The value of prognostic markers for pediatric trauma patients
Cansu Durak, Ebru Guney Sahin, Yasar Yusuf Can, Alican Sarisaltik, Kubra Boydag Guvenc
1Department of Pediatric Intensive Care, Sancaktepe Sehit Prof. Dr. IlhanVarank Training and Research Hospital, Health Science University, Istanbul 34785, Türkiye
2Republic of Türkiye Ministry of Health, Cayirova District Health Directorate, Kocaeli 41420, Türkiye
KEYWORDS: Critical care; Pediatric; Lactate; Procalcitonin; Trauma
INTRODUCTION
Trauma is one of the leading causes of admission to pediatric emergency departments and intensive care units.[1]Mortality over the age of one year old due to pediatric trauma is an important health problem,especially in developing countries.[2]Mortality rates were noted as 40% at the time of the accident, 30% in the early period, and 30% in the late period.Hypoxia,hypovolemia, and severe brain trauma are the leading causes of mortality in pediatric trauma patients in the early period.On the other hand, systemic inflammatory response syndrome (SIRS), multiple organ failure syndrome (MOFS), sepsis, and acute respiratory distress syndrome (ARDS) are the most common causes that increase mortality in the late period.[3]Recently, great strides have been made in addressing the early period,both with injury prevention, and dramatic advances in resuscitation, surgical procedures, and pediatric intensive care medicine.[4,5]However, progress is urgently needed in improving the outcomes of post-traumatic SIRS.
Trauma triggers a strong, immediate systemic inflammatory response as a result of tissue damage,hypotension, hypoxia, cytokine release, and inflammation.The initial injury and the subsequent inflammatory response cause MOFS.[6-8]MOFS unfortunately remains the leading cause of late post-traumatic death.[9]Accurate identification of patients at risk of developing SIRS at an early stage and timely treatment of patients have become very important for the prognosis of patients.These findings lead us to investigate the prognostic role of inflammatory biomarkers with the aim of identifying patients with potentially poor outcomes.Therefore, we conducted this study both to evaluate our experience and to assess the relationship between laboratory parameters and outcomes of pediatric trauma patients.
METHODS
Study population
A retrospective evaluation of 77 pediatric trauma patients who were admitted to the PICU at Sancaktepe Sehit Prof.Dr.IlhanVarank Training and Research Hospital from August 2020 to December 2022 was performed.In our 12-bed PICU, a total of 912 patients were hospitalized and followed up during the study period.Patients with the following were included: age between 1 month and 18 years old; injury mechanisms with traffic accident, or falling; and admission time within 24 h from initial injury.All the trauma patients in this study were admitted to our PICU after their initial evaluation in our emergency department (ED).Patients who died within 24 h after admission, and patients with underlying diseases, including genetic, metabolic,and hepatic disease, other chronic organ dysfunction or detected infectious disease, were excluded from the study.We obtained informed consent from all parents before hospitalization and during all procedures.Clinical Research Ethics Committee approval was received from the hospital (17.06.22 E-46059653-020-552).This study was planned in accordance with the ethical principles of theDeclaration of Helsinki.
Data collection and definition
A detailed form was used for data collection regarding the patient’s age, gender, type of trauma,cause of trauma, length of stay in the PICU, duration of mechanical ventilation, extracorporeal treatment requirement, inotropic treatment, transfusion requirement, laboratory parameters, treatment outcomes,and mortality.The blood sampling data of all cases were measured at almost the same time on admission and the worst value in the first 24 h of admission was recorded.Complete blood count, serum albumin, procalcitonin(PCT), C-reactive protein (CRP) levels, and blood gas analysis on admission were recorded retrospectively.For the calculation of the Pediatric Risk of Mortality III (PRISM III) Score, data from 16 variables regarding temperature, systolic blood pressure, heart rate, partial pressure of arterial oxygen (PaO2), partial pressure of arterial carbon dioxide (PaCO2), glasgow coma score(GCS), pupillary reaction, prothrombin time (PT),activated partial thromboplastin time (APTT), serum creatinine, serum urea nitrogen, serum potassium, blood glucose, serum bicarbonate levels, white blood cell and platelet counts were recorded within 24 h of PICU admission.[10]
Multisystem trauma was defined as injuries to two or more organs in different cavities or damage to internal organs and the musculoskeletal system including the face and pelvis.Causes of death were divided into early and late periods.Early mortality was defined as patients who died from injuries resulting in hypotension, hypoxia, and hypovolemia within the first 72 h.Late mortality was defined as patients who died due to causes such as SIRS,MOFS, sepsis and ARDS after 72 h.
The primary outcome is the mortality in the PICU.The secondary outcomes are the prognostic factors, such as the requirements of continuous renal replacement therapy (CRRT), inotropic agent, therapeutic plasma exchange (TPE), mechanical ventilation, and the length of hospital stay.
Statistical analysis
SPSS statistical software 20.0 for Windows was used for statistical analyses.Numbers, frequencies,ratios, medians, and interquartile range (IQR) values were presented in the descriptive statistics of the data.The distribution of variables was checked by using the Kolmogorov-Smirnov and Shapiro-Wilk tests.During the analysis of quantitative data,t-test and Mann-WhitneyUtest were performed.The Chi-square test was used to compare categorical variables, and Fisher’s exact test was used when chi-square conditions could not be met.PRISM scores, PCT, neutrophil/lymphocyte ratios(NLR), and lactate/albumin ratios (LAR) were further evaluated for their predictive ability for mortality by receiver operating characteristic (ROC) curve analysis.According to the estimated cut-off values, PCT, NLR,and LAR were transformed into binary variables.The relationship between these predictors and prognostic factors were further analyzed.
RESULTS
A total of 77 patients admitted to the PICU due to trauma were included in our study.The median age was 70 (33–157) months, and most of the patients were male(n=53, 67.5%).The median duration of PICU stay was 6(1–11) d.The median PRISM III score was 6 (2–9), and the pediatric trauma score (PTS) was 8 (3–9.5).Invasive mechanical ventilation was required in 37 patients(48.1%), and the median duration of invasive mechanical ventilation was 3 (2–11) d.Inotropic drugs were used in 18 patients (23.4%).TPE and CRRT were performed in 3 patients (3.9%).When evaluated according to the trauma regions, most patients had head or multiple system traumas.The mortality rate due to trauma was 11.1%.Seven patients died in the early period, mainly due to severe traumatic brain injury; while two patients died due to MODS in the late period.One patient with probable brain death had carotid circulation.
According to mortality in the PICU, patients were divided into a survival group (n=68) and a non-survival group (n=9).Patients in the non-survival group presented significantly higher PRISM III and significantly lower PTS scores than those in the survival group (21 vs.5,P<0.001; and -1 vs.9,P<0.001).PCT (P=0.014), LAR(P<0.001) and NLR (P=0.021) were also higher in the non-survival group than in the survival group.The requirements for mechanical ventilation (P=0.001),CRRT (P=0.001), TPE (P=0.035), transfusion of packed red blood cells (P=0.012) and platelet suspension(P=0.001) were significantly higher in the non-survival group (Table 1).While TPE patients required more platelet suspension, there was no statistically significant difference in the need for packed red blood cells.
ROC curves were used to evaluate the predictive ability of mortality with PRISM III score, PCT, LAR,and NLR.According to ROC analysis, cut-off values for PRISM III score, PCT, LAR, and NLR were 18.500(P<0.001), 1.105 (P=0.014), 0.535 (P<0.001), and 3.120 (P=0.021), respectively (Figure 1 and Table 2).The relationship between PCT, LAR and NLR and other prognostic parameters was evaluated regarding the cutoff values.While the requirements for inotropic agents and mechanical ventilation were significant higher in patients with PCT levels above the cut-off values; the requirements for CRRT, inotropic agents, TPE therapy and mechanical ventilation were significant higher in patients with LAR ≥ 0.535 (Tables 3–4).The requirement for CRRT and TPE therapy was also significant higher in patients with NLR ≥ 3.120 (Table 5).

Figure 1.Analysis of receiver operating characteristic (ROC) curve of mortality and biomarkers.PRISM III: Pediatric Risk of Mortality III score.

Table1.Comparison of prognostic factors and laboratory parameters between survivors and non-survivors
DISCUSSION
Trauma is one of the leading causes of morbidity and mortality in childhood.In many different studies, the average age of trauma patients was found to be in a wide range between 17 months and 12 years.[11]Additionally, it supports a male predominance similar to our study.[12]Motor vehicle accidents are the most common cause of injuryrelated death worldwide, followed by falls.[13]However,another study from our country has shown that falls are generally more common than other types of trauma.[11]In our study, the median age was 70 months and the most common cause of injury was falling.In our opinion, this result is related to the fact that young children are more exposed to home accidents such as falling from heights due to their long stay at home during the pandemic period.
The prognosis of severe trauma patients is of great importance, particularly in consideration of increased mortality and morbidity risk.Early prediction of prognosis and providing early treatment may improve outcomes in severe trauma patients.Although recent advances in pediatric critical care, surgical procedures,and resuscitation techniques have positively impacted on the outcomes, the development and application of biomarkers as both predictive and prognostic indicators remains a field of extensive research.
Several biomarkers and scoring systems have been used to predict outcomes, prognosis, and mortality after trauma.The PRISM III score is one of the most widely used scoring systems to predict intensive care outcomes in critically ill pediatric patients.Costa et al[14]reported that the median PRISM score in nonsurvivors was higher(median 8 points, range 4–14) than that in survivors(median 7, range 3–12).The median PRISM III score in our study was 6, whereas in the case of survivors, it was 5, and in the case of non-survivors, it was 21.Our results are in concordance with a study from Brazil in which the PRISM III score in survivors was 7, and in nonsurvivors,it was 15.[14]The PRISM III score has been shown in many studies to be effective in predicting mortality and therefore serves as a useful tool for assessing prognosis in the PICU.
Our study showed that non-survivors required more mechanical ventilation, inotropic agents, packed red blood cell (PRBC) and platelet suspension (PS) transfusion,CRRT, and TPE therapies than survivors.Since these prognostic factors show MOFS developing with many criteria such as respiratory failure, heart failure, renal failure, and acute traumatic coagulopathy, it causes an increase in mortality as stated in many studies.[9,11,15]
The use of NLR is increasing in clinical practice.A high level of NLR often indicates a poor prognosis for critically ill patients.In recent years, the prognosticvalue of the NLR in adult trauma patients has been investigated.A single-center study in Asia showed that NLR was associated with mortality in adult patients with traumatic brain injury.[16]Alimohammadi et al[17]found that an elevated NLR could be a predictor of poor clinical outcomes in children with moderate to severe TBI.Similarly, NLR was significantly higher in nonsurvivors than in survivors in our study.The cut-offvalue was found to be 3.12, lower than the 7.92 value of in the previous research.[18]We also found that NLR was related to CRRT and TPE requirements.
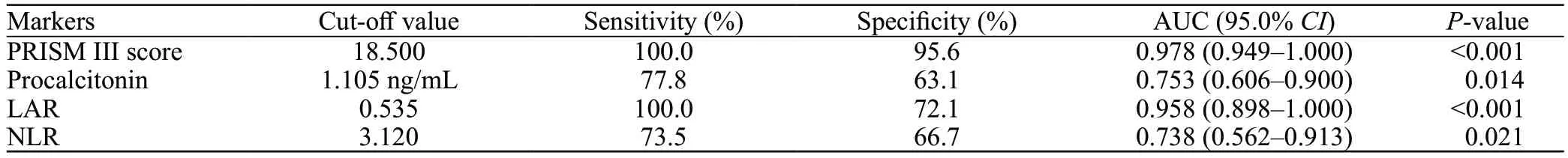
Table 2.Predictive performance of markers on the mortality of pediatric trauma patients based on the ROC curves analysis

Table 3.Relationship between procalcitonin level and prognostic factors
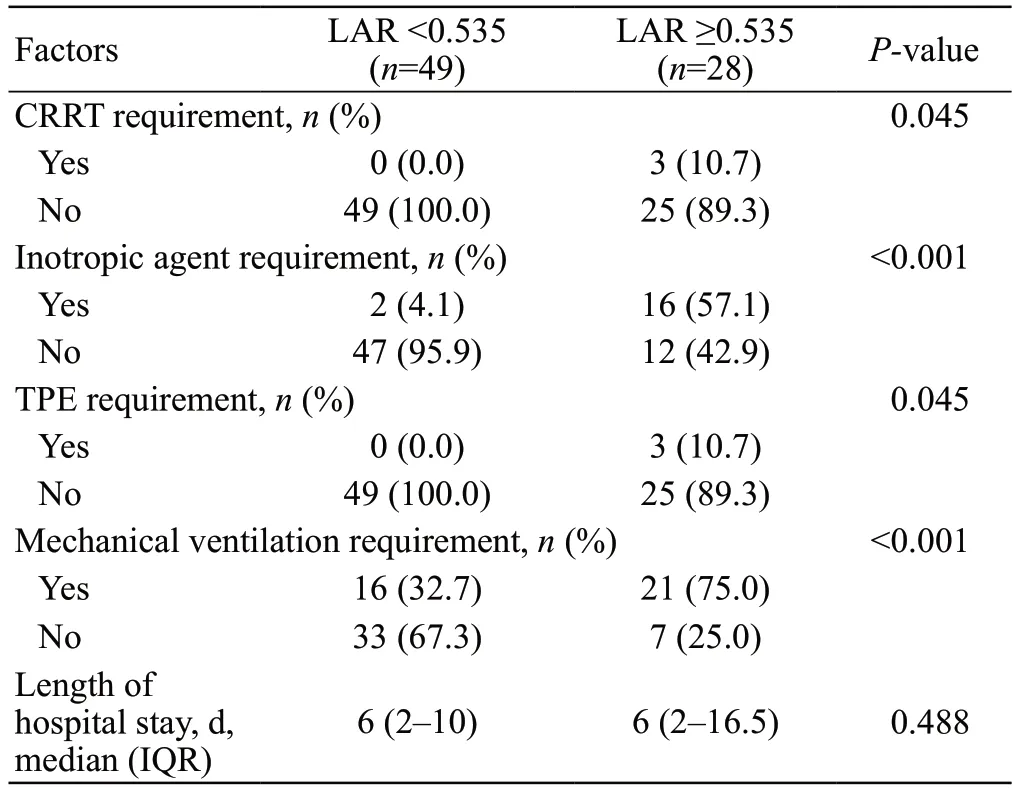
Table 4.Relationship between lactate/albumin ratio and prognostic factors

Table 5.Relationship between neutrophil/lymphocyte ratio and prognostic factors
Numerous biomarkers of post-traumatic inflammation have been investigated.A large number of studies have been conducted on CRP and PCT.Both of them are inflammatory indicators that are widely used in the diagnosis and treatment of acute diseases.In trauma,the initial elevations in PCT levels are transient, and peak approximately 48–72 h before falling, unlike other inflammatory markers such as CRP, which can remain elevated for at least 2 weeks after trauma even in the absence of organ failure or sepsis.Early elevation of PCT is related to the severity of the trauma and the extent of tissue damage.[19,20]Therefore, PCT was found to be more sensitive than CRP in adult trauma patients.[8]However,the use of PCT levels as a prognostic indicator in trauma has not been established in the pediatric population.Xu et al[13]reported that secondary to multiple trauma,PCT levels increased in more pediatric patients, even though leukocyte and CRP levels remained unchanged.However, they found that early rising leukocyte levels and injury severity scores were better than PCT in predicting the mortality of multiple trauma patients in the PICU.In our study, PCT was more sensitive than CRP in trauma patients.With a cut-off level of 1.105 ng/mL,PCT was found to be related to inotropic agents and mechanical ventilation requirements.
Recently, the LAR has been investigated to predict mortality in critically ill patients.Many studies have shown that LAR may be superior to single lactate in predicting mortality, neurological outcomes, and survival in pediatric and adult sepsis patients.[21-24]However, there are limited data on its role as a predictor in pediatric and adult trauma patients.Han et al[25]showed an increase in LAR (odds ratio: 1.618;P=0.028) with a cut-off value of 0.755 in the ROC curve as an independent predictor of MODS development.In our study, the LAR of non-survivors was significantly higher and the cut-off value of LAR was determined to be 0.535.Although logistic regression analysis could not be performed since the sample size of our study was limited, we found that LAR was closely related to other prognostic factors such as the requirement of inotropic agents, mechanical ventilation, CRRT, and TPE.
Limitations
One of the most important limitations is the small number of patients since our study was conducted in a single center.Moreover, our study is a retrospective study.The laboratory parameters could not be recorded simultaneously in all patients, and the worst values in the first 24 h of admission were evaluated.
CONCLUSION
In conclusion, there is insufficient evidence regarding biomarkers for the outcomes of pediatric trauma patients.In our opinion, LAR, PCT, and NLR values in pediatric trauma patients can be used to identify patients at risk of mortality.Further prospective cohort studies with larger sample size would be beneficial.
Funding:The authors have no financial relationships relevant to this article to disclose.
Ethical approval:We obtained informed consent from all parents before hospitalization and during all procedures.Clinical research ethics committee approval was received from the hospital(17.06.22 E-46059653-020-552).
Conflicts of interest:The authors have no conflicts of interest to disclose.
Author contribution:CD takes responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.CD, EGS, and YYC designed the study, planned the concept, and prepared and edited the manuscript.CD and KBS had a role in the literature overview and data analysis.AS contributed to the statistical analysis.All authors contributed to the writing of this paper and have seen and approved the final version.
 World journal of emergency medicine2023年6期
World journal of emergency medicine2023年6期
- World journal of emergency medicine的其它文章
- Tension urinothorax as a reversible cause of cardiac arrest: a case report
- A case of pulmonary mucormycosis presented with cardiac arrest
- Pyopneumothorax caused by Parvimonas micra and Prevotella oralis: a case report
- Hemorrhagic pancreatitis from fenofibrate and metformin toxicity: a case report
- The effect of prophylactic antibiotics in acute upper gastrointestinal bleeding patients in the emergency department
- The effects of hyperbaric oxygen therapy on paroxysmal sympathetic hyperactivity after cardiopulmonary resuscitation: a case series
