2022)[J].中华妇产科杂志,2022,57(9):653-667.
[2]Eshre Guideline Group on RPL,Bender Atik R,Christiansen OB,et al.ESHRE guideline: recurrent pregnancy loss[J].Human Reproduction Open,2018,2018(2):hoy004.
[3]Mashiach S.Recurrent Pregnancy Loss: Causes, Controversies, and Treatment[J].Isr Med Assoc J,2021,23(1):64-65.
[4]Chen X,Diao L,Lian R,et al.Potential impact of maternal vitamin D status on peripheral blood and endometrium cellular immunity in women with recurrent implantation failure[J].Am J Reprod Immunol,2020,84(1):e13243.
[5]Li D,Zheng L,Zhao D,et al.The role of immune cells in recurrent spontaneous abortion[J].Reproductive Sciences,2021,28(12):3303-3315.
[6]Zhao R,Zhang W,Ma C,et al.Immunomodulatory function of vitamin D and its role in autoimmune thyroid disease[J].Frontiers in Immunology,2021,12:574967.
[7]何湘娇,赵静,张琼,等.血清与卵泡液25-羟维生素D水平与体外受精-胚胎移植妊娠结局的相关性研究[J].中华生殖与避孕杂志,2020,40(4):271-278.
[8]Zhou X,Li B,Wang C,et al.Study on the changes in TSH,TPO-Ab and other indicators due to Vitamin D deficiency in Pregnant Women with subclinical hypothyroidism in the first trimester[J].Pakistan Journal of Medical Sciences,2020,36(6):1313.
[9]Keller A,Varela Vazquez C,Dangol R,et al.The role of vitamin D in the development of diabetes post gestational diabetes mellitus:A systematic literature review[J].Nutrients,2020,12(6):1733.
[10]Bao W,Song Y,Bertrand KA,et al.Prepregnancy habitual intake of vitamin D from diet and supplements in relation to risk of gestational diabetes mellitus:A prospective cohort study[J].Journal of Diabetes,2018,10(5):373-379.
[11]Holick Michael F.The vitamin D deficiency pandemic:Approaches for diagnosis,treatment and prevention [J].Reviews in Endocrine and Metabolic Disorders,2017,18(2):153-165.
[12]Saraf R,Morton SMB,Camargo Jr CA,et al.Global summary of maternal and newborn vitamin D status–a systematic review[J].Maternal & Child Nutrition,2016,12(4):647-668.
[13]Pilz S,Zittermann A,Obeid R,et al.The role of vitamin D in fertility and during pregnancy and lactation:a review of clinical data[J].International Journal of Environmental Research and Public Health,2018,15(10):2241.
[14]Li N,Wu HM,Hang F,et al.Women with recurrent spontaneous abortion have decreased 25(OH) vitamin Dand VDR at the fetal-maternal interface [J].Braz J Med Biol Res,2017,50(11):e6527.
[15]Andersen LB,J?覬rgensen JS,Jensen TK,et al.Vitamin D insufficiency is associated with increased risk of first-trimester miscarriage in the Odense Child Cohort[J].American Journal of Clinical Nutrition,2015,102(3):633-638.
[16]齐雅杰.维生素D与复发性流产的关系研究[D].呼和浩特:内蒙古医科大学,2019.
[17]Dzik KP,Kaczor JJ.Mechanisms of vitamin D on skeletal muscle function:oxidative stress,energy metabolism and anabolic state[J].European Journal of Applied Physiology,2019,119:825-839.
[18]Jueraitetibaike K,Ding Z,Wang DD,et al.The effect of vitamin D on sperm motility and the underlying mechanism[J].Asian Journal of Andrology,2019,21(4):400.
[19]Kuyucu Y,Sencar L,Tap ?魻,et al.Investigation of the effects of vitamin D treatment on the ovarian AMH receptors in a polycystic ovary syndrome experimental model:an ultrastructural and immunohistochemical study[J].Reproductive Biology,2020,20(1):25-32.
[20]Wan L,Gu J,Liu T,et al.Clinical performance of automated chemiluminescent methods for anticardiolipin and anti‐β2‐glycoprotein I antibodies detection in a large cohort of Chinese patients with antiphospholipid syndrome[J].International Journal of Laboratory Hematology,2020,42(2):206-213.
收稿日期:2023-03-24;修回日期:2023-04-06
編辑/杜帆

